The optimal blood management after cardiac surgery remains controversial. Moreover, blood transfusions may have an impact on long-term outcomes.
ObjectiveThe aim of this study is to characterize the impact of liberal red blood cell transfusions on Health-Related Quality of life (HRQoL) after cardiac surgery.
MethodsWe studied a cohort of 205 consecutive patients after ICU discharge. Baseline characteristics and clinical data were recorded, and HRQoL was assessed using the EuroQoL-5D instrument, applied 6 months after ICU discharge. A specific question regarding the improvement in the quality of life after the surgical intervention was added to the HRQoL questionnaire. Risk factors related to impaired quality of life were identified using univariate comparisons and multivariate regression techniques.
ResultsThe median (interquartile range, IQR) of transfused red blood cells was 3 (1–4). Among 205 patients, 178 were studied 6 months after discharge. Impairment in at least one dimension of the EuroQoL-5D questionnaire was observed in 120 patients, with an overall score of 0.8 (IQR 0.61–1). The number of red blood cell transfusions was related to an impaired HRQoL (OR 1.17 per additional unit, 95% confidence interval 1.03–1.36, p=0.03), a trend to lower visual analog scale score (coefficient −0.75 per additional unit, 95% confidence interval −1.61 to 0.1, p=0.09) and an absence of improvement in HRQoL after surgery compared to the previous status (OR 1.13, 95% confidence interval 1.03–1.25, p=0.01).
ConclusionsLiberal red blood cell transfusions increase the risk of impaired HRQoL after cardiac surgery.
El manejo óptimo de la sangre después de cirugía cardíaca sigue siendo controvertido.
ObjetivoAnalizar el impacto de la transfusión liberal de concentrado de hematíes (CdH) sobre la calidad de vida relacionada con la salud (CVRS) después de la cirugía cardíaca.
MétodosSe estudió una cohorte de 205 pacientes consecutivos. Se registraron las características basales y los datos clínicos, y se evaluó la CVRS utilizando el EuroQoL-5D, 6 meses después del alta de la UCI. Se añadió una pregunta específica sobre la mejoría de la CVRS tras la cirugía cardiaca. Los factores de riesgo relacionados con la alteración de la CVRS se identificaron mediante el uso de comparaciones univariadas y técnicas de regresión multivariante.
ResultadosLa mediana (rango intercuartílico [IQR]) de los CdH transfundidos fue de 3 (1-4). De 205 pacientes, 178 fueron estudiados 6 meses después del alta, 120 pacientes (67%) mostraron deficiencias en alguna dimensión del cuestionario EuroQoL-5D, con un puntaje general de 0,8 (IQR: 0,61-1). El número de transfusiones de CdH se relacionó con una CVRS deteriorada (OR: 1,17 por unidad adicional; intervalo de confianza del 95%: 1,03-1,36; p=0,03), menor escala analógica visual (coeficiente: −0,75 por unidad adicional, intervalo de confianza del 95%: −1,61-0,1; p=0,09) y una ausencia de mejoría en la CVRS después de la cirugía en comparación con el estado previo (OR: 1,13; intervalo de confianza del 95%: 1,03-1,25; p=0,01).
ConclusiónLa transfusión liberal de CdH aumenta el riesgo de deterioro de la CVRS después de la cirugía cardíaca.
