To analyze whether the application of Lean techniques to improve the flow of critically ill patients in a health region with its epicenter in the intensive care unit (ICU) of a reference hospital.
DesignObservational study with pre and post intervention analysis.
SettingICU of a reference hospital.
PatientsWe design projects and a value stream map of flow and compared pre and post intervention.
InterventionsWe recorded demographic data, patient transfers by EMS for lack of beds and delay times in the discharge from ICU to ward. Multidisciplinary meetings and perform daily visual panel, with high priority ICU discharge. We promote temporary relocation of critically ill patients in other special areas of the hospital. We performed a professional satisfaction questionnaire with pre and post implementation of process. We make a statistical analysis of pre and post-intervention comparisons.
ResultsWe planned for 2013 and progressively implemented in 2014. Analysis of patients entering the critical process flow (1) evaluate patients who must transfer for lack of beds, focusing on a diagnosis: pre 10/22 vs. 3/21 post (p=.045); (2) analysis of time delay in the discharge from the ICU to ward: 360.8±163.9min in the first period vs. 276.7±149.5 in the second (p=.036); and (3) personal professional satisfaction questionnaire, with 6.6±1.5 points pre vs. 7.5±1.1 in post (p=.001). Analysis of indicators such as the ICU acquired infections, length of ICU stay, the rate of re-admissions and mortality, with no significant differences between the two periods.
ConclusionsThe application of Lean techniques in the critically ill process had a positive impact on improving patient flow within the health region, noting a decrease of transfers outside the region due to lack of beds, reduced delayed discharge from ICU to conventional ward and increased satisfaction of ICU professionals.
Analizar si la aplicación de técnicas «Lean» mejora el flujo de pacientes críticos de una región sanitaria, tomando como epicentro el servicio de medicina intensiva (UCI) del hospital de referencia.
DiseñoEstudio observacional con análisis pre y postintervención.
ÁmbitoUCI del hospital de referencia.
PacientesDiseñamos proyectos y un mapa de flujo y comparamos características pre y postintervención.
IntervencionesRegistramos datos demográficos, de traslados de pacientes por el SEM por falta de camas y los tiempos de demora en la hora de alta de la UCI a planta de hospitalización. Realizamos reuniones multidisciplinarias y panel visual diario, con priorización de altas de UCI. Promovimos la reubicación temporal de pacientes críticos en otras áreas especiales del hospital. Cuestionario de satisfacción profesional con valoración pre y postintervención. Análisis estadístico de las comparaciones pre y postintervención.
ResultadosSe planificó durante 2013 y se implementó de forma progresiva en 2014. Las medidas principales fueron: (1) análisis de la entrada de pacientes al flujo del proceso de críticos, evaluando los pacientes que deben trasladarse por falta de camas, centrados en un diagnóstico y un área: 10/22 pre vs. 3/21 post (p=0,045); (2) análisis del tiempo de demora en la hora de alta de UCI a planta de hospitalización: 360,8±163,9min en el primer periodo vs. 276,7±149,5 en el segundo (p=0,036); y (3) cuestionario de satisfacción profesional personal, con 6,6±1,5 puntos pre vs. 7,5±1,1 en post (p=0,001). Análisis de los indicadores de UCI, como son las infecciones adquiridas, los días de estancia, la tasa de reingresos y la mortalidad, sin diferencias significativas entre ambos periodos.
ConclusionesLa aplicación de técnicas ‘Lean’ en el proceso de críticos tuvo un impacto positivo en la mejora del flujo de pacientes dentro de la región sanitaria, observando una disminución de los traslados fuera de la región por falta de camas, una reducción en la demora del alta de UCI a hospitalización convencional y un aumento de la satisfacción de los profesionales de la UCI de referencia.
In our hospital and in the intensive care unit (ICU), the average occupation rate is over 90%. Since the ICU is a single Unit serving a reference population of 844,000 inhabitants, in some cases not all the critically ill patients corresponding to that population can be admitted to the ICU, and transfer to other ICUs in hospitals located in a different healthcare region is required.
On the other hand, the characteristics inherent to critical patients cause demand to vary greatly depending on the time of year and on the surgical activity in the center. Detailed monitoring of the evolution of the care process is therefore necessary in order to assign the necessary resources, according to time and demand.
Before the start of this study, the care process in our ICU already included activity assessment indicators that generated information on the quality of care of the critically ill (level of infections), costs (pharmacy materials and resources), service (admission and discharge times) and safety (readmission and mortality rates).
