To compile an inventory of information requests prioritized by the family members, to find out which professionals them consider able to respond these requests, and to explore the differences in perception between family members and professionals.
DesignQualitative analysis of content validation and descriptive cross-sectional study.
Scope41 Spanish ICU.
ParticipantsRelatives, physicians and nurses of critical patients.
InterventionFrom an initial list of questions extracted from literature review, physicians, nurses, and relatives of critical patients incorporated issues that they considered not included. After analyzing content validity, a new list was obtained, which was again submitted to the participants’ assessment to evaluate the level of importance that they assigned to each question and which professional they considered appropriate to answer it.
ResultsMost important questions for the relatives: concern about the clinical situation, measures to be taken, prognosis and information. There was a coincidence between relatives and professionals in the priority issues for families. There were significant differences in the importance given to each question: between doctors and relatives (72/82 questions), and between nurses and relatives (66/82 questions) (p<.05). For the relatives, 63% of the questions could be answered by doctors or nurses, 27% preferably by doctors and 10% by nurses.
ConclusionsThe most relevant issues for families were prognosis and severity, but also the need for information. Healthcare professionals tend to underestimate the importance of many of the questions that concern families. Relatives feel that most of their concerns can be resolved either by doctors or nurses.
Elaborar un catálogo de demandas informativas priorizadas por los familiares, conocer qué profesionales consideran estos que pueden responder a estas demandas y explorar las diferencias de criterio entre familiares y profesionales.
DiseñoAnálisis cualitativo de validación de contenido; estudio descriptivo transversal.
ÁmbitoCuarenta y una UCI españolas.
ParticipantesFamiliares, médicos y enfermeras/os de pacientes críticos.
IntervenciónDe un listado inicial de preguntas extraído de revisión de la literatura, médicos, enfermeras/os y familiares de pacientes críticos incorporaron cuestiones que consideraron no incluidas. Tras análisis de validación de contenido, se obtuvo un nuevo listado que fue valorado nuevamente por los participantes para determinar el nivel de importancia que asignaban a cada pregunta y qué profesional consideraban adecuado para responderla.
ResultadosCuestiones más importantes para los familiares: preocupación por la situación clínica, medidas a tomar, pronóstico e información. Existió coincidencia entre familiares y profesionales en las cuestiones prioritarias para las familias. Existieron diferencias significativas en la importancia dada a cada pregunta: entre médicos y familiares (72/82 preguntas) y entre enfermeras/os y familiares (66/82 cuestiones) (p<0,05). Para los familiares, el 63% de las preguntas podrían ser contestadas por médicos o enfermeras/os indistintamente, el 27% preferentemente por los médicos y 10% por las enfermeras/os.
ConclusionesLas cuestiones más relevantes para las familias fueron pronóstico y gravedad, pero también la necesidad de información. Los profesionales sanitarios tendemos a subestimar la importancia de muchas de las cuestiones que preocupan a las familias. Los familiares consideran que la mayoría de sus inquietudes pueden ser resueltas indistintamente por médicos o enfermeras/os.
The fact that most patients assisted at Intensive Care Units (ICU) are unable to communicate themselves makes their families the main speakers in the information process.1 There are multiple studies2–5 that say that the priorities of the families of critically ill patients are information and nearness with the patient and the medical team, being this need for information especially relevant for the families of patients who have passed away or are about to.6 Clear, easy to understand information is the key to go from that initial stage of confusion to a better control of the situation,7 understand the situation of the patient and promote implication during the decision-making process since information provides us with elements that make it easier to choose between this or that option.8
The information process to the families at the ICU can be better. This is what the scientific literature, both in Spain9,10 and worldwide8,11 tells us. Some studies tell us that the difficulties identified during the first decade of the 21st century are still not solved such as the lack of team work, the role of the nursing team that does not know what kind of information they can disclose, or the need for consensus on the contents of the information provided.12,13
These difficulties are very relevant and have a direct impact on the quality of the information process. At the Spanish ICUs, the doctor is the “official” spokesperson.14,15 Information is usually provided once a day15 and at a given time. In a high percentage of cases this information is whether not understood8 or misunderstood.16 Usually, this information is all about technical aspects and issues that the medical team considers relevant, and these aspects may coincide, or not, with the family's preferences or needs. So it comes as no surprise that the families have doubts afterwards and try to solve them with other resources such as asking the nursing team that does not really know what aspects they should really inform on.