Patients undergoing cardiac surgery often require the administration of red blood cells (RBC) units to maintain hemoglobin to ensure tissue oxygen supply. Although lifesaving, allogeneic RBCs pose their own risks, ranging from febrile reactions to iron overload or severe lung injury among others.1 By these reasons, excessive RBC transfusions must be viewed with caution and perhaps the best practice is to avoid unnecessary transfusions. Several studies have identified a correlation between the RBC transfusion and an increased risk of death after cardiac surgery,2 even after adjustment by the baseline covariates.3 Major bleeding is independently associated with operative mortality in cardiac surgery patients. Preoperative anemia and RBC transfusion are additional independent risk factors for operative mortality that could multiplicate the effects of other factors.4 However, while a recent trial has shown a trend to a better survival with a more liberal transfusion policy (using an hemoglobin level below 9g/dL as cut-off value)5 and evidence from randomized controlled trials in cardiac surgery, refutes findings from observational studies that liberal thresholds for red blood cell transfusion are associated with a substantially increased risk of mortality and morbidity,6 a more recent trial shows that in patients undergoing cardiac surgery, who had a moderate to high risk of death, a restrictive strategy regarding the transfusion of red blood cells was not inferior to a liberal strategy.7 Some studies recommend efforts to save blood in cardiac surgery patients due to the lack of adverse effects of a restrictive strategy.8
Some publications on transfusion and cardiac surgery have shown great variability in the indication of RBC transfusion.9 Therefore, the optimal threshold to trigger the use of these blood products is not known. A restrictive transfusion policy threshold has shown that is safe in most clinical settings and the current blood banking practices of using standard-issue blood are recommended.10
RBC transfusion has been associated with an increase in early morbid outcomes and reduced long-term survival after cardiac surgery, its relationship to functional quality of life after surgery has been less explored.
Given the relationship between RBC transfusion and morbidity, we hypothesized that this factor could also be related to a worse health-related quality of life HRQoL after a cardiac intervention. To study a putative relationship between transfusion and HRQoL, we studied a cohort of patients after major cardiac surgery, collecting clinical data during their hospital stay and their HRQoL 6 months after discharge.
Materials and methodsStudy designThis was a prospective, observational study including 205 consecutive patients admitted to the Hospital Universitario Central de Asturias (Oviedo, Spain) for scheduled cardiac surgery from January to April 2015. Minor interventions were excluded. These minor interventions were extractions of pacemaker leads or removal of infected pacemaker generators. All of them did not require extracorporeal circulation and for which reason they were excluded. In addition, heart transplants were not included due to the intrinsic characteristics of this pathology. The study was approved by the Regional Ethics Committee, and informed consent was obtained from each patient before data collection. All red blood cell units were leukodepleted and stored in an additive solution saline, adenine, glucose and mannitol. Platelets and fresh frozen plasma units were inactivated prior to administration. It is important to note that the indication of transfusion in our unit depends on the responsible physician. A liberal transfusion strategy was followed. The hemoglobin trigger threshold for RBC transfusion was 9g/dL. This observational study was carried out prior to the implementation of a Patient Blood Management (PBM) program in our Hospital. Due to the non-existence of a PBM program, no patient received RBC transfusion prior to the surgical intervention for anemia treatment. The RBC transfusion during the perioperative period includes transfusions of red cells from operation theater to Hospital discharge.
Data collectionAfter inclusion, demographical and clinical data, including comorbidities, diagnoses, type of intervention, analytical results, received therapies and adverse events, were collected in a specific database. The included patients were followed until hospital discharge, and the number of blood products transfused was registered. Patient risk was assessed by the logistic EuroSCORE and EuroSCORE-II systems.
Health-related quality of lifeSix months after hospital discharge, patients were interviewed and the Spanish version of the EuroQoL-5D instrument11 administered. Briefly, this tool evaluates 5 different dimensions (mobility, self-care, usual activities, pain and discomfort, anxiety and depression) with one of three possible answers each one (No impairment, moderate problems, severe problems). An impaired HRQoL was defined as moderate or severe problems in at least one dimension. A final score can be computed after adjustment by predetermined coefficients, as published.11 Finally, a visual analog scale (VAS) is registered, giving a value of 100 to the best achievable quality of life and 0 to the worst.
In addition to the EuroQoL-5D data, a specific question regarding the improvement in the quality of life after the surgical intervention was added, and one out of three possible answers (better, equal or worse) recorded.
Statistical analysisData are presented as median and interquartile range (IQR). Univariate comparisons were done using the non-parametric Mann–Whitney U test or a chi-square test for continuous and categorical variables respectively. Uni- and multivariante (logistic or linear for binary and continuous outcomes, respectively) regression models were performed in order to report unadjusted and adjusted effect sizes. The coefficients of Nagelkerke and Hosmer–Lemeshow were using for measuring the goodness of fit of the linear and binary regression models, respectively. Besides, a propensity score matching procedure was using for dealing with a possible indication bias. The propensity score was computed by logistic regression which included age, preoperative hemoglobin values, functional status and type of surgery and included in the multivariate models.
