Edited by: Alberto García-Salido - Pediatric Intensive Care Unit, Hospital Infantil Universitario Niño Jesús, Madrid, Spain
Last update: May 2024
More infoTo reduce radiation exposure in newborns admitted due respiratory distress based on the implementation of lung ultrasound (LUS).
DesignQuality improvement (QI), prospective, before-after, pilot study.
SettingThird level neonatal intensive care unit (NICU) level with 25-bed and 1800 deliveries/year.
PatientsInclusion criteria were neonates admitted with respiratory distress.
InterventionsAfter a theoretical and practical LUS training a new protocol was approved and introduced to the unit were LUS was the first-line image. To study the effect of the intervention we compare two 6-month periods: group 1, with the previous chest X-ray (CXR)-protocol (CXR as the first diagnostic technique) vs. group 2, once LUS-protocol had been implemented.
Main variables of interestThe main QI measures were the total exposure to radiation. Secondary QI were to evaluate if the LUS protocol modified the clinical evolution as well as the frequency of complications.
Results122 patients were included. The number of CXR was inferior in group 2 (group 1: 2 CXR (IQR 1–3) vs. Group 2: 0 (IQR 0–1), p<0.001), as well as had lower median radiation per baby which received at least one CXR: 56 iGy (IQR 32–90) vs. 30 iGy (IQR 30–32), p<0.001. Respiratory support was similar in both groups, with lower duration of non-invasive mechanical ventilation and oxygen duration the second group (p<0.05). No differences regarding respiratory development complications, length of stay and mortality were found.
ConclusionsThe introduction of LUS protocol in unit decreases the exposure radiation in infants without side effects.
Reducir la exposición a la radiación en neonatos ingresados por distrés respiratorio mediante implementación de la ecografía pulmonar (EP).
DiseñoEstudio piloto, prospectivo, anterior-posterior, mejoría de la calidad.
Ámbito Unidad de cuidados intensivos neonatal (UCIN) de tercer nivel con 25 camas y 1800 partos/anuales.
PacientesCriterio de inclusión neonatos con distrés respiratorio.
IntervencionesDespués de una formación teórico-práctica en EP un nuevo protocolo fue implementado y aprobado siendo la EP la primera técnica de imagen. Para estudiar el efecto de la intervención comparamos dos períodos de 6 meses: grupo 1, con el protocolo de radiografía de tórax (RTX) (RTX primera técnica diagnóstica) vs. grupo 2, una vez implementado el protocolo de EP.
Variables de interésLa principal variable de interés fue la exposición total a la radiación. Las secundarias fueron la evolución clínica y la frecuencia de complicaciones.
ResultadosSe incluyeron 122 pacientes. El número de RTX fue inferior en el grupo 2 (grupo 1: 2 RTX [RIQ 1-3] vs. grupo 2: 0 [RIQ 0-1], p<0,001), con una menor dosis de radiación media por cada paciente que recibió al menos una RTX: 56 iGy (RIQ 32-90) vs. 30 iGy (RIQ 30-32), p<0,001. El soporte respiratorio fue similar en ambos grupos, con menor duración de la ventilación no invasiva y oxigenoterapia en el segundo grupo (p< 0,05). No hubo diferencias en el desarrollo de complicaciones respiratorias, días de ingreso o mortalidad.
ConclusionesLa introducción de un protocolo de EP en una unidad disminuye la exposición a la radiación sin efectos secundarios.
Term and premature infants admitted to the neonatal intensive care unit (NICU) due respiratory distress are frequently exposed to radiation for diagnostic imaging. Several studies have examined cumulative grade ionizing radiation exposure including both conventional1,2 and digital imaging techniques3 in this population. The immaturity of these patients with a long life expectancy places them at high risk for delayed radiation-induced malignancies compared to later age periods.4 Due to the improvement in neonatal management, there is an increasing interest in the long term evolution of the premature babies and the effect of the higher dose of ionizing radiations during their NICU income. Lung ultrasound (LUS) has emerged in recent years as a point-of care radiation-free tool, easy and fast to perform, repeatable, harmless to the patient and does not require transport.5
Several studies have focused on the use of LUS to help to identify the aetiology of different neonatal respiratory distress disorders in hospitals with a high degree of LUS training and experience,6–8 but there are few data regarding the implementation of LUS protocol in hospitals without previous LUS expertise and the impact to reduce radiation exposure without secondary effects on patient's care.9
In the present study we followed a Plan-Do-Study-Act cycle to develop and test the quality improvement (QI) intervention of the Integration of LUS as a first image technique for newborn's admitted to a NICU due to respiratory distress following a neonatologist training and implementation of LUS protocol.