In order to be able to solve all these difficulties, it is necessary that the medical team has a certain degree of consensus on what the content of information should be and how different professionals should handle it.17 In this sense, other authors have brought to light some of the questions usually asked by the families of critically ill patients.18 These studies are a good starting point in order to keep digging and specifying the contents of information that families demand. This project tries to contribute to this line of work by elaborating a catalog of informative requests prioritized by the families themselves that backs up the clinical practice. On the one hand, knowing these demands helps the medical team be able to structure the message that will be transmitted to the families, so it can be as meaningful and adequate as possible to them. On the other hand, knowing what professionals, according to the families, can respond to their informative demands will help us define the informative competences of the different professionals that participate in the healthcare process.
Thus, the following goals were set:
- –
Define the main informative demands from the families of patients admitted to ICUs.
- –
Explore the different perceptions of informative demands from families, doctors, and nurses.
- –
Identify who are considered the most adequate professionals when it comes to satisfying each informative demand.
Different methodologies adapted to the different stages of a study were used by combining document analysis, the qualitative analysis of content validation in a first stage, and ultimately, one transversal descriptive study.
SettingMulticenter study of 41 Spanish ICUs with 66 professionals (doctors and nurses in each ICU) who acted as data mining coordinators in their respective units. The field work was conducted during different stages from September 2015 through March 2016.
The study population was ICU personnel (doctors and nurses) and family members or next of kin of patients admitted at that time to the participating ICUs. Non-probability convenience sampling was used and participants were selected based on the following inclusion criteria:
- –
Family member or next of kin who was the main caregiver and who agreed to participate in the study.
- –
Families of patients hospitalized for over 48h.
- –
Nurses with over 6 months of ICU experience.
- –
Doctors with over 6 months of ICU experience.
It was the study coordinators of each center who, after implementing the aforementioned inclusion criteria, selected the study participants (professionals and families).
VariablesThe study variables were aspects and questions posed while reviewing former studies (out of this review only Peigne et al.’s study could be selected),18 and contributions from professionals and families of patients admitted to ICUs during the study period.
ProcedureAfter finishing the recruiting stage at the ICUs and completing the document with the questionnaire from the medical literature that could be included in the ICU informative processes, the study was conducted during several stages.
- -
Stage 1: coordinators provided all participants with a document including an “initial questionnaire”. This list included 21 questions thought to be important for the families according to a former study conducted in France.18
- -
The coordinators picked 20 participants from each unit (10 professionals—doctors and nurses—and 10 family members/next of kin) and they were handed out the list so that each participant could add all those questions they thought had been left out in the list proposed by researchers. The coordinators of each unit entered the questions obtained in their units in a database created to that end.
- -
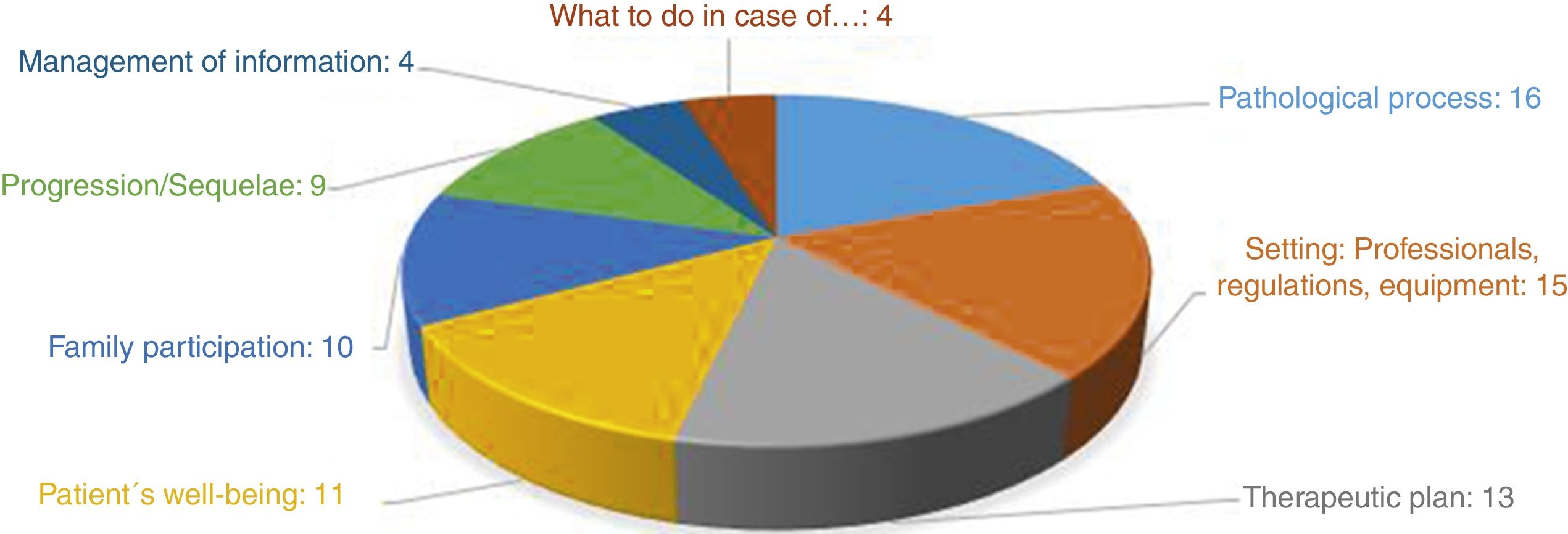
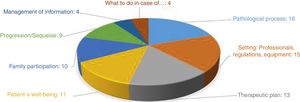
All of the 205 nurses picked added some kind of proposal and out of the 205 doctors picked, 151 (74%) added this or that question. Grouping doctors and nurses, out of the 410 professionals picked, 356 (87%) added some proposal. Out of the 410 family members picked, 203 (50%) did so; the remaining 50% thought their questions were already shown in the initial document. Three researchers independently analyzed the 2095 questions suggested by 205 nurses, 203 family members and 151 doctors, and conducted one qualitative content analysis19 by eliminating redundancies and summarizing those questions that were not generalizable to common cases. This analysis was triangulated to achieve consensus.20 From this consensus, the second document called “final questionnaire” was born including 82 questions grouped into 8 different categories to be taken into consideration during informative processes (Fig. 1).