Odds ratios or coefficients and their 95% confidence intervals were computed for each variable included in these models. All the analyses were done using the R statistical software. A p-value lower than 0.05 was considered significant.
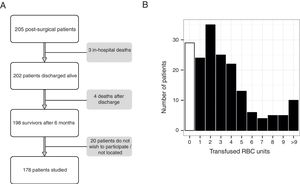
ResultsDuring the study period, 205 patients underwent elective cardiac surgery. Ultimately, 178 out of 205 eligible patients were contacted and studied 6 months after discharge (Fig. 1A). The main characteristics of this sample are shown in Table 1.
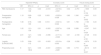
Main characteristics of the simple and univariate comparisons between patients with preserved and impaired health-related quality of life (HRQoL).
| Global N=178 | No HRQoL impairment N=58 | HRQoL impairment N=120 | OR CI (95%) | p | |
|---|---|---|---|---|---|
| Age | 72 [65–78] | 69 [61–76] | 73 [67–78] | 0.95 (0.92–0.98) | 0.013 |
| Female sex (number [%]) | 69 [39] | 13 [22] | 56 [47] | 3.02 (1.48–6.18) | 0.002 |
| BMI (kg/m2) | 28.4 [25.2–31.2] | 28 [25–29.4] | 28.5 [25.4–31.7] | 0.96 (0.90–1.03) | 0.340 |
| Comorbidities (number [%]) | |||||
| Arterial hypertension | 135 (76) | 43 (74) | 92 (76) | 1.14 (0.55–2.36) | 0.712 |
| Pulmonary hypertension | 61 (34) | 23 (40) | 38 (32) | 1.22 (0.73–2.05) | 0.377 |
| Diabetes | 41 (23) | 10 (17) | 31(26) | 1.67 (0.75–3.70) | 0.225 |
| COPD | 20 (11) | 7 (12) | 13 (11) | 0.89 (0.33–2.37) | 0.805 |
| Chronic renal disease | 34 (11) | 7 (12) | 27 (23) | 2.11 (0.86–5.19) | 0.108 |
| NYHA status (number (%) | |||||
| I | 27 (15) | 12 (21) | 15 (13) | 1.00 [Ref.] | – |
| II | 108 (61) | 36 (62) | 72 (60) | 0.62 (0.26–1.47) | 0.283 |
| III | 38 (21) | 10 (17) | 28 (23) | 0.56 (0.24–1.30) | 0.182 |
| IV | 5 (3) | 0 (0) | 5 (4) | – | – |
| Severity | |||||
| EUROSCORE II | 1.7 [1.1–3.0] | 1.5 [1.1–2.5] | 1.7 [1.1–3.3] | 0.96 (0.86–1.07) | 0.622 |
| Logistic EUROSCORE | 5.5 [3.0–7.7] | 4.8 [2.1–6.4] | 6.0 [3.2–8.1] | 0.91 (0.83–0.92) | 0.016 |
| Hemoglobin (g/dl) | |||||
| Preoperative | 13.5 [12.1–14.5] | 13.9 [12.8–15.0] | 13.4 [11.7–14.2] | 1.21 (1.01–1.46) | 0.027 |
| Postoperative | 10.2 [9.5–11.2] | 10.4 [9.7–11.2] | 10.1 [9.4–11.2] | 1.09 (0.85–1.40) | 0.496 |
| Type of surgery (number (%)) | |||||
| On pump aortocoronary bypass | 26 (15) | 7 (12) | 19 (156) | 1.06 (0.55–2.04) | 0.566 |
| Off-pump aortocoronary bypass | 15 (8) | 6 (10) | 9 (7) | 0.72 (0.21–1.77) | 0.482 |
| Aortic valve replacement | 69 (39) | 25 (43) | 44 (37) | 0.73 (0.46–1.14) | 0.515 |
| Mitral valve replacement | 28 (16) | 9 (15) | 19 (16) | 0.80 (0.29–2.19) | 0.852 |
| Aortic root replacement | 12 (7) | 5 (8) | 7 (6) | 0.73 (0.27–2.01) | 0.599 |
| Valvular and coronary surgery | 28 (16) | 6 (10) | 22 (18) | 2.15 (0.95–4.85) | 0.092 |
| Extracorporeal circulation time (min) | 88 (72–114) | 86 (76–111) | 90 (70–119) | 0.98 (0.99–1.01) | 0.995 |
| Aortic cross-clamp time (min) | 73 (57–94) | 72 (63–95) | 74 (56–92) | 1.00 (0.99–1.11) | 0.632 |
| Hemoderivatives | |||||
| RBC units | 3 [1–4] | 2 [1–3] | 3 [2–5] | 0.81 (0.71–0.93) | <0.001 |
| Platelet units | 0 [0–1] | 0 [0–1] | 0 [0–1] | 0.95 (0.69–1.30) | 0.836 |
| FFP units | 0 [0–2] | 0 [0–0] | 0 [0–2] | 0.85 (0.70–1.05) | 0.133 |
