The aim of this study is to describe the results of Spanish ICUs in ETHICUS II study.
DesignPlanned substudy of patients from ETHICUS II study.
Setting12 Spanish ICU.
Patients or participantsPatients admitted to Spanish ICU who died or in whom a limitation of life-sustaining treatment (LLST) was decided during a recruitment period of 6 months.
InterventionsFollow-up of patients was performed until discharge from the ICU and 2 months after the decision of LLST or death.
Main variables of interestDemographic characteristics, clinical profile, type of decision of LLST, time and form in which it was adopted. Patients were classified into 4 categories according to the ETHICUS II study protocol: withholding or withdrawing life-sustaining therapy, active shortening of the dying process, failed cardiopulmonary resuscitation and patients with brain death.
ResultsA total of 795 patients were analyzed; 129 patients died after CPR, 129 developed brain death. LLST was decided in 537 patients, 485 died in the ICU, 90.3%. The mean age was 66.19 years ± 14.36, 63.8% of male patients. In 221 (41%) it was decided to withdraw life-sustaining treatments and in 316 (59%) withholding life-sustaining treatments. Nineteen patients (2.38%) had advance living directives.
ConclusionsThe predominant clinical profile when LTSV was established was male patients over 65 years with mostly cardiovascular comorbidity.
We observed that survival was higher in LLST decisions involving withholding of treatments compared to those in which withdrawal was decided.
Spain has played a leading role in both patient and ICU recruitment participating in this worldwide multicenter study.
Describir los resultados obtenidos en UCI españolas en el estudio ETHICUS II.
DiseñoSubestudio planificado de pacientes del ETHICUS II.
Ámbito12 UCI españolas.
Pacientes o participantesPacientes que fallecieron o en los que se decidió una limitación de tratamiento de soporte vital (LTSV) durante un periodo de reclutamiento de 6 meses.
IntervencionesSe realizó seguimiento hasta el alta de la UCI y 2 meses tras la decisión de LTSV o fallecimiento.
Variables de interés principalesCaracterísticas demográficas, clínicas, tipo de decisión de LTSV. Se clasificaron en 4 categorías: omisión o retirada de tratamientos de soporte, acortar el proceso de morir, resucitación cardiopulmonar ineficaz y muerte cerebral.
ResultadosUn total de 12 UCI participaron en el ETHICUS II. Incluyeron 795 pacientes; 129 fallecieron tras realizarse RCP, 129 desarrollaron muerte encefálica. Se decidió LTSV en 537, fallecieron en UCI 485, el 90,3%. La edad media fue 66,19 años ± 14,36, el 63,8% fueron hombres. En un 41% se decidió retirada de tratamientos de soporte total y en un 59% se procedió a no iniciar medidas. Diecinueve pacientes (2,38%) disponían de documento de voluntades vitales anticipadas.
ConclusionesEl perfil clínico predominante cuando se estableció una LTSV fue el de pacientes varones mayores de 65 años con comorbilidad mayoritariamente cardiovascular.
La supervivencia fue mayor en las decisiones de LTSV que comprendían la omisión de tratamientos respecto a aquellas en las que se decidió la retirada.
España ha ocupado un papel destacado en este estudio multicéntrico de ámbito mundial.
Decisions on the limitation of life support therapy (LLST) form part of routine practice in the Intensive Care Unit (ICU). Such decisions are complex and are debated within the professional care teams when considering the futility of both the applied treatments and those that may be added to critical patient care. LLST is defined as the withholding (omission) or withdrawal of those measures which in the concrete situation of the patient are considered by the care team to be futile. The difficulty of some of these judgments of futility is explained by the prognostic uncertainty inherent to clinical practice. Such uncertainty is combated based on the best possible knowledge of the clinical facts, as determined from the scientific evidence, physical examination, evolutive monitoring of the response to treatments, and complementary tests. Clinical practice always requires professionals to base themselves on clinical facts and also on the values of both the patients and the healthcare organization and society as a whole. For decades, the specialty of Intensive Care Medicine has placed a special focus on the development of documents intended to help professionals in the end-of-life decision-making process — promoting responsible clinical ethics capable of ensuring the best possible treatments and care for patients.1–3 As in all clinical interventions, proportionality in maintaining or introducing treatments should be the goal of clinicians in order not to fall into therapeutic obstinacy. It is, therefore, necessary to document clinical experience in decision-making referred to LLST in order to share knowledge and cast light onto a process that is difficult to carry out but which forms part of the daily activity in the ICU. In the year 2003, the data of the largest study up to that time on the real practice of LLST in 37 ICUs from 17 European countries were published4: the ETHICUS study. More than 15 years later, the data corresponding to the ETHICUS II study have been published,5,6 with greater Spanish participation than in the initial ETHICUS study, which reflects the changes there have been in the end-of-life decision-making process worldwide concerning the situation at the start of the century. The present study describes the end-of-life decision-making process in Spanish ICUs and analyzes the results concerning the rest of the countries participating in the ETHICUS II study.
