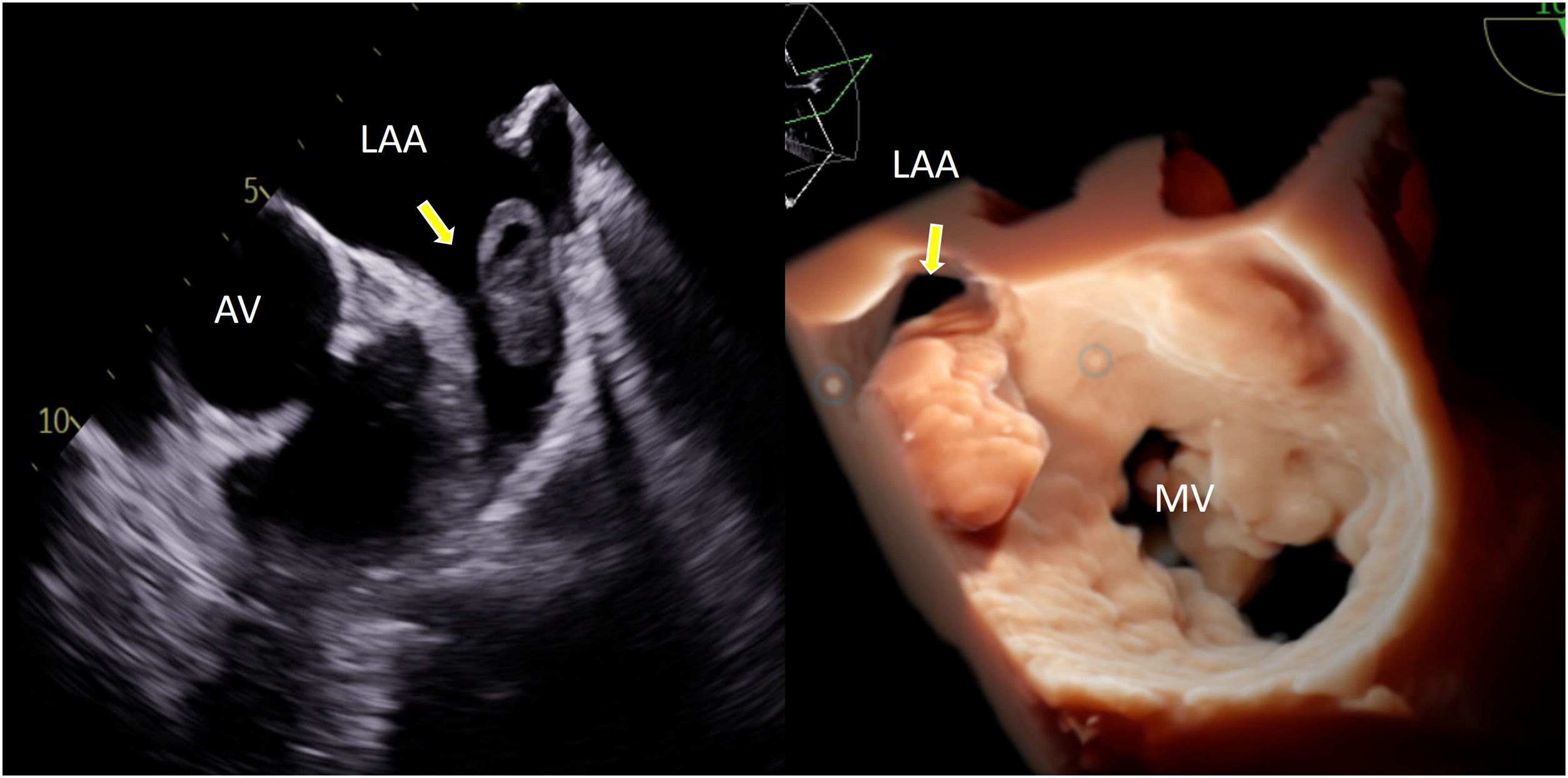
A 74-year-old woman with hypertension and paroxysmal atrial fibrillation (CHA₂DS₂-VASc score of 2) presented to the emergency department with symptomatic atrial fibrillation (AF) and rapid ventricular response. She had not been receiving anticoagulation. A bedside transthoracic echocardiogram showed severe left ventricular dysfunction, and she was admitted for rate control and planned direct current cardioversion (DCCV). As per standard protocol in non-anticoagulated patients, a transesophageal echocardiogram (TOE) was performed prior to cardioversion. TOE revealed a massive, multilobulated thrombus entirely occupying the left atrial appendage (Fig. 1, yellow arrows), contraindicating immediate cardioversion. Despite initial stability and anticoagulation initiation, the patient developed multifocal ischemic stroke 48 h later.
This case underscores the potentially silent yet high-risk nature of thrombus formation in patients with paroxysmal AF, even with intermediate thromboembolic risk scores. It highlights the essential role of TOE before cardioversion in identifying thrombi that may not be evident clinically or on transthoracic imaging. Early identification of intracardiac thrombus can prevent catastrophic outcomes and modify management strategies, emphasizing the role of careful imaging-based risk stratification in atrial fibrillation.
Ethics approval and consent to participateNot applicable.
Consent for publicationThis case report was conducted in accordance with the ethical guidelines of Gold Coast University Hospital, with patient data anonymized to ensure confidentiality. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Disclosure of funding sourceThe present article has not received any grants or financial support.
Nothing to declare.