
Edited by: Rosario Amaya Villar - Unidad de Cuidados Intensivos, Hospital Universitario Virgen del Rocio, Sevilla, España
Last update: December 2023
More infoBarotrauma, defined as tissue damage caused by a pressure gradient between a non-ventilated body cavity and the surrounding air or fluid, is a frequent complication in patients with acute respiratory distress syndrome (ARDS).1
It has recently been evidenced that COVID-19 pneumonia is associated with respiratory failure and ARDS, which may require invasive mechanical ventilation (IMV) in the more serious cases. It has been seen that ARDS COVID-19 patients requiring IMV have a higher incidence of barotrauma than patients with ARDS due to other etiologies,2 even with the use of protective ventilation strategies.3
Barotrauma can manifest as pneumothorax (PTX), pneumomediastinum (PMD) or subcutaneous emphysema.3 In an attempt to predict the risk of PTX/PMD in ARDS COVID-19 patients requiring IMV, use has been made of the Macklin effect, described as a lineal accumulation of air adjacent to the bronchovascular sheath in the lung parenchyma window of the thoracic CT scan, as an early radiological predictor4 allowing the selection of patients who are more likely to develop this complication.
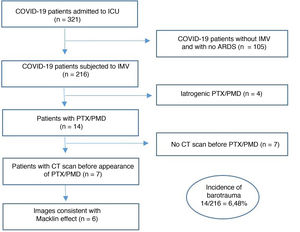
We report the incidence of barotrauma in our Intensive Care Unit (ICU) of Hospital de Mataró (Mataró, Spain) and the number of patients with PTX/PMD in which the Macklin effect was observed in the lung parenchyma window of a thoracic CT scan performed before the first radiological evidence of the disorder (Fig. 1).
A retrospective analysis was made of all the patients admitted to our ICU due to COVID-19 from 1 March 2020 to 31 October 2021, subjected to IMV and who developed PTX/PMD. We excluded cases of iatrogenic barotrauma, patients without IMV during admission, and subjects with no previous thoracic CT scan prior to the first radiological evidence of barotrauma (Fig. 1). Of the 321 patients admitted to our ICU, 216 (67.2%) required IMV, and of these, 14 (6.48%) presented PTX/PMD during their clinical course. Of the 14 patients with PTX/PMD, only 7 (50%) had a previous thoracic CT scan prior to the first radiological evidence of PTX/PMD that allowed evaluation of the presence of the Macklin effect. In 6 of these 7 patients (85.7%), we found images consistent with the Macklin effect in the lung parenchyma window of a thoracic CT scan performed days before the appearance of barotrauma (Fig. 2).
Macklin effect in a COVID-19 patient with ARDS subjected to IMV. The lung parenchyma window of the thoracic CT scan [a] shows a lineal accumulation of air adjacent to the bronchovascular sheath of the left upper lung lobe (the black arrow indicates the Macklin effect). [b] Appearance of pneumothorax days later.
As limitations of this study, mention must be made of the limited sample size involved, the need for an experienced radiologist, and the obtainment of an early thoracic CT scan allowing evaluation of the presence of the Macklin effect in order to be able to estimate the risk and vulnerability of these patients.
We confirm that the Macklin effect was a good early radiological predictor of the development of PTX/PMD in our ARDS COVID-19 patients requiring IMV, supporting the high specificity (95.6%) and sensitivity (89.2%) reported in other studies.4 In COVID-19 patients subjected to IMV and who suffer respiratory worsening, with evidence of the Macklin effect in a basal thoracic CT scan, we should continue to apply protective ventilation strategies and moreover perform a control thoracic CT scan or conventional thoracic radiographic study (conditioned to availability) in order to discard the appearance of barotrauma as the cause of such worsening. On the basis of the above, we recommend an early thoracic CT scan at the time of respiratory failure and admission to the ICU, in order to assess the presence of the Macklin effect, with the aim of adjusting the ventilatory strategies to minimize the appearance of PTX/PMD as a complication, in view of the high mortality rate (60%) observed in patients with barotrauma and associated ARDS due to COVID-19.5
Ethical particularsThe present study was approved by the Clinical Research Ethics Committee of Hospital de Mataró on 17 June 2022 (Reference: CEIm 01/22).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Financial supportNone.







![Macklin effect in a COVID-19 patient with ARDS subjected to IMV. The lung parenchyma window of the thoracic CT scan [a] shows a lineal accumulation of air adjacent to the bronchovascular sheath of the left upper lung lobe (the black arrow indicates the Macklin effect). [b] Appearance of pneumothorax days later.](https://static.elsevier.es/multimedia/21735727/0000004700000004/v1_202303262126/S2173572722002314/v1_202303262126/en/main.assets/thumbnail/gr2.jpeg?xkr=1dZuESKpnCAWr3yCSGZ24A==)