Patients and methodsThis was a prospective interventional study performed in a NICU from April-2020 to April-2021. Inclusion criteria were newborns with respiratory distress in the NICU. Exclusion criteria were complex congenital malformations.
A LUS protocol was implemented in the NICU Hospital in October 2020 after a QI intervention. It is a 25-bed NICU with 1800 deliveries/year with special interest in respiratory care and research, but without previous standard LUS training.
The primary QI was to evaluate the impact of LUS implementation on the exposure to CXR and the amount of total radiation to newborns.
Secondary QI were to evaluate if the LUS protocol modified the clinical evolution (the duration of invasive and/or non-invasive ventilation, duration of O2 therapy and ventilator-free days), as well as the frequency of complications (bronchopulmonary dysplasia rate, pneumothorax, or mortality).
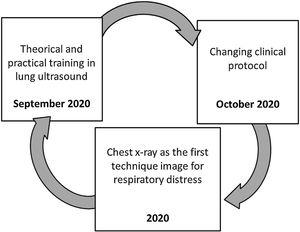
Fig. 1 represents the pathway of the quality improvement project according to the Plan-Do-Study-Act cycle.10 The process was started in September 2020 when LUS training was introduced in our NICU. Later on October 2020 there was a change in the clinical protocol being LUS adopted as the first-line image technique for patients with respiratory distress.
According to the current dosing protocol by the Radiology Department, the CXR dose entrance was 28, 30 and 32 iGy for neonates less than 1500g, 1500–2500g and more than 2500g, respectively.
Senior consultant neonatologists (SCN) received a theoretical and practical LUS training sessions based on a 2-day e-learning and practical course in September 2020. First SCN took an e-learning coursed of interactives internet-based modules. Theoretical lectures (6h) included a combination of text, photos, and movies on newborn's LUS. The practical training part (6h) was carried out with the SCN performing bedside LUS while formally supervised by SCN trained in pulmonary ultrasound with more than 10 years of LUS experience (40–50 lungs scans per month).
A 15-MHz linear probe was used to perform the exams. Once the new protocol was approved by the NICU staff and introduced in October 2020, a Plan-Do-Study-Act cycle was followed to develop and test the QI intervention of the integration of LUS as the first-line image for term and preterm babies admitted to the NICU with respiratory distress. In case the attended clinician had doubts about the LUS examination, a chest X-ray (CXR) was performed. To study the effect of the intervention we compare two 6-month periods: group 1, with the previous CXR-protocol (CXR as the first diagnostic technique) vs. group 2, once LUS-protocol had been implemented.
Patient data were taken in real-time from patient's file or NICU monitoring system being anonymously recorded in a secured Spreadsheet. No images were used for the study. The variables collected included general clinical data of the patients and the respiratory support required in the NICU (need for invasive mechanical ventilation, non-invasive mechanical ventilation, high-flow nasal cannula, the total length of oxygen therapy, and the ventilator-free days). Ventilator-free days were calculated as the number of days in the NICU without invasive mechanical ventilation, within the first 28 days of life; this number is zero for patients who died in the NICU. Complications were registered, such as bronchopulmonary dysplasia and pneumothorax, and also the length of stay (LOS) in NICU and mortality, considered as any death occurring during the NICU admission.
The study was carried out in accordance with the Declaration of Helsinki. Study was approved by the local ethic committee (PI-20-325). Parents received information about the project upon NICU admission and signed informed consent was obtained. The revised Standards for Quality Improvement Reporting Excellence (SQUIRE2) guidelines were followed through the project.
The statistical analyses were performed using SPSS® 26.0. Categorical variables were expressed as frequency (percentage) and compared using the chi-squared test or Fisher's exact test, as needed. Continuous variables were expressed as median (interquartile range) and compared using the Mann–Whitney U test. A value of p<0.05 was considered statistically significant.
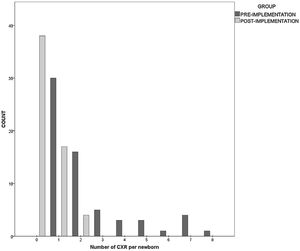
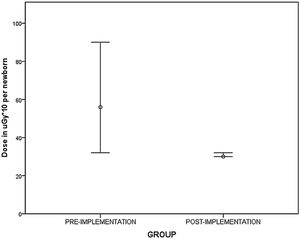
ResultsA total of 122 newborns were included: 63 in group 1 and 59 in group 2. Sixty-five (53.2) were males and the median gestational age was 36.1 (33.1–38.9). Seventy-one (58.2%) were preterm. There were no differences with regards the baseline data as it is shown in Table 1. In group 1, 100% of patients received at least one CXR, while in group 2, only 35.6% (p<0.001). The number of CXR was inferior in group 2 (group 1: 2 CXR (IQR 1–3) vs. group 2: 0 (IQR 0–1), p<0.001), as well as had lower median radiation per baby which received at least one CXR: 56 iGy (IQR 32–90) vs. 30 iGy (IQR 30–32), p<0.001. Fig. 2 represents number of CXR per patients and Fig. 3 represents the dose of radiation per newborns in both groups.
