Patients admitted to the intensive care unit (ICU) due to acute decompensated pulmonary hypertension (ADPH) have a high in-hospital mortality. Hospital survivors usually have a troublesome clinical course after discharge, and long-term outcomes of ADPH survivors have been scarcely described and are largely unknown.1
To test the hypothesis that patients who survived an ADPH episode and were discharged from ICU have a worse long-term survival compared to ambulatory patients without previous ICU admission due to ADPH, we conducted a retrospective multicenter cohort study including adults with pulmonary hypertension (PH) groups 1 and non-surgical group 4. Study period was from January 2014 until January 2019 and was conducted in two large teaching hospitals in Brazil (two medical ICUs and one cardiovascular ICU). The local Institutional Review Board approved the study on May 10, 2019 (3.317.990) and waived need for informed consent.
Clinical, hemodynamic, and laboratory data were collected from electronic medical records, from the most recent PH clinic visit in the last six months for the ambulatory group and from last visit previous to ICU admission in the ICU group. The criteria for ICU admission was unplanned admission due to ADPH, defined by acute right heart failure with low cardiac output and elevated RV filling pressures, requiring inotropes, vasopressors or other life-sustaining therapies. If a patient had more than one ICU admission, only the first admission was considered.2,3 Time zero for survival analysis was the day of ICU discharge for ICU group and for ambulatory group was the day of last visit at the PH clinic.
Propensity scores (PS) were estimated using logistic regression and used to match patients based on exposure (ICU admission) and outcome (two-year survival) on 1:1 ratio.4,5 Patients were matched to eight confounders: age, PH group, gender, European Society of Cardiology/ European Respiratory Society (ESC/ERS) PH risk assessment, New York Heart Association functional class (NYHA-FC), brain natriuretic peptide (BNP), six-minute walk test (6MWT) and Charlson comorbidity index. ESC/ERS PH risk assessment classification was calculated using a simplified version of the risk assessment strategy proposed by the ESC/ERS PH guidelines, using the following variables: NYHA-FC, BNP, 6MWT, right atrial pressure (RAP) or cardiac index (CI).6,7 More information about methods provided in the supplemental material.
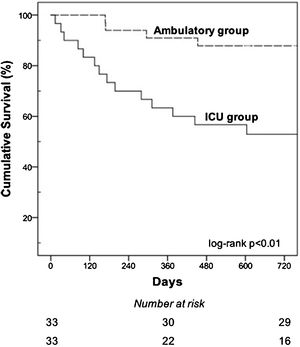
Pairs were matched by greedy nearest neighbor using calipers of width equal to 0.2 of the standard deviation of the logit of the logistic regression.8 One and two-year survival rates were presented on a Kaplan–Meier curve and compared by a log-rank test, and the hazard ratios were calculated by a Cox proportional hazard model.
Clinical features of unmatched and matched patients are shown in Table 1 and additional detailed information is provided in the supplementary material. A total of 46 patients required ICU admission (ICU group) and 62 did not (ambulatory group) during the study period. ICU group had a worse baseline NYHA-FC, higher BNP levels and lower 6MWT compared with ambulatory group (p<0.05 for all comparisons, using chi-square or Mann–Whitney).
Characteristics of patients that required ICU admission compared to patients with no previous ICU admission, depicted for both unmatched and matched samples during the study period.