- -
Stage 2: the “final questionnaire” was re-sent to the coordinators so that professionals and family members could rank the importance of such questions. They were asked to score every question using a Likert scale going from 1 to 9, being 1 “not very important” and 9 “very important”. Also, in this stage they were asked to say who they thought was the most capable professional to answer to each and every one of the 82 questions. They could answer “doctor”, “nurse” or “both”. At this stage, 654 different answers were given; 287 answers came from the families (70%), 190 from the nursing team (92%) and 177 from the doctors (86%). All the answers eventually made it to the general database.
During stage 1 one inductive content analysis was conducted summarizing the 2095 questions received. This summary generated the list of 82 questions used during stage 2. A second content analysis conducted, more analytical this time, grouped the questions into wider topics. Rigor was guaranteed through the triangulation of researchers.
Once the second stage was over all questions were arranged using measures of frequency and central tendency of the score obtained for each and every one of the 82 questions (study variables). Based on the average score obtained in each of the variables studied, both according to families and professionals, one priority list was created.
In order to analyze the differences between the perceptions of families and professionals the non-parametric Mann–Whitney U test for not normally distributed data was used. Statistical significance started at p<0.05.
Then, descriptive statistics through percentages and frequency distribution was used to arrange the different questions based on what professionals the participants thought should answer each question. Such analysis was conducted taking the perspectives of families and professionals into consideration.
Ethical aspectsAll rules and regulations on the protection of personal information were observed and the anonymity and confidentiality of data was guaranteed at all time. Informed consent from all participants was required. The way the information obtained was handled did not allow the identification of the center or the participant involved. The project was approved by the Clinical Research Ethics Committee (CREC) at Málaga, Spain with favorable judgment dated September 25, 2015 and also by each local CRECs.
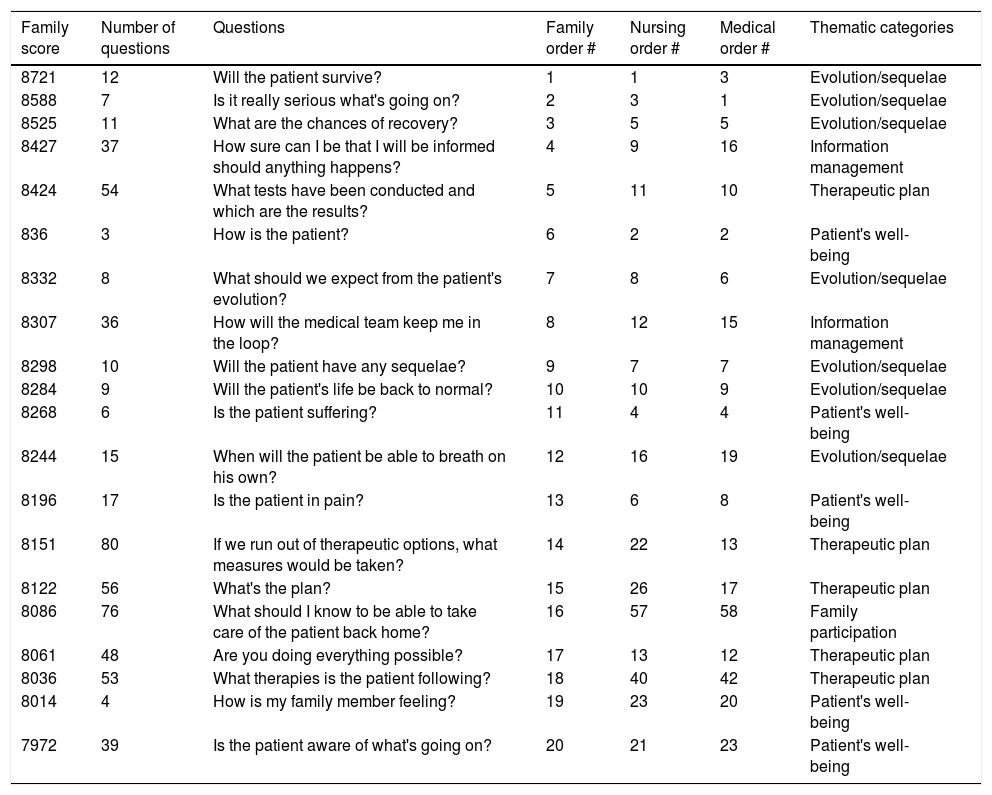
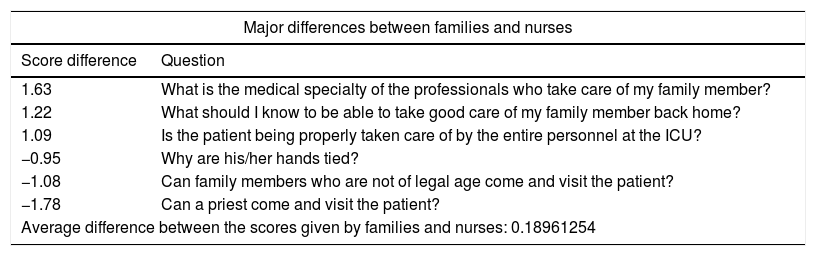
ResultsThe study primary goal was to define the main informative demands from the families of patients admitted to ICUs. Based on the priority order given by them to the 82 questions of the final list, the 20 most important questions deal with the possibilities of survival, the expected progression of the patient, and the possible sequelae (1st, 2nd, 3rd, 7th, 9th, 10th, and 12th in the priority order), the need for information and the way information is handled (4th and 8th), the therapeutic plan (5th, 14th, 15th, 17th, 18th), the patient's well-being (6th, 11th, 13th, 19th, 20th) and family participation (16th). Table 1 (fully available through the additional electronic material [Annex 2]) shows the classification of questions based on the priority order given by the families according to the average score obtained and its association with the following columns that show the priority order given by nurses and doctors, and the type of informative demand each question refers to. When it comes to the study secondary goal (explore the different perceptions of informative demands from families, doctors, and nurses), and even though it is not exactly coincidental