In view of the characteristics of our healthcare area, a study project was started in late 2013 on the flow of critical patients in the region, with the designing of a “critical patients process” involving the application of “Lean” techniques to improve and correct the flow of these patients. Lean techniques fundamentally seek to reduce variability within one same process and eliminate superfluous elements that lack added value.1–3 The core document was the development of a value stream map, the epicenter of which was the Department of Intensive Care Medicine of the healthcare region from where all the information and interventions were centralized under the coordination of an intensivist. The principal study hypothesis was that the implementation of Lean techniques could have a positive impact upon a series of measurable parameters of the process. To this effect, the data were recorded, with analysis and comparison of the pre- and post-intervention phases–the intervention basically consisting of implementation of the critical patients process in the healthcare region.
The specific objectives of our study were: (1) to evaluate whether the application of Lean techniques in the ICU and hospital of the healthcare region had a positive impact in reducing patient transfer to other regions because of a lack of ICU beds; (2) to determine whether application of the flow of critical patients in the hospital resulted in a decrease in delay of patient discharge from the ICU to the hospital ward; and (3) to assess the level of satisfaction of the ICU professionals implicated in the critical patients process.
MethodsLean techniques were first applied to the automobile industry, and basically consist of a simple, profound and effective work method designed to increase productive efficiency in all processes, based on the kaizen management philosophy of continuous incremental improvement in time and space, with the aim of eliminating wastefulness. The methodology is characterized by imbuing the employee with a sense of belonging to the team and of participation by being able to contribute ideas for continuous improvement of the process.2 In a first step we define the work setting and scope of the activity. This is a key aspect in order to identify those actions which have a positive impact upon the overall process, not only on one of the services involved in management of the critically ill. In this regard, the problem was studied from a multidisciplinary perspective in late 2013, assessing the different origins and destinations of the patients with which the critical patients process of the hospital works. As reference we used articles in which Lean techniques were applied, particularly in the emergency care setting, with the purpose of ensuring a more agile admission process and reducing the patient waiting times in performing laboratory tests.4 As basic working tool we used the experience in Lean techniques of Virginia Mason Hospital and other similar literature sources as references.5–7
We identified a series of problems which were addressed in order of importance, as assessed in the discussion and analysis group. Lean techniques were then applied with a new design of flow–eliminating wastefulness referred to time and mode, and reallocating the critical patients of the region to different special units within the hospital, such as the Coronary Unit (COU) and postsurgery resuscitation unit (RES), which acted as buffer units in the face of excessive demand. We started implementation of the critical patients process in early 2014. In the conduction of these first actions, the creation of a module managed by means of a visual panel in the ICU–which acted as epicenter–was a key element for coordination of all the professionals involved. Each day, all the personnel members of the ICU participate in a meeting with a maximum duration of 10min in which the state of the process is commented, and the following aspects are discussed and decided upon:
- •
Workload of the Department.
- •
Current capacity and capacity predicted for the next hours.
- •
Anticipated patient admissions and discharges.
- •
Distribution of the personnel in the process.
- •
Relation of the ICU with other services within the same process (COU, RES, emergency care, hospitalization and emergency medical service [EMS]).
- •
Urgent discharge and box cleaning and preparation.
- •
Techniques to be used in the Unit and external complementary tests.
- •
Isolated patients, need for physiotherapy and special techniques.
- •
Other topics of interest (visits, evolution of epidemiological curves).
In a second step, and to study the saturation of the different areas of the hospital and of the healthcare region, we standardized a meeting with the different implicated services. This meeting is coordinated by the process supervisor–in this case an intensivist from the reference ICU–and each service presents its current saturation and expected patient flow (admissions and discharges) for the next 24h. Patients for discharge from the ICU are a priority issue, and maximum agility of the process is sought in this case. The decisions derived from the mentioned meeting are recorded by means of a flowchart that is updated daily, and which also serves as minutes on the meeting.
In order to assess the impact of the actions, we measured the waiting intervals for patient discharge from the ICU to the hospitalization ward in several periods of time. Registry was made of the delay (in min) from the moment of decision of patient discharge to the ward to the moment when transfer was effectively carried out. An evaluation and comparison were made of the critical patients transferred via EMS outside the region due to a lack of beds in our ICU in the pre-intervention and post-intervention period. For this evaluation, and in order to avoid selection bias, we adopted a concrete diagnostic coding system including sepsis and septic shock, and also considered a concrete reference area fully assigned to us–in this case Blanes Hospital (Selva).
A quantitative, 10-point satisfaction questionnaire was administered to the ICU professionals, assessing organizational aspects, interprofessional relations and personal satisfaction, following international standards.5 The scores in turn were compared between a period before and a period after the intervention. Lastly, an analysis was made of the health outcomes of the critical patients of our Department, assessing the two study periods for infections, mean stay, readmissions and mortality.
The Clinical Research Ethics Committee was informed of the study, and in view of the characteristics of the project, the obtainment of informed consent was not considered necessary. Patient confidentiality was guaranteed during the period of the study and in the records.