Patients and methodsA planned sub-study was made of the patients admitted to the Spanish ICUs participating in the worldwide ETHICUS II study — a prospective observational trial involving 199 ICUs from 36 countries with the consecutive inclusion of patients admitted to adult ICUs who died or in whom LLST decisions had been made. The recruitment period covered 6 months from 1 September 2015 to 30 September 2016. The patients included in the present study were recruited in Spanish ICUs and were followed up until discharge, two months after the LLST decision, or death. The data corresponding to the Spanish participants were entered by the local investigators of the Spanish ICUs in the study case report forms, and the information was forwarded to the Spanish national ETHICUS II study coordinator for analysis. Before the recruitment period, the questionnaires and case report forms were translated into Spanish, and the Spanish participation was coordinated by the Bioethics Working Group of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]).
The study variables were: age, gender, medical history, clinical characteristics, diagnosis upon admission to the ICU, type of LLST decision and the moment in which the decision was made, participation of the patient and/or relatives, and the existence of advance living directives or patient wishes in the case of patients able to make decisions regarding their health condition. The patients were divided into four categories according to the ETHICUS II study protocol: withholding or withdrawing life-sustaining therapy, active shortening of the dying process, failed cardiopulmonary resuscitation, and patients with brain death.
The statistical analysis was performed by a non-clinical statistician who had managed the Spanish database, using the SPSS version 26 statistical package. Categorical variables were reported as frequencies and percentages, while continuous variables were reported as the median and interquartile range (IQR). Comparative analyses between groups were carried out with the Wilcoxon–Mann–Whitney U-test or chi-square test (χ2). Approval from the local Research Ethics Committee was obtained in all the participating Spanish centers.
ResultsA total of 795 patients from 12 participating Spanish ICUs – 8 belonging to tertiary hospitals and four to secondary hospitals – were analyzed during the study period (Fig. 1). These individuals represented 15.1% of the total patients admitted to intensive care in the course of the study period. Spain was one of the countries with the greatest representation in terms of patient recruitment in the ETHICUS II study (Fig. 2). A total of 129 patients died following advanced cardiopulmonary resuscitation (CPR), and 129 suffered brain death. The group of patients in which LLST was decided comprised 537 individuals, of which 485 died in the ICU (90.3%).
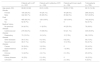
The decision to withhold life-sustaining therapy was more frequent than the decision to withdraw such therapy. In some cases, both decisions overlapped, since different invasive treatments were involved. These were cases in which the decision was made to withdraw measures that had already been introduced, as well as to not start other life-sustaining therapeutic measures. In 455 patients the decision was made not to start such measures, and in 314 the decision was made to withdraw measures that had already been implemented. Table 1 shows the clinical characteristics of the study population, and the reasons for admission are reported in Table 2.
Clinical characteristics of the study population.