with the order of importance given by the families, 85% of the main 20 questions suggested by the families match the 20 most important questions suggested by the doctors, and with 75% of the main questions suggested by the nurses. When comparing the significance score given to every question, there are significant differences (p<0.05) between the scores given by families and doctors in 72 (87.8%) of the 82 questions of the list, being the downward difference the most common one. The same thing happens in 66 questions (80.5%) when the score given by families and nurses is brought to comparison. There are also differences in the assessments made by doctors and nurses, being these differences statistically significant in 53 (64.5%) of the 82 questions. Figure 1 of the additional material shows the importance given to each question by families, nurses, and doctors. The questions where there is a more significant divergence are shown in Table 2.
List of the 20 main questions by order of importance for the families and its association with the order of importance given to these same questions by nurses and doctors.
| Family score | Number of questions | Questions | Family order # | Nursing order # | Medical order # | Thematic categories |
|---|---|---|---|---|---|---|
| 8721 | 12 | Will the patient survive? | 1 | 1 | 3 | Evolution/sequelae |
| 8588 | 7 | Is it really serious what's going on? | 2 | 3 | 1 | Evolution/sequelae |
| 8525 | 11 | What are the chances of recovery? | 3 | 5 | 5 | Evolution/sequelae |
| 8427 | 37 | How sure can I be that I will be informed should anything happens? | 4 | 9 | 16 | Information management |
| 8424 | 54 | What tests have been conducted and which are the results? | 5 | 11 | 10 | Therapeutic plan |
| 836 | 3 | How is the patient? | 6 | 2 | 2 | Patient's well-being |
| 8332 | 8 | What should we expect from the patient's evolution? | 7 | 8 | 6 | Evolution/sequelae |
| 8307 | 36 | How will the medical team keep me in the loop? | 8 | 12 | 15 | Information management |
| 8298 | 10 | Will the patient have any sequelae? | 9 | 7 | 7 | Evolution/sequelae |
| 8284 | 9 | Will the patient's life be back to normal? | 10 | 10 | 9 | Evolution/sequelae |
| 8268 | 6 | Is the patient suffering? | 11 | 4 | 4 | Patient's well-being |
| 8244 | 15 | When will the patient be able to breath on his own? | 12 | 16 | 19 | Evolution/sequelae |
| 8196 | 17 | Is the patient in pain? | 13 | 6 | 8 | Patient's well-being |
| 8151 | 80 | If we run out of therapeutic options, what measures would be taken? | 14 | 22 | 13 | Therapeutic plan |
| 8122 | 56 | What's the plan? | 15 | 26 | 17 | Therapeutic plan |
| 8086 | 76 | What should I know to be able to take care of the patient back home? | 16 | 57 | 58 | Family participation |
| 8061 | 48 | Are you doing everything possible? | 17 | 13 | 12 | Therapeutic plan |
| 8036 | 53 | What therapies is the patient following? | 18 | 40 | 42 | Therapeutic plan |
| 8014 | 4 | How is my family member feeling? | 19 | 23 | 20 | Patient's well-being |
| 7972 | 39 | Is the patient aware of what's going on? | 20 | 21 | 23 | Patient's well-being |
The 1st column shows the average score per question given by the family members. The 2nd and 3rd colums show the number of question in the initial questionnaire and the question as such. Columns 4th, 5th and 6th show the order number by score given for every participant group (in gray the 10 most important questions according to the family members and in salmon color the following 10 questions by order of importance, also according to the family members). The last column shows the thematic category each question is categorized into.