| Variables | Unmatched sample | Matched sample | ||||||
|---|---|---|---|---|---|---|---|---|
| ICU admission (n=46) | No ICU admission (n=62) | P | ASMD | ICU admission (n=33) | No ICU admission (n=33) | P | ASMD | |
| Age (years) | 41 (35–47) | 44 (38–55) | 0.17 | 0.25 | 43 (34–56) | 48 (38–58) | 0.56 | 0.10 |
| Female, n (%) | 35 (76.1) | 53 (85.1) | 0.22 | 0.24 | 29 (87.9) | 27 (81.8) | 0.73 | 0.17 |
| PH group, n (%) | 0.82 | 0.06 | 0.81 | 0.13 | ||||
| PAH | 33 (71.7) | 46 (74.2) | 25 (75.8) | 23 (69.7) | ||||
| CTEPH | 13 (28.3) | 16 (25.8) | 8 (24.2) | 10 (30.3) | ||||
| PH Risk, n (%) | 0.10 | 0.43 | 0.67 | 0.21 | ||||
| Low | 6 (13.0) | 19 (30.6) | 6 (18.2) | 7 (21.2) | ||||
| Intermediate | 34 (73.9) | 37 (59.7) | 24 (72.7) | 21 (63.6) | ||||
| High | 6 (13.1) | 6 (9.7) | 3 (9.1) | 5 (15.2) | ||||
| FC-NYHA, n (%) | <0.01 | 0.66 | 0.60 | 0.19 | ||||
| I-II | 11 (23.9) | 35 (56.5) | 10 (30.3) | 13 (39.4) | ||||
| III-IV | 35 (76.1) | 27 (43.5) | 23 (69.7) | 20 (60.6) | ||||
| 6MWT (meters) | 366 (300–434) | 410 (338–492) | 0.04 | 0.51 | 373 (274–426) | 388 (327–415) | 0.91 | 0.02 |
| BNP (pg/mL) | 356 (198–436) | 124 (53–250) | <0.01 | 0.62 | 227 (111–313) | 145 (99–251) | 0.40 | 0.19 |
| Charlson Index, n (%) | 0.33 | 0.20 | 0.80 | 0.12 | ||||
| 0−1 | 29 (63.0) | 33 (53.2) | 21 (63.6) | 19 (57.6) | ||||
| ≥ 2 | 17 (37.0) | 29 (46.8) | 12 (36.4) | 14 (42.4) | ||||
Categorical and continuous data are presented as frequencies (percentages) and median (25–75% interquartile range), respectively. ICU=intensive care unit, ASMD=absolute standardized mean difference, PH=pulmonary hypertension; PAH=pulmonary arterial hypertension, CTEPH=chronic thromboembolic pulmonary hypertension, PH Risk=European Society of Cardiology/ European Respiratory Society (ESC/ERS) risk assessment, FC-NYHA=New York Heart Association functional class, 6MWT=six-minute walk test, BNP=brain natriuretic peptide at last visit in the clinic.
After matching balance, all variables had an absolute standardized mean difference (ASMD)<0.25, indicating a negligible difference between groups regarding confounders variables.9 Additionally, a high overlap in the PS distribution of ICU group and ambulatory group was observed by side-by-side boxplots corroborating the good matching (Fig. S1).
In the matched sample we compared 33 patients in the ICU group with 33 patients in the ambulatory group. One-year survival of ICU group was lower compared with ambulatory patients (66.7% vs. 90.9%, log rank P<0.01). The two-year survival in the ICU group was lower compared with the ambulatory group (48.5% vs 87.9%, respectively; P<0.01) (Fig. 1). ICU admission due to ADPH was associated with higher one and two-year mortality. Hazard ratio (HR) of 4.64 (95% CI 1.29–16.67; P=0.02) for one-year mortality, and HR 4.96 (95% CI 1.63–15.11; P<0.05) for two-year mortality.
Kaplan-Meier curves showing the cumulative probabilities of survival in the ICU group compared with ambulatory group during the study period. Patients admitted to the ICU had a 1- and 2-year survival rates of 66.7% and 48.5%, respectively, compared with 90.9% and 87.9% in the no ICU group (log-rank test p<0.01 for both comparisons).
To determine the robustness of the primary analysis, we performed a sensitivity analysis using multivariable Cox regression for one-year and two-years mortality including the propensity score and the PH-targeted therapy (no therapy, monotherapy, double therapy or triple therapy) as variables. In this analysis, ICU admission had a HR 5.27 (95% CI 1.43–19.41; P=0.01) for one-year mortality, and HR 6.55 (95% CI 2.07–20.72; P<0.01) for two-year mortality. The sensitivity analysis indicates that results are robust, and ICU admission is associated with lower long-term survival in this population with similar baseline severity of PH.
Decreased long-term survival after ICU discharge was also reported in previous studies with patients admitted due to ADPH. Our 1-year survival rate after ICU discharge was close to the 65% reported by Campo et al.10 Tejwani et al. reports a 2-year survival rate of 40% in a similar population.1 This suggest our findings are consistent with previous publications.
Need of ICU admission reflects the severity of an acute illness, but could also be a marker of deteriorating PH rather than a factor causing further decline in an individual's health status. History of ADPH requiring ICU admission should be regarded as a “red flag” to alert physicians to high-risk patients for worse long-term outcomes.
Due to the rarity of this condition, large prospective cohorts and randomized clinical trials would be time and resource consuming. Propensity score matching attempts to simulate randomization of subjects as occurs in randomized controlled trials, but it can be limited by bias due to unmeasured or hidden confounders, sensitivity analysis cannot determine if such a bias exists.
The main finding of our study is that in patients with PH group 1 and 4, those discharged from hospital after an ICU admission due to ADPH have a lower one and two-year survival compared with a matched group of patients without previous ICU admission with similar baseline severity of PH, age, gender, comorbidities and PH-targeted therapy. This important prognostic information can be used for discharge planning and patient counseling. Larger prospective studies are needed to determine definitively the long-term outcomes of patients with ADPH.
FundingThe authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Conflict of interestThe authors declare no conflict of interest.
The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.