Newborn baseline data.
| Variables | Total (n=122) | Group 1 (n=63) | Group 2 (n=59) | p-Value |
|---|---|---|---|---|
| Gender (male) | 65 (53.2) | 33 (52.3) | 32 (54.2) | 0.193 |
| Weight in grams | 2405 (1810–3230) | 2395 (1717–3065) | 2500 (1863–3470) | 0.248 |
| Gestational age | 36.1 (33.1–38.9) | 35.6 (32.5–38.6) | 36.3 (33.4–38.7) | 0.358 |
| Preterm | 71 (58.2) | 39 (61.9) | 32 (54.2) | 0.391 |
| On call admission | 71 (58.2) | 36 (57.1) | 35 (59.3) | 0.807 |
| 5′ Apgar score | 7 (6–8) | 7 (6–9) | 8 (7–9) | 0.003 |
| 10′ Apgar score | 9 (8–9) | 9 (8–9) | 9 (8–9) | 0.185 |
| Antenatal steroids | 52 (42.6) | 26 (41.3) | 26 (44.1) | 0.755 |
| Complete antenatal steroids | 31 (58.5) | 14 (53.8) | 17 (63) | 0.501 |
| Caesarean delivery | 60 (49.2) | 28 (44.4) | 32 (54.2) | 0.280 |
| Confirmed sepsis | 7 (5.8) | 4 (6.3) | 3 (5.2) | 0.546 |
| Antibiotics in first 24h | 57 (46.7) | 31 (49.2) | 26 (44.1) | 0.570 |
Categorical values expressed as total number as percentage. Continuous values expressed as median (IQR). On call admission: admission during nighttime or weekends.
Respiratory support was similar in both groups, with only statistically significant differences with respect the duration of non-invasive mechanical ventilation and the oxygen duration, both lower in group 2. This may related to less need for MV in group 2. Table 2 includes the comparison of respiratory support according to the group. Fig. 4 shows the comparison of patients regarding the number of CXR per patient and the need for mechanical ventilation. Statistically significant differences were observed between those patients who did not required mechanical ventilation, with lower number of CXR in the group 2. There were no differences regarding the development of complications (bronchopulmonary dysplasia rate, pneumothorax), length of stay in NICU and mortality, as it is shown in Table 3.
Newborn respiratory support.
| Variables | Total (n=122) | Group 1 (n=63) | Group 2 (n=59) | p-Value |
|---|---|---|---|---|
| No CXR | 38 (31.1) | 0 (0) | 38 (64.4) | <0.001 |
| Total CXR | 1 (0–2) | 2 (1–3) | 0 (0–1) | <0.001 |
| LUS | 67 (54.9) | 8 (12.7) | 59 (100) | <0.001 |
| MV | 12 (9.8) | 10 (15.9) | 2 (3.4) | 0.031 |
| MV hours | 24 (15–54) | 20 (10–70) | 27 (24–30) | 0.813 |
| PEEP | 6 (6–6) | 6 (6–6.8) | 6 (6–6) | 0.102 |
| FiO2 | 25 (21–25) | 25 (21–25.5) | 25 (21–25) | 0.294 |
| Surfactant | 11 (9) | 8 (12.7) | 3 (5.1) | 0.208 |
| Surfactant <3h | 8 (6.6) | 6 (9.5) | 2 (3.4) | 0.275 |
| NIV | 120 (98.4) | 61 (96.8) | 59 (100) | 0.496 |
| NIV hours | 28 (18–60) | 58 (26–82) | 20 (12–34) | <0.001 |
| HFNC | 64 (52.5) | 39 (61.9) | 25 (42.4) | 0.031 |
| HFNC hours | 60 (48–168) | 72 (48–192) | 54 (36–110) | 0.211 |
| Total O2 hours | 10 (1–68) | 36 (6.5–89) | 5 (0–12) | <0.001 |
| Ventilator-free days | 23.8 (9.3–27.3) | 20.2 (0.4–27.6) | 25.4 (23.8–27) | 0.722 |
| SNAPPE-II | 2 (1–3) | 2 (1–3) | 2 (1–3) | 0.862 |
| CRIB-II | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.819 |
Categorical values expressed as total number as percentage. Continuous values expressed as median (IQR). CXR: Chest X-ray: LUS: Lung ultrasound. MV: Mechanical ventilation. PEEP: Positive end-expiratory pressure. Surfactant <3h. Surfactant administered during the first 3h. NIV: Non-invasive ventilation. HFNC: High flow nasal cannula. SNAPPE-II: Score for Neonatal Acute Physiology Perinatal Extension. CRIB II: Clinical Risk index for babies.