Questionnaire with major score differences between families and nurses, families and doctors, and doctors and nurses.
| Major differences between families and nurses | |
|---|---|
| Score difference | Question |
| 1.63 | What is the medical specialty of the professionals who take care of my family member? |
| 1.22 | What should I know to be able to take good care of my family member back home? |
| 1.09 | Is the patient being properly taken care of by the entire personnel at the ICU? |
| −0.95 | Why are his/her hands tied? |
| −1.08 | Can family members who are not of legal age come and visit the patient? |
| −1.78 | Can a priest come and visit the patient? |
| Average difference between the scores given by families and nurses: 0.18961254 | |
| Major differences between families and doctors | |
|---|---|
| Score difference | Question |
| 2.02 | What is the medical specialty of the professionals who take care of my family member? |
| 1.94 | What should I know to be able to take good care of my family member back home? |
| 1.80 | Is the patient being properly taken care of by the entire personnel at the ICU? |
| −0.50 | Should I call other family members? |
| −0.56 | Can family members who are not of legal age come and visit the patient? |
| −1.09 | Can a priest come and visit the patient? |
| Average difference between the scores given by families and doctors: 0.72334875 | |
| Major differences between nurses and doctors | |
|---|---|
| Score difference | Question |
| 1.43 | What do the alarms mean? |
| 1.25 | What do the data on the monitor really mean? |
| 1.16 | What is the purpose of the tubes and machines the patient is connected to? |
| 0.05 | Is the patient's condition serious? |
| −0.02 | Are there other alternatives somewhere else? |
| −0.24 | Should I call other family members? |
| Average difference between the scores given by nurses and doctors: 0.53373621 | |
When analyzing the priority level attributed to different questions per group, there are significant differences in some cases when the opinion of the families was compared to the opinions of doctors and nurses. In this sense, a coincidental pattern between doctors and nurses was confirmed (Figure 2 of the additional material).
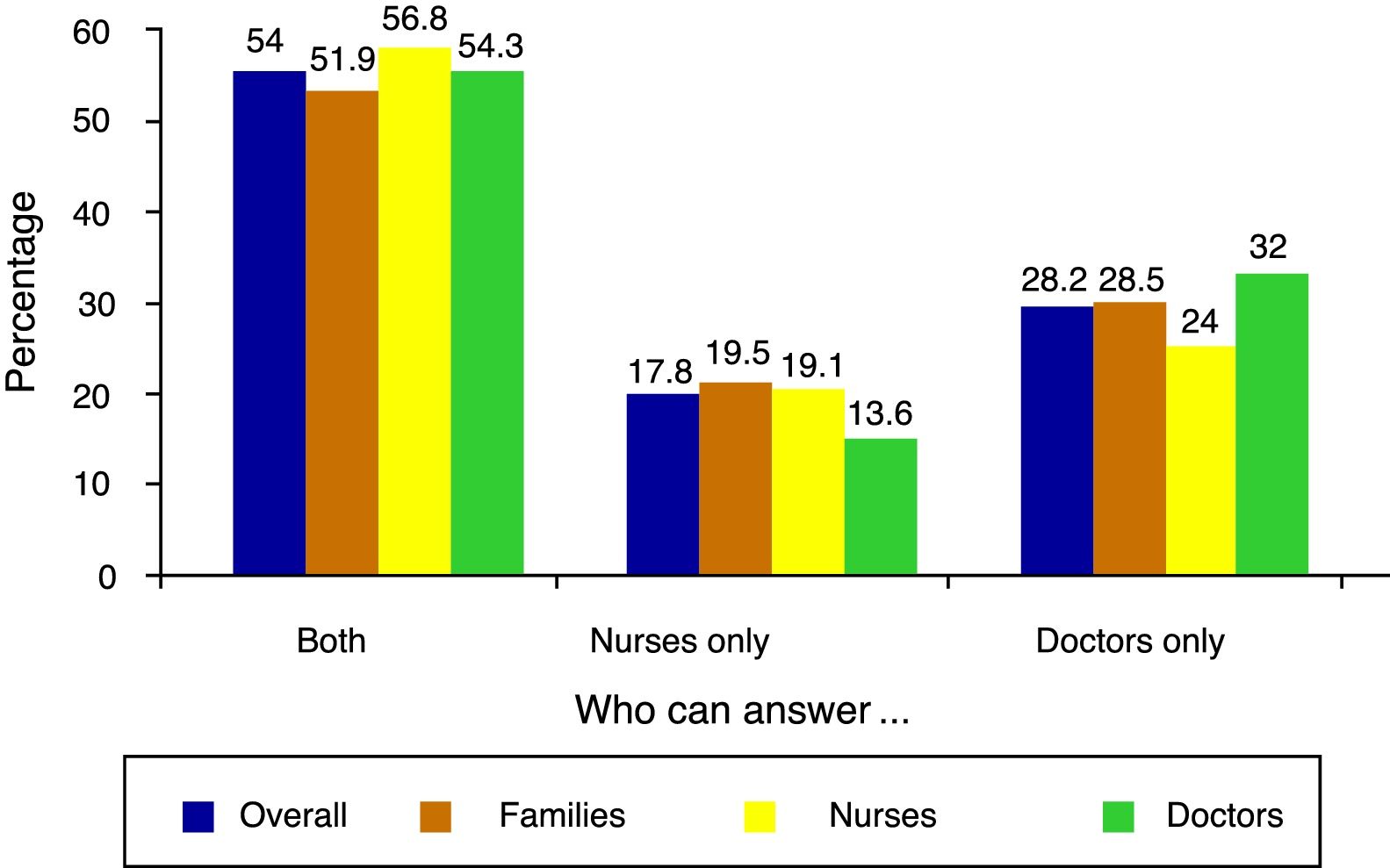
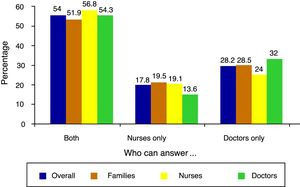
When it comes to the third goal (identify who are considered the most adequate professionals when it comes to satisfying each informative demand), overall, the option “both” was the leading one (54%) followed by “the doctor only” (28.2%) and “the nurse only” (17.8%). Differences can be seen if we take into consideration the opinions of the three groups that responded separately: families, nurses and doctors (Fig. 2).
