To evaluate changes in the disconnection of mechanical ventilation in Spain from 1998 to 2016.
DesignPost-hoc analysis of four cohort studies.
Ambit138 Spanish ICUs.
Patients2141 patients scheduled extubated.
InterventionsNone.
Variables of interestDemographics, reason for mechanical ventilation, complications, methods for disconnection, failure on the first attempt at disconnection, duration of weaning, reintubation, post-reintubation tracheotomy, ICU stay and mortality.
ResultsThere was a significant increase (p < 0.001) in the use of gradual reduction of support pressure. The adjusted probability of using the gradual reduction in pressure support versus a spontaneous breathing trial has increased over time, both for the first attempt at disconnection (taking the 1998 study as a reference: odds ratio 0.99 in 2004, 0.57 in 2010 and 2.43 in 2016) and for difficult/prolonged disconnection (taking the 1998 study as a reference: odds ratio 2.29 in 2004, 1.23 in 2010 and 2.54 in 2016). The proportion of patients extubated after the first attempt at disconnection has increased over time. There is a decrease in the ventilation time dedicated to weaning (from 45% in 1998 to 36% in 2016). However, the duration in difficult/prolonged weaning has not decreased (median 3 days in all studies, p = 0.435).
ConclusionsThere have been significant changes in the mode of disconnection of mechanical ventilation, with a progressive increase in the use of gradual reduction of pressure support. No relevant changes in outcomes have been observed.
Evaluar los cambios en la desconexión de la ventilación mecánica en España desde 1998 hasta 2016.
DiseñoAnálisis post-hoc de cuatro estudios de cohorte.
ÁmbitoUn total de 138 UCI.
EnfermosUn total de 2.141 enfermos extubados de forma programada.
IntervencionesNinguna.
Variables de interés principalesDemográficas, motivo de ventilación mecánica, complicaciones, métodos para la desconexión, fracaso del primer intento de desconexión, duración de la desconexión, reintubación, traqueotomía post-reintubación, estancia y mortalidad en la UCI.
ResultadosSe observa un aumento significativo (p < 0,001) en la presión de soporte como técnica de desconexión. Ha aumentado, a lo largo del tiempo, la probabilidad ajustada de utilizar la presión de soporte progresivamente decreciente frente a una prueba de ventilación espontánea, tanto para el primer intento de desconexión (referencia estudio de 1998: odds ratio 0,99 en 2004, 0,57 en 2010 y 2,43 en 2016) como para la desconexión difícil/prolongada (referencia estudio de 1998: odds ratio 2,29 en 2004, 1,23 en 2010 y 2,54 en 2016). La proporción de extubación tras el primer intento de desconexión ha aumentado con el tiempo. Hay una disminución del tiempo dedicado a la desconexión (desde un 45% en 1998 a un 36% en 2016). Sin embargo, no ha disminuido la duración en la desconexión difícil/prolongada (mediana 3 días en todos los estudios, p = 0,435).
ConclusionesHa habido cambios significativos en el modo de desconexión de la ventilación mecánica, con un aumento progresivo del uso de la presión de soporte. Se han observado mínimos cambios en los desenlaces.
Over the last 30 years significant changes have been made in the process of weaning from mechanical ventilation. At the end of the 1980s an editorial concluded: «It is evident that more studies are needed before our knowledge on this relevant clinical area can reach a truly scientific level. Currently, weaning is still an art».1 At that time, in the United States, synchronized intermittent mandatory ventilation was the preferred weaning mode used in over 90% of all weaning trials.2 In a study conducted among Spanish intensive care units back in 1992, 24% of the patients were weaned using the T-tube trial of increasing duration; 18% with synchronized intermittent mandatory ventilation (SIMV); 15% with pressure support ventilation (PSV); 9% with SIMV with PSV, and 33% with some combination of 2 or more of the aforementioned methods.3
The clinical trials with randomization conducted from the 1990s until present day have allowed us to systematize weaning from mechanical ventilation using 3 different steps: predictor measurement followed by spontaneous breathing trial followed by extubation.4 One clinical practice guideline5 and one consensus conference6 determine that a spontaneous breathing trial is the best diagnostic test to determine whether a patient can be extubated and establish that this trial should be performed at its best with low-PSV. In patients with a failed first trial, the results from the clinical trials conducted in the 1990s recommended preventing the use of SIMV.7 Confirmation that the use of SIMV as a weaning technique could extend the duration of weaning came along with studies that demonstrated that weaning could only be achieved with a gradually decreasing PSV8 or else with a daily spontaneous breathing trial using a T-tube.9,10 These studies were the pillars on which weaning from ventilation is founded based on scientific bases.
The primary endpoint of this analysis conducted among patients admitted to Spanish intensive care units who participated in 4 international trials on mechanical ventilation is to assess whether the process of weaning from mechanical ventilation changed parallel to the results coming from clinical trials or the recommendations coming from the guidelines. The analysis secondary endpoint was whether there is geographical variability in the weaning modes.
Patients and methodsPost-hoc analysis of 4 prospective, observational, and multicenter trials conducted throughout a month in the years 1998,11 2004,12 2010,13 and 2016.14 The studies included patients who required invasive mechanical ventilation for over 12 h or non-invasive ventilation for over an hour. For the purpose of this analysis, only patients admitted to