| Patients with LLST (n = 537) | Patients with ineffective CPR (n = 129) | Patients with brain death (n = 129) | Total patients (n = 795) | |
|---|---|---|---|---|
| Age (years, SD) | 68.68 (12.62) | 63.5 (14.55) | 58.52 (17.52) | 66.19 (14.36) |
| Gender | ||||
| Female | 195 (36.3%) | 44 (34.1%) | 49 (38.0%) | 288 (36.2%) |
| Male | 342 (63.7%) | 85 (65.9%) | 80 (62.0%) | 507 (63.8%) |
| Died | ||||
| Yes | 485 (90.3%) | 129 (100%) | 129 (100%) | 743 (93.3%) |
| No | 52 (9.7%) | 0 | 0 | 52 (6.7%) |
| Medical history | ||||
| No previous disease | 24 (4.5%) | 11 (8.5%) | 43 (33.3%) | 78 (9.8%) |
| Cardiovascular disease | 279 (52.0%) | 73 (56.6%) | 53 (41.1%) | 405 (50.9%) |
| Respiratory disease | 70 (13.0%) | 18 (14%) | 10 (7.8%) | 98 (12.3%) |
| Other diseases | 39 (7.3%) | 9 (7.0%) | 8 (6.2%) | 56 (7.0%) |
| Neuromuscular disease | 38 (7.1%) | 5 (3.9%) | 10 (7.8%) | 53 (6.7%) |
| Cancer | 30 (5.6%) | 3 (2.3%) | 0 | 33 (4.2%) |
| Gastrointestinal disease | 27 (5%) | 2 (1.6%) | 1 (0.8%) | 30 (3.8%) |
| Immune diseases | 14 (2.6%) | 4 (3.1%) | 2 (1.6%) | 20 (2.5%) |
| Kidney disease | 16 (3%) | 2 (1.6%) | 0 | 18 (2.3%) |
| Unknown | 0 | 2 (1.6%) | 2 (1.6%) | 4 (0.5%) |
LLST: limitation of life support treatments; CPR: advanced cardiopulmonary resuscitation.
Reasons for admission.
| Reason for admission to ICU | Patients with LLST (n = 537) | Patients with ineffective CPR (n = 129) | Patients with brain death (n = 129) | Total patients (n = 795) |
|---|---|---|---|---|
| Neurological | 103 (19.2%) | 9 (7.0%) | 87 (67.4%) | 109 (25.0) |
| Cardiovascular | 96 (17.9%) | 54 (41.9%) | 9 (7.0%) | 159 (20.0%) |
| Respiratory | 126 (23.5%) | 25 (19.4%) | 4 (3.1%) | 155 (19.5%) |
| Surgical | 83 (15.5%) | 18 (14.0) | 7 (5.4%) | 108 (13.6%) |
| Sepsis | 67 (12.5%) | 13 (10.1%) | 1 (0.8%) | 81 (10.2%) |
| Gastrointestinal | 33 (6.1%) | 4 (3.1%) | 0 | 37 (4.7%) |
| Traumatologic | 12 (2.2%) | 2 (1.6%) | 20 (15.5%) | 34 (4.3%) |
| Metabolic | 7 (1.3%) | 2 (1.6%) | 1 (0.8%) | 10 (1.3%) |
| Miscellaneous | 6 (1.1%) | 2 (1.6%) | 0 | 8 (1.0%) |
| Hematological | 4 (0.7%) | 0 | 0 | 4 (0.5%) |
LLST: limitation of life support treatments; CPR: advanced cardiopulmonary resuscitation.
In the group of patients in which the clinical decision of LLST was made, total withdrawal of the life-sustaining therapeutic measures was decided in 41% of the cases, and in 59% the decision was made not to start such measures as these were considered by the professionals as being futile.
In none of the decisions regarding LLST was there disagreement on the part of the relatives of the patients once they had been informed about the clinical decision made. Nineteen patients (2.38%) had documented advance living directives, even if these implied the rejection of treatments, which is different from clinical decisions referred to LLST. The mean ICU stay was 10.75 ± 22.55 days, and the mean time from admission to the ICU to the decision referred to LLST was 8.81 ± 16.13 days. The interval between the decision referred to LLST and patient death was 3.62 ± 13.27 days, which was similar to the time interval between the decision referred to LLST and discharge from the ICU among the patients who survived (3.24 ± 9.32 days).
We recorded differences in the survival curves by analyzing the time between the first decision referred to LLST and patient death (Fig. 3). The withdrawal of life-sustaining therapeutic measures was associated with greater mortality than the withholding of such measures. The logistic regression analysis in the group of patients with LLST showed age (OR = 1.047, CI 1.017–1.077) and the type of LLST decision (withdraw versus withhold) (OR = 4.05, CI 2.12–7.738) to be significantly associated to mortality. The rest of the variables were discarded by the model.