When analyzing the opinions of the families only (table of the additional material), most participants think that both doctors and nurses can be adequate professionals to answer 52 questions (63.4%). Most families think that it is the treating physician who should solve their doubts in 22 questions (26.8%), ant that it is the treating nurse who should answer 8 questions (9.8%). Of the 20 questions that the families think are the most important ones, they think that 10 of these questions should be answered by doctors, and the remaining 10 by both doctors and nurses alike.
DiscussionOne of the most common aspects in medical literature as a source of dissatisfaction for the families is the perception of poor or bad communication with the healthcare providers. There are important training deficiencies in healthcare providers when it comes to the communicative processes. As a consequence, communication with the families usually follows the models of the most veteran colleagues and is based on their own experiences and mistakes.21 On top of improving the how, it is also necessary to get to know what informative priorities the person who is going to receive such information has. This study shows that families prioritize survival, sequelae and the impact they have. They want to know how they are going to be informed, how will the patient's condition be controlled, how will the patient's well-being be guaranteed, and what options are on the table. As we go down in this hierarchy, the demands are more concrete like what is the therapeutic plan going to look like, what should the family do, or what devices are being used, among others.
The results presented here show that families and professionals perceive informative demands differently. This is why we should know how important different aspects are for the families and for professionals. On the one hand, professionals and families have different hierarchies when it comes to the informative priorities. There is more coincidence between doctors and nurses, and more differences between doctors and families. On the other hand, professionals gave low scores, that is, the questions were more important to families than professionals. This gap could be explained by the preoccupation and ignorance from the families of certain situations that healthcare providers live as daily routine and that, from the clinical point of view, are unimportant.