Quantitative data were reported as the mean and standard deviation, and qualitative data were presented as numbers and percentages. Comparisons were based on the Student's t-test or Mann–Whitney U-test in the case of quantitative parameters, and using the Pearson chi-squared test or Fisher exact test in the case of qualitative variables. Statistical significance was considered for p<0.05. The SPSS® version 12 statistical package (Chicago, IL, USA) was used throughout.
ResultsWe basically conducted an analysis of the demographic findings in the pre-intervention period and compared them with the post-intervention period. No significant differences were found, and the two populations therefore were regarded as homogeneous and comparable. A second evaluated aspect was the number of patients requiring transfer via EMS due to a lack of beds: this situation occurred in 10 patients/22 requests in the pre-intervention period versus in three patients/21 requests in the post-intervention period–the inter-period reduction being statistically significant (p=0.045).
The time of discharge from the ICU to the conventional hospital ward was 16:00±2:43p.m. in the first period versus 14:26±2:29p.m. in the second period, and the delay in effective discharge counting from the time of request of patient discharge was 360.8±163.9min in the first period versus 276.7±149.5min in the second period–the inter-period reduction in delay being statistically significant (p=0.036), with a reduction in waiting time from discharge request to effective transfer to the hospital ward of about 1h and 30min in the post-intervention period.
Comparison of the evolutive outcomes referred to infections acquired in the ICU, i.e., ventilation-associated pneumonia (number of episodes/1000 days of tube), catheter-related urinary tract infection (number of episodes/1000 days of catheter) and catheter-related bacteremia (number of episodes/1000 days of catheter), as well as readmission rate and mortality rate, yielded no statistically significant differences between the pre- and post-intervention periods.
Although implementation of the new methodology in the ICU proved difficult during the first few months, due to a lack of clear understanding among the professionals of the objectives of the change, the use of a daily visual panel displaying the situation of the critical patients and their distribution in the different areas of the region, with a monitor trained in Lean techniques, contributed to improve acceptance of the new methodology. In this regard, the professional satisfaction survey among physicians, nurses, assistant personnel and hospital porters in the ICU revealed a statistically significant improvement in score in all three professional dimensions considered: organization, inter-professional relations and personal satisfaction.
All these data, with the comparative analysis of the two periods and corresponding p-values, are summarized in Table 1.
Characteristics before and after implementation of the Lean techniques.
| Characteristic | Pre-intervention | Post-intervention | p-value |
|---|---|---|---|
| Demographic | |||
| No. patients admitteda | 697 | 691 | – |
| Age, years (SD)a | 61.1 (16.4) | 60.5 (16.9) | 0.122 |
| No. males (%)a | 446 (64.0) | 437 (63.2) | 0.810 |
| APACHE II, points (SD)a | 17.8 (6.9) | 18.4 (7.4) | 0.510 |
| SAPS II, points (SD)a | 36.3 (16.1) | 38.5 (16.3) | 0.481 |
| EMS transfer due to lack of beds | |||
| No. transfers/total requestedb | 10/22 | 3/21 | 0.045 |
| Delay in discharge from ICU to ward | |||
| Delay in minutes (DE)a | 360.8 (163.9) | 276.7 (149.5) | 0.036 |
| Evolutive outcomes in the ICU | |||
| Ventilation-associated pneumoniaa | 7.2 | 5.2 | 0.167 |
| Catheter-related bacteremiaa | 0.95 | 0.54 | 0.211 |
| Catheter-related urinary infectiona | 4.2 | 4.3 | 0.865 |
| Mean stay, daysa | 7.9 | 7.9 | 0.992 |
| Readmissions to ICU, no. (%)b | 16 (2.3) | 15 (2.2) | 0.966 |
| Mortality in ICU, no. (%)b | 125 (18) | 145 (21) | 0.311 |
| Professional satisfaction survey | |||
| Organization, points (SD)a | 6.2 (1.6) | 7.6 (1.2) | 0.001 |
| Interprofessional, points (SD)a | 6.4 (1.5) | 7.3 (1.2) | 0.001 |
| Personal satisfaction, points (SD)a | 6.6 (1.5) | 7.5 (1.1) | 0.001 |
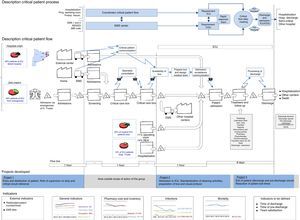
In order to illustrate the flow of critical patients and the components of the process, Fig. 1 shows a working panel reflecting the value stream map of the complete critical patients process. The panel is divided into different parts exhibiting all the elements of the critical patients process, and the principal projects–which are dynamic–are displayed and modified. The health outcomes of each period are also shown and can be compared.