| Hospital length of stay | 11 (9–16) | 10 (9–11) | 13 (10–19) | 0.88 (0.82–0.95) | <0.001 |
BMI: body mass index; RBC: red blood cell; FFP: fresh frozen plasma; OR: odds ratio; CI: 95% confidence interval; COPD: Chronic Obstructive Pulmonary Disease; NYHA: New York Heart Association.
The median number of blood transfusions per patient was 3 (IQR 1–4). Twenty-nine patients (16%) did not receive any blood component during hospitalization. The distribution of blood transfusions in the study cohort is shown in Fig. 1B.
Results on HRQoL are depicted in Fig. 2. A substantial proportion of patients (from 15 to 41%) referred moderate to severe problems in each dimension of the EuroQoL-5D instrument (Fig. 2A–E). The median EuroQoL and visual analog scale scores were 0.8 (IQR 0.61–1) and 70 (IQR 50–80) respectively, with similar distributions in both variables (Fig. 2F and G).
Based on these results, the sample was split according to the presence of an impaired HRQoL. Overall, 120 out of 178 patients (67%) reported an abnormal result in at least one of the EuroQoL-5D dimensions. Those with an abnormal HRQOL were older, more commonly women, with an increased risk assessed by the logistic EuroSCORE, showed lower pre-operative hemoglobin levels and received more blood transfusions (Table 1).
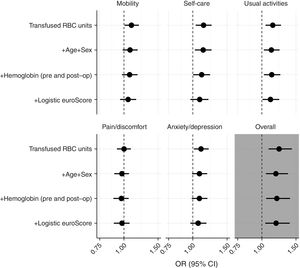
In order to identify the variables related to an impaired HRQoL, different logistic regression models were constructed. In univariate models, the number of RBC units transfused was related to an impairment in the overall result and in each dimension of the EuroQoL-5D tool. Multivariable models, incorporating age, sex, pre- and postoperative hemoglobin levels were tested. The odds ratios of the number of transfused RBC units for each model are shown in Fig. 3. As shown in this figure, the weight of transfused RBC units was higher in the “self care” and “usual activities” dimensions, keeping its statistical significance after adjusting by other covariates.
Impact of the number of red blood cell (RBC) units transfused on each dimension of the EuroQoL-5D instrument (A–E) and in the overall value (F). Plots show the odds ratio per one RBC unit and the 95% confidence interval in each one of the logistic regression models (each one adding all the previous covariates).
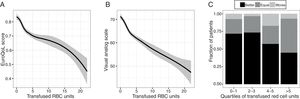
The results of the final models (Table 2), including all the variables with statistically significant differences in the univariate comparisons, demonstrated that age, female sex and transfused RBC units were related to an increased risk of impaired HRQoL after cardiac surgery. The R2 of Nagelkerke coefficient was 0.1964 and Hosmer–Lemeshow test had a p=0.085 for the logistic model. For the lineal models we used the p value of ANOVA and R2 adjusted (R2 adj.=0.052, p=0.025 for EuroQoL score and R2 adj.=0.1195, p=0.025 for VAS) (Table 2). Similarly, transfused RBC units were significantly related to the overall EuroQoL score and the only variable showing a trend to a significant relationship with the visual analog scale value. Fig. 4 shows the relationship between the number of transfused RBC units and the visual analog scale (Fig. 4B) or the final EuroQoL score (Fig. 4A) after adjusting by the other variables of the model.