Lastly, we contributed to the debate of what questions do the families wish to be informed on by different professionals. The families think that a great deal of relevant questions can be answered by nurses or doctors alike (for the families, in 63% of the questions the answer on who should respond to the questions was “both”). Of all the questions they think should be answered by doctors or nurses, they think doctors should answer those that have to do with prognosis, sequelae, treatment, and diagnosis. On the other hand, they think nurses are better positioned to answer questions related to caregiving, sensations, setting, and rules, among other. In line with these results, the guidelines established by the Society of Critical Care Medicine on assisting families of critically ill patients17 say that information should be a team effort and recommend that information should be provided by both professionals alike. However, in practice, issues that have to do with legislation, the organization of services, training, and professional competence, and even, professional interests complicate the doctor-nurse process of providing information together.
For instance, in Spain the general rule of most ICUs is that it is only the treating physician who should inform the families, so he is usually alone when doing this, or else, doctors and nurses separately. In very few ICUs doctors and nurses provide information to the families together.14 The nurses usually do not know what kind of information the family has been provided with, so in order to avoid contradictions, they take a cautious role by providing brief and uncompromising information. Although there are initiatives that try to change this practice,22,23 nurses have always tried to not be there during the informative process24 and even justify that this informative process is not one of their responsibilities. It is not uncommon to find nurses downplaying information and denying communication with the families.16,25
A study like this one should be generalized being extremely cautious. When comparing our results to Peigne et al.’s,18 there is a coincidence in 9 of the 21 questions considered the most important ones. Although both studies have questions on prognosis, treatment and information, the French study also has questions on family involvement in the healthcare process or in the decision-making process. The origin of this mismatch can be the cultural differences of the populations surveyed or the different information policies of these two countries that should be taken into consideration.
Quality communication requires training and the collaborative effort of a team working adequately.26 We should assess how different institutions deal with these aspects, what are the tools that we using, and what stand do we take with one another. Also, what role do we play in communication with our colleagues, patients, and the families. Also, it is necessary to implement these recommendations in the reference and assess the results of such implementation.27
Matching the information and communication provided by the healthcare teams to the demands and needs from the families of critically ill patients will not only improve the perception they have of the healthcare that the patient is receiving but also help them face these difficult moments. One of the limitations of our study is that the answers were not assessed based on the clinical results obtained (survival). Future studies should analyze the differences between the opinion of the families of patients who survived and those who did not. This study did not take into consideration the different perception of attending physicians and residents. Thus, in future studies, it would be advisable to take into consideration all the possible differences in their respective contributions.
ConclusionsThe most important questions for the families have to do with prognosis and severity, and the need for receiving information. Although healthcare providers think these questions are a priority too, they are usually less concerned about the preoccupations of the families and there is significant divergence in the priority of some of the concerns shown by the families.
Families think that most of their informative demands can be satisfied by doctors and nurses alike. This means that communication and consensus are needed between doctors and nurses in order to provide coherent and complete information, which is why we think it is essential to promote a change in the information policies by fostering doctor-patient information processes.
Therefore, it would be important to implement tools between nurses and doctors (training in communication techniques such as active hearing, help relationship) in order to improve our relation to the families.
AuthorshipThe study promoter and leading researcher is José Manuel Velasco Bueno who was backed by the Research Team of the Humanizing Intensive Care (HUCI in Spanish) Project that fostered recruitment from the participant centers. Each and every one of the authors contributed to the study design, the reference search, the analysis of data and the discussion of results. All of them reviewed the manuscript in its different versions and approved the manuscript final version.
Conflict of interestsNone declared.
We wish to thank the collaboration from all the professionals from the different Intensive Care Units involved, both as local coordinators of the study and as assistants providing interesting contributions. And obviously we wish to thank the families of the critically ill patients admitted to these ICUs who gave us their particular view on the information requested by them.