DiscussionThe present study describes the real-life clinical practice in the Spanish ICUs participating in an international study of great impact in the field of clinical bioethics in intensive care. With over 700 analyzed patients, it reports on how the clinical decisions referred to end-of-life care are made in the ICU. The analysis of the clinical characteristics of the patients in which LLST decisions were made describes a predominant profile in the form of a male under 70 years of age with a mainly cardiovascular disease history. This observation coincides with the data from other published studies that have shown the existence of comorbidities before admission to the ICU to be related to LLST decisions,7,8 with the main reasons for admission being respiratory, cardiovascular and neurological conditions. On examining the data from other countries participating in the ETHICUS II study, no marked differences were observed regarding the decisions referred to LLST.6 The existence of advance living directives in our country was anecdotal, though this does not mean that such directives do not have to be consulted in all patients who are unable to decide at the time of admission to the ICU. The Spanish patient cohort recorded the lowest mortality rate in southern Europe — the figures in the rest of the countries in the region being close to 100%. Nevertheless, the mortality rate was 10% higher than the global average of the study, which was 83.4%. This finding must be interpreted with caution, and reflects variability in terms of both the admission criteria used and in decision making referred to the admitted patients.
In the ETHICUS II study, most of the countries reported a mortality of over 80%, with lower figures in European countries such as Switzerland, Denmark and The Netherlands. In turn, Australia, New Zealand and the United States documented mortality rates of about 75%, which differs greatly from the most extreme mortality figure in the study, reported by China (45.9%).5 On examining the literature, marked variability in LLST decisions is observed,9,10 as already documented in the ETHICUS study,4–6 with significant cultural, religious and legal differences among countries. Nevertheless, in clinical practice, it is important to note that differences in decision-making are also commonly seen within the same country.11 Indeed, such differences are even observed at a more local level within each team, where there are different opinions that evidence both difficulty in decision-making and the need to continue working on the importance of team ethical debate.3,12
It is important to mention that decisions referred to LLST do not necessarily imply the death of the patient — in contrast to other end-of-life scenarios such as euthanasia, where death occurs in all cases. LLST decisions seek to avoid futile treatments, and this explains why one out of every 5 patients in which LLST was decided in the ETHICUS II trial did not die.6 We found survival to be greater in the case of LLST decisions involving the withholding of life-sustaining measures than in those cases where the withdrawal of invasive measures was decided. This is an observation of great importance, evidencing that an invasive treatment is not always the best therapeutic option, and that in some patients – due to their clinical situation and profile – the adoption of conservative treatment strategies may be more effective than invasive treatments. In addition, palliative care is an established reality in ICUs, being applied on an individualized basis within a multidisciplinary context.14,15
The limitation of life support treatment not only combats therapeutic obstinacy in each concrete case but also addresses the values of the healthcare organization referred to concepts such as opportunity cost. This aspect is poorly developed in the argumentation of clinicians, out of concern that it might not be adequately understood. However, we have recently experienced it during the worst months of the SARS-CoV-2 pandemic, when resources were lacking and difficult decisions had to be made, considering the greatest possibilities of recovery.13 A percentage of patients with LLST survive at discharge from the ICU, particularly those in whom the decision has been made to not start life-sustaining measures. This highlights that LLST is a routine practice in Spanish ICUs, with prognostic outcomes dependent upon the type of LLST decision made.
The present study has strengths and limitations. Despite the important participation of Spanish ICUs, the studied population was small in comparison with that of the total national ICUs, and there may have been bias on the part of the participating units due to interest in aspects related to the end-of-life decision-making process. Likewise, no detailed analysis was made of patient severity and organ failure at the time of the decision referred to LLST. On the other hand, as a strength of the study, mention must be made of the fact that the data were collected in the context of an international study with quality control, and were analyzed and published globally, ensuring the quality of the information. In this regard, the present study is one of the largest prospective series in Spanish ICUs.
Financial supportNone.
Author contributionsCharles Sprung and Alexander Avidan are the main coordinators of the study at the international level: ETHICUS II. They designed the project and facilitated the database corresponding to the patients recruited in Spain for analysis. They have approved the preparation of the manuscript and its submission for publication.
Ángel Estella is the national coordinator of the ETHICUS II study in Spain. He is the principal investigator of this sub-study and has participated in data collection, designing of the database, the selection of centers, and in Spanish coordination of the study. He has participated in the drafting of the manuscript and is the corresponding authors of the article.
Carolina Lagares has carried out the statistical analysis.
Mari Cruz Martin has contributed to the drafting of the manuscript and review of the final version.
All the authors have participated in patient recruitment and completion of the case report forms, and have approved the final version of the manuscript.
Conflicts of interestThe authors declare that they have no conflicts of interest.