Predictors of impaired health-related quality of life (HRQoL), overall EuroQoL score (ranging from 0 to 1) and self-reported visual-analog scale (ranging from 100 to 0, corresponding to the best and worst achievable quality of life).
| Impaired HRQoL | EuroQoL score | Visual analog scale | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | Coef | 95% CI | p | Coef | 95% CI | p | |
| RBC transfusions | 1.17 | 1.03–1.36 | 0.03 | −0.010 | −0.019 to −0.001 | 0.04 | −0.751 | −1.605 to 0.104 | 0.09 |
| Preoperative hemoglobin | 1.19 | 0.89–1.59 | 0.23 | 0.003 | −0.022 to 0.028 | 0.83 | 1.540 | −0.851 to 3.932 | 0.21 |
| Postoperative hemoglobin | 1.08 | 0.76–1.55 | 0.66 | 0.010 | −0.021 to 0.042 | 0.51 | 1.738 | −1.180 to 4.655 | 0.24 |
| Age | 1.05 | 1.01–1.09 | 0.01 | −0.003 | −0.007 to 0.000 | 0.08 | 0.088 | −0.247 to 0.424 | 0.61 |
| Female sex | 2.81 | 1.21–6.87 | 0.02 | −0.096 | −0.171 to −0.022 | 0.01 | −2.184 | −9.128 to 4.761 | 0.54 |
| Logistic EUROSCORE | 1.03 | 0.96–1.12 | 0.51 | −0.003 | −0.010 to 0.003 | 0.28 | −0.292 | −0.874 to 0.290 | 0.33 |
| Propensity score | 6 | 0.21–185.2 | 0.30 | −0.041 | −0.362 to −0.281 | 0.80 | 3.719 | −26.13 to 33.57 | 0.81 |
OR: odds ratio; CI: 95% confidence interval; RBC: red blood cells.
Relationship between the number of red blood cell (RBC) units transfused and the overall EUROQOL-5D score (A) and the reported visual analog scale (VAS, panel B) after adjusting by age, sex, pre- and post-operative hemoglobin levels and Euroscore. Panel C shows the distribution of the self-reported change in health-related quality of life before and after the surgical intervention, according to the quartiles of transfused RBCs.
Finally, the self-reported change in HRQoL before and after surgery was recorded. One hundred fifteen patients (65%) reported an improvement compared to their pre-surgical status, whereas 49 (27%) and 14 (8%) reported being equal or worse respectively. Absence of change in HRQoL was related to the number of RBC units transfused (OR 1.13, 95% confidence interval 1.03–1.25, p=0.01) after adjustment by age, sex, pre- and post-operative hemoglobin values and logistic Eursocore. Fig. 4C show these self-reported changes in HRQoL by quartiles of transfused RBC units.
DiscussionDespite advances in perioperative strategies designed to reduce transfusion requirements, the final percentage of patients undergoing cardiac surgery who eventually require some type of transfusion continues to be high, between 45 and 70% depending on the series,12 and there is evidence that it is still on the rise, in large part due to the increase in both, the complexity of the procedures and the associated morbidity of patients.
Our results show that liberal blood transfusion has a significant impact on health-related quality of life after cardiac surgery. This effect persisted after adjustment by age, sex and severity, and no other variables were identified as moderators. Collectively, these results confirm the strong relationship between red blood transfusion and long-term, patient-centered outcomes.