Alonso Tovar, Ana Rosa (Hospital Morales Meseguer, Murcia); Álvarez García, M. Paz (Hospital U. Marqués de Valdecilla, Santander); Aparicio Zaldívar, Eva Gregoria (Hospital Universitario de Fuenlabrada, Madrid); Aragón López, Ana María (Hospital La Mancha Centro, Alcázar de San Juan, Ciudad Real); Bellido Domínguez, José María (Hospital U. Virgen de La Victoria, Málaga); Bermejo Caballero, Beatriz (Hospital Infanta Cristina, Badajoz); Borrego Domínguez, Raúl (UCIP Hospital Virgen de La Salud, Toledo); Bravo Arcas, María Luisa (Hospital Clínico San Carlos, Madrid); Calleja Rodríguez, Clementina (Hospital U. Central de Asturias, Oviedo); Canabal Berlanga, Alfonso (Hospital Virgen de La Salud, Toledo); Carballeda Camacho, Eva (Hospital Virgen de La Victoria, Málaga); Casamián Labarta, Alfonso (Hospital Royo Villanova, Zaragoza); Cuadrado Zaragoza, Oscar (Hospital U. Puerta de Hierro, Majadahonda, Madrid); Cuenca Rodríguez, Luis (Hospital U. Los Arcos del Mar Menor, Murcia); Dalmau Monfort, Lourdes (Hospital de Barcelona, Barcelona); Díaz López, Yasmina (Hospital Clínic, Barcelona); Escudero Augusto, Dolores (Hospital U. Central de Asturias, Oviedo); Estévez Vicente, Manuela (Hospital Álvaro Cunqueiro, Vigo); Fraiz Padín, Auxi (Hospital Regional Málaga, Málaga); Franco Valenzuela, Raquel (Hospital U. Mútua de Terrassa, Barcelona); Gallego Gutiérrez, Isabel (Hospital Regional Málaga, Málaga); García Arias, Belén (Hospital U. Central de Asturias, Oviedo); García García, Yolanda (Hospital Royo Villanova, Zaragoza); García Rodríguez, Daida (Quirón Salud, Albacete); García Saorín, Noemí (Hospital Infanta Sofía, Madrid); Gómez Canosa, María Sandra (C. H. Arquitecto Marcide, Ferrol, A Coruña); Herráiz Bermejo, Leonor (Hospital U. Puerta de Hierro, Majadahonda, Madrid); Huidobro Labarga, Beatriz (UCIP Hospital Virgen de La Salud, Toledo); Iribarren Diarasarri, Sebastián (Hospital Universitario Araba, Vitoria); Lafuente García Jesús, Pablo (Hospital Royo Villanova, Zaragoza); Leiva Aguado, Gemma (Hospital La Fe, Valencia); Llanos Jorge, Celina (Hospital Quirón, Tenerife); Lospitao Gómez, Sara (Hospital U. de Fuenlabrada, Madrid); Marina Talledo, Nuria (Hospital U. Marqués de Valdecilla, Santander): Martín Gallardo, Félix José (Hospital de Ronda, Málaga); Martín Iglesias, Lorena (Hospital U. Central de Asturias, Oviedo); Martin López, Caridad (C.H. de Santiago de Compostela, A Coruña); Martínez Fernández, María Del Mar (Hospital Regional Málaga, Málaga); Martorell Servera, Petra (Hospital U. Son Espases, Mallorca); Mas Bilbao, Naia (Hospital de Galdakao-Usansolo, Vizcaya); Medina Pérez, Sara (Hospital Quirón, Tenerife); Millán Castilla, Francisco (Hospital Costa del Sol, Marbella, Málaga); Miquel Diego, Pau (Hospital Germans Trias i Pujol, Badalona, Barcelona); Morón Canís, Mónica (Hospital Xanit Intern, Benalmádena, Málaga); Mulet Amengual, Antònia (Hospital Son Llàtzer, Mallorca); Mulet Jiménez, Amalia (Hospital Verge de La Cinta, Tortosa, Tarragona); Murcia Sáez, Isabel (Hospital Universitario de Albacete, Albacete); Naveira Abeigón, Enrique (Clínica Santa Elena, Torremolinos, Málaga); Ortega Guerrero, Álvaro (Hospital Quirón, Málaga); Pérez Lis, Amparo (Hospital Álvaro Cunqueiro, Vigo, A Coruña); Rojas Amezcua, María (Hospital Infanta Margarita, Cabra, Córdoba); Rubió i García, Lluís-Joaquim (Hospital Mare de Déu dels Lliris, Alicante); Rubio Navarro, Manuel (Hospital Virgen de La Victoria, Málaga); Sánchez Morillo, Matilde (UCIP Hospital Sant Joan de Déu, Barcelona); Sánchez Suárez, Yolanda (Hospital U. Puerta de Hierro, Majadahonda, Madrid); Torondel Capdevila, Eva M. (Hospital Verge de la Cinta, Tortosa, Tarragona); Torralba Melero, Martin (Hospital U. de Albacete, Albacete); Velasco Sanz, Tayra (Hospital Clínico San Carlos, Madrid); Vicente Martínez, M. Lucía (Hospital de Granollers, Barcelona); Vilaseca Garrigasait, Esther (Hospital de Barcelona, Barcelona); Wojtysiak, Monika (Hospital Universitario Quirón, Madrid); Xirgu Cortacans, Judith (Hospital de Granollers, Barcelona).
The names of the collaborating professionals in this study are related in Annex 1.
Please cite this article as: Velasco Bueno JM, Alonso-Ovies A, Heras La Calle G, Zaforteza Lallemand C, Equipo de investigación del Proyecto HUCI (Humanizando los Cuidados Intensivos). Principales demandas informativas de los familiares de pacientes ingresados en Unidades de Cuidados Intensivos. Med Intensiva. 2018;42:337–345.