Panel showing the value stream map of the critical patients process. The panel is divided into different parts: the critical patient process is shown at top, while critical patient flow with the updated actual data are shown at bottom. The three projects developed in the period of the study are indicated, with details provided in the text. Finally, the considered health indicators of the critical patients in the ICU are shown.
The present study has shown that Lean techniques designed to improve the flow of critical patients in a healthcare region–with the Department of Intensive Care Medicine of a reference hospital as epicenter–are effective in reducing the number of patients requiring transfer outside the region due to a lack of beds, with temporary reallocation to other special areas within the hospital. In addition, a reduction was observed in the time elapsed from the decision of patient discharge from the ICU to effective transfer to the conventional hospital ward, and improved satisfaction of the ICU professionals with the new working methodology was recorded. Furthermore, no negative effects were observed in relation to critical patient outcomes such as infections acquired in the ICU or the readmission and mortality rates.
Implantation of the critical patients process has largely contributed to find a solution for those critical patients in our healthcare region who previously would have been transferred via EMS to other regions because of a lack of beds. This is a recurrent problem in our healthcare system, and can have a negative impact upon the clinical course of such patients.8
However, improvement of the flow of patients in the course of the process is a long-term project that requires improved synchronization among all the implicated services. In this regard, improvements have been made in certain services of the hospital, and this, combined with changes in the flow of critical patients in the ICU, has resulted in significantly earlier discharge from the ICU to the conventional hospital ward. To our knowledge, this has not been previously reported: we have found only one article describing a reduction in admission time, but in the opposite sense, i.e., patient admission to the ICU from the hospital ward, with application of the “Six Sigma” methodology, which is similar to the Lean techniques described in our study.9
Certainly, the good results obtained with the Lean techniques are conditioned to adequate implication and commitment on the part of the team of professionals in the ICU, the application of protocols and of checklists in all procedures within the process, and the implementation of safe and quality critical care practices.10,11 At present there is a “Lean thinking” trend that aims to transform the way in which healthcare systems operate in developed countries. However, it is also true that this concept cannot be extrapolated to all services, all hospitals, or all countries.3 We believe that these and other improvement strategies should be referred to as “continuous improvement techniques” targeted to all health-related actions, whether encompassed within concrete processes or not, with a gradual tendency to obviate terms such as “Lean” and “Six Sigma”, which are more related to the manufacturing industry.
Our study has a number of limitations, including particularly the fact that it is a single-center observational study, and the lack of previous publications on the application of Lean techniques in critical patients. Furthermore, these techniques are rather inexact and can be used in very diverse ways depending on the setting involved. Consequently, we decided to analyze variables that are easy to measure in the pre- and post-intervention context, though there probably are many other parameters that could also be analyzed, and which possibly might not have such a positive effect as those considered in our study. An aspect to be considered in future may be the impact upon the clinical course of patients who as in our study have been reallocated (“buffer” effect) for a period of time before definitive admission to the ICU of the reference hospital.
There is no doubt that an independent and closed ICU, isolated from the hospital and from the surroundings, is destined to become a thing of the past, with no options for expansion or future perspectives within the current healthcare system. The increasingly popular and modern concept is that of the “ICU without walls”,12 permeable to all that happens in the hospital, and characterized by anticipation of potential critically ill patients through the implementation of telemedicine systems,13 electronic information systems and rapid response teams.14 In this regard, the ICU without walls can immediately deal with problems affecting patients outside the ICU, and can even anticipate possible situations of risk – thereby preventing patients from progressing toward critical conditions.
In conclusion, our study shows that Lean techniques or “continuous improvement techniques” applied to the critical patients process in our setting improve the flow and care of critical patients in the healthcare region, increasing satisfaction among the professionals and exerting no negative effect upon the health outcome measures. This serves to confirm the words of Martin and Gordo15 regarding the activities in the ICU: “It is necessary to maintain a spirit of improvement, targeting effort especially to less developed areas, such as teamwork, improved communication, participation of the patient, or the culture of responsibility and safety”.
Conflict of interestThe authors declare that they have no conflicts of interest.
The authors wish to express their most sincere gratitude to all the professionals of the ICU (physicians, nurses, assistant personnel, hospital porters and administrative personnel), and especially to Guadalupe Garcia and Montse Garcia, who have been fully dedicated to implementation of the critical patients process, with important contributions to the continuous improvement of critical patient care. Thanks are also due to Dr. Vicenç Martinez-Ibañez, who had the initial idea of the project, and to Dr. Gloria Padura and Dr. Joaquim Casanovas, who have contributed to its continuation.
Please cite this article as: Sirvent JM, Gil M, Alvarez T, Martin S, Vila N, Colomer M, et al. Técnicas «Lean» para la mejora del flujo de los pacientes críticos de una región sanitaria con epicentro en el servicio de medicina intensiva de un hospital de referencia. Med Intensiva. 2016;40:266–272.