There is an increasing interest on the outcome of critically ill patients after ICU and hospital discharge. ICU stay has been related to an impaired post-ICU functional status, even one year after discharge.13 Neurocognitive and musculoskeletal disorders account for the major part of these poor outcomes, and it has recently been reported that patients after venoarterial-ECMO show physical and psychological difficulties.14 Our results are in line with these findings, showing a major impairment in all the dimensions studied. Although we have no data at later time points, the impact of critical illness on HRQoL may persist even 5 years after discharge.15
A recent prospective study examined the association between red blood cell transfusion and 1-year neurocognitive and disability levels in patients with traumatic brain injury and their results suggest an independent association between RBC Transfusion and unfavorable long-term functional outcomes.16
Blood transfusion has been identified as an adverse prognostic factor in critically ill patients. In this sense, red blood cell transfusions may increase the risk of infections,17 the incidence of ischemic events and the hospital length of stay and costs.18 Moreover, they have been related to an increase in early and late mortality after aortocoronary bypass surgery.19 This observation has been demonstrated even in low-risk cardiac surgery patients.20 These results are in contrast with a recent large trial that failed to demonstrate any benefit of a restrictive strategy regarding red-cells transfusion,5 although in a more recent study the restrictive strategy turned out to be not inferior to a liberal strategy in mortality and post-operative complications.7 Therefore, the optimal management of blood transfusion in the postoperative cardiac patient remains controversial. As described, RBC Transfusion does not improve the clinical outcome in nonbleeding critically ill patients with moderate anemia, that reinforces the current tendency to a restrictive strategy,21 and if long-term consequences are taken into account, our results would support a more conservative approach.
Regarding quality of life, Koch and coworkers performed a large observational analysis in cardiac surgery patients,22 demonstrating a decrease in the performance status in those who receive one or more transfusions. Our work confirms and updates these results. Moreover, we extend this observation, as we show a dose-dependent effect of blood transfusions and study other dimensions of HRQoL such as pain, anxiety or depression.
The reasons for these results are unknown. We have the hypothesis that transfusion-related immunomodulation (TRIM) plays a role in this explanation.23 TRIM likely represents a complicated set of physiologic responses to transfusion, including both proinflammatory and immunosuppressive effects.24
Hyperinflammation and severe immune suppression are associated with poor outcomes from critical illness.25 Although red blood cell concentrates are leukodepleted, TRIM has been related to the presence of residual leukocytes and micro particles resulting from their processing26,27 as well as the existence of free hemoglobin and iron. The older concentrates are more susceptible to alterations in the membrane of the red cells, with cellular apoptosis phenomena, all of them involved in an anomalous immune response.28
Our study faces several limitations derived from its observational nature. First, there is a risk of bias due to unaccounted factors that are responsible for the final outcome. In this sense, blood transfusions could be only a marker of risk, and the final outcome being conditioned by the baseline factors or by the indication itself. We tried to avoid this bias using multivariate models including both the severity and a propensity score as covariates. The results are robust, and the number of red blood cell units retains its significance even after adjustment by the risk of death predicted by the EuroSCORE scale. Moreover, the pre- and post-operative hemoglobin levels did not show a significant relationship with HRQoL, reinforcing the idea that the outcomes were related to the effects of RBC transfusion rather than due to anemia. Lastly, we have no data of HRQoL before the surgical procedure. However, when self-reported change in HRQoL before and after surgery was recorded, the improvement was again related to the number of transfused red cell units.
Identifying the pathogenetic mechanisms responsible for the long-term disabilities could help to apply therapeutic strategies aimed to its correction. In this sense, several interventions such as follow-up programs,29 home-based rehabilitation30 or cognitive rehabilitation31 have failed to improve these long-term outcomes. Although the association between blood transfusion and quality of life reported by our study and others does not mean causality, the impact of a restrictive use of red blood cells on quality of life could be explored. Additionally, politransfused patients constitute a high-risk population in which specific measurements could be applied with a higher probability of success. Finally, a restrictive strategy regarding RBC transfusion based on recent studies should be taken into account, especially in avoidable transfusions, in stable patients.
ConclusionsThe results shown, demonstrate that liberal blood transfusions are related to a high risk of impaired quality of life after cardiac surgery, even after adjusting by confounding factors. These findings should be considered to decide the optimal management of blood products in this setting and could help to identify patients with a high risk of sequels after ICU stay.
FundingGMA is the recipient of a grant from Instituto de Salud Carlos III (INT15-002).
Conflict of interestsThe authors declare no conflict of interests.