For decades, the material sciences (rheology) have been applied to mechanical ventilation (MV), and calculations have been made of the work burden for the respiratory system associated with breathing through a ventilator. In this context, the lung is regarded as a viscoelastic element, and mathematical models have been used to describe the relationship between the tension (stress) upon the respiratory system during ventilation and its corresponding deformation (strain).1
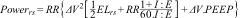
Gattinoni et al. defined mechanical power (MP) as the energy transmitted to the respiratory system per unit time (in J/min). In patients subjected to volume control ventilation (VCV), they calculated MP by multiplying each component of the classical equation of motion by volume variation and respiratory rate – thereby including the contribution of different MV-related factors in lung injury.2
RR: respiratory rate; ΔV: tidal volume; ELrs: elastance of the respiratory system; I:E: inspiratory/expiratory time; Raw: airway resistance; PEEP: positive end-expiratory pressure
These same investigators demonstrated a correlation between ventilator-induced lung injury (VILI) and MP, and even defined an injury threshold.3
Mechanical power increases exponentially with tidal volume, driving pressure (DP), flow and respiratory rate, and increases linearly with positive end-expiratory pressure (PEEP) and airway resistance (Raw) – these parameters being described as factors associated with mortality in ventilated patients in the multicenter LUNG SAFE cohort.4
Since then, several simplified versions of the formula developed by Gattinoni et al. have been introduced, as well as specific formulas for pressure control ventilation (PCV) modes, since the equation for calculating MP in VCV is based on a linear increase in airway pressure (Paw) during inspiration, which is not adequate in PCV modes.5,6 Assuming an ideal square curve of Paw during inspiration in PCV, the calculation of MP is based on the inspiratory pressure gradient (Pinsp).7 The problem with so many formulas is that some authors have reported broad variations in MP depending on the formula used to calculate it
The present issue of Medicine Intensiva publishes a study on the prevalence of elevated MP in patients subjected to MV in routine clinical practice. This international, multicenter observational study involved a cohort of 372 patients from 133 Intensive Care Units (ICUs) in 15 countries. Most of the patients required intubation and MV due to acute respiratory failure (33%) or neurological disorders (31%).
As the main finding of the study, the patients ventilated in PCV mode presented greater MP than those ventilated in VCV mode (19 and 16 J/min, respectively). Thirty-eight percent of the patients presented MP > 17 J/min, with no statistically significant differences between the PCV and VCV modes. This study thus evidences the high prevalence of potentially harmful MP in our routine clinical practice.
The difference in MP between the PCV and VCV modes found by the authors is consistent with previous data found in the literature. An explanation for these observations would be that the amount of energy distributed by the ventilator varies due to the difference between flow patterns, leading to different P/V curves P/V.8 Furthermore, greater transpulmonary pressure gradients have been reported in PCV versus VCV mode.
In the same way that Amato et al. have shown a driving pressure (DP) of > 15cmH2O to be more significantly associated with mortality in patients with acute respiratory distress syndrome (ARDS) than plateau pressure (Pplateau), recent studies suggest that MP values of > 18−20 J/min are also associated to increased mortality.9
But is the calculation of mechanical power really necessary?
Guérin et al. observed a linear relationship between DP, MP, Pplateau and compliance in patients with ARDS subjected to protective ventilation.10 However, since MP is derived from the equation of motion, it incorporates additional parameters not included in DP, such as flow or respiratory rate, which can impact mortality in patients with ARDS.11 It thus affords an additional risk estimate beyond DP alone. Prospective studies are needed to examine the effect of a ventilatory strategy upon controlled MP versus the DP management strategy, though it would be interesting to have continuous MP monitoring at the patient bedside to minimize the damage induced by MV.
The study also contemplates the investigation of different components of MP, establishing the surrogate parameters that best represent lung response to ventilation. Based on this, mathematical models are established for each ventilation mode, choosing the best option using the Akaike Information Criterion (AIC) tool. The AIC estimates the error of prediction of the relative quality of statistical models for a given set of data. The models best assessed by the AIC system contain strain and strain rate surrogates as in previous studies, reflecting this viscoelastic component of the lung.
Although the mentioned study is observational, its strengths lie in the large sample size involved and the participation of 15 different ICUs, with the added novelty of using AIC as a statistical tool for determining the best way to calculate MP.
Mechanical power is little used as a tool, due to the difficulty of calculating it in the routine clinical practice setting. It therefore would be advisable for automated systems to perform continuous calculation of this variable. Another consideration is how to incorporate it into the daily activity of the professionals. The LUNG SAFE study has recently evidenced the scant presence of DP in clinical practice, despite its simplicity. We thus encourage professionals to delve into it through this study and to calculate it in their ventilated patients as a complementary variable for adjusting the ventilator. Regardless of whether we prefer DP or MP, in the end our goal must be to reduce MV-induced injury, based on the classical principle “primum non nocere”.
FundingNot applicable.
Conflicts of interestNot applicable.
See related article: https://doi.org/10.1016/j.medine.2023.11.004