Comparison of the complications according to the group.
| Variables | Total (n=122) | Group 1 (n=63) | Group 2 (n=59) | p-Value |
|---|---|---|---|---|
| BPD | 4 (3.3) | 3 (4.8) | 1 (1.7) | 0.620 |
| Pneumothorax | 3 (2.5) | 1 (1.6) | 2 (3.4) | 0.610 |
| Mortality | 3 (2.5) | 3 (4.8) | 0 (0) | 0.245 |
| LOS | 8 (5–24) | 9 (6.5–21) | 8 (3–24) | 0.166 |
Categorical values expressed as frequency and percentage. BPD: bronchopulmonary dysplasia. LOS: Length of hospital stay.
To our knowledge, this is the first study showing the introduction of LUS protocol in a NICU without previous experience decreases the exposure radiation in both term and preterm infants without problems encountered changing from CXR-protocol to the LUS-based protocol. In addition, we show an improvement in some secondary QI measures such as the oxygen duration.
Our results demonstrate that neonatologist can achieve a good competence in LUS after a 2-day course based on an e-learning and practical course like previous studies have shown.9
After the introduction of routine LUS in our NICU, we found a significant decrease in the number of total CXR, the number of CXR per baby and the mean dose per baby without significant adverse changes to patient morbidity. Interestingly, the number of newborns managed without any CXR rose to 64.4%.
As both study groups were similar in terms of demographics and clinical characteristics and because the NICU consultants were the same, we may say that no other variables may explain the decrease on radiation.
Although there are no studies relating the cancer risk due to radiation exposure in premature babies and there is no recommended safe level of radiation in this population it is well known that in-utero exposure is associated with an increased cancer risk11 being the maximum allowable exposure during pregnancy 1mSV.1,12 None of the patients from our study exceed this dose due the use of digital radiography being the cumulative effective doses from the first period of our study similar to others previously reported.2,13 Another possible concern could be if there is a discrepancy between daytime and night time outcomes as other studies have previously shown due the lack of senior supervision affecting the quality of perinatal care.14,15 This is not the case of LUS as the majority of newborn's admission (58%) befalls during this timetable showing that after a correct and procotolyzed LUS course there should not be concerns about patient safety.
One of the strength of our project is the context in which was developed. This LUS protocol was introduced into a NICU without previous experience in POCUS guidelines but with medical and nurse team with a high degree of training in respiratory care. Therefore, our results may be used in other NICU Settings without experience in LUS showing that it is an effective strategy to minimize CXR and maximize protective shielding.
Previous published papers have shown that e-learning programmes can be used to teach LUS16,17 and the combination of interactive learning concepts and blended activities leads to a skills increase. Moreover e-learning programmes have achieved similar results to classical classroom-based presentations.18 E-learning methods of teaching theoretical knowledge have the advantage of flexibility in terms of the time, place, and pace of the learning activity E-learning methods of teaching theoretical knowledge have the advantage of flexibility in terms of the time, place, and pace of the learning activity.19 We believe our method of integrating an e-learning curriculum has proven to be helpful in the setting of the medical disruption caused by the actual Coronavirus Disease 2019 (COVID-19) pandemic.20 Our work has several limitations. Firstly, it was carried out at in a single centre being the sample size small. Secondly, although the study included premature newborn's there were very few extremely premature's, the ones would be benefit more of a LUS protocol to avoid radiation since are the ones with higher rates of mechanical ventilation or to develop bronchopulmonary dysplasia and necrotizing enterocolitis. Last, as the design of the study was a before-after there may be some inherent variations which cannot be controlled as epidemiologic changes due the COVID pandemic. Although this can not excluded, we believe this a minimal bias as no other protocol changes were made in the unit.
ConclusionsIntroducing the LUS protocol in a NICU without prior experience reduces radiation exposure in both term and preterm infants without negative consequences derived from the switching from the CXR protocol to the LUS-based protocol.
Statement of ethicsThe study was carried out in accordance with the Declaration of Helsinki. Study was approved by the local ethic committee (PI-20-325). Parents received information about the project upon NICU admission and signed informed consent was obtained. The revised Standards for Quality Improvement Reporting Excellence (SQUIRE2) guidelines were followed through the project.
Authors’ contributionsAll the authors contributed equally to the study and the written of the manuscript.
Data availability statementThe data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding sourcesThere was no financial support to do this study, which was conducted with our own resources. No other financial institution was involved in this paper.
Conflict of interestThe author's have no conflicts of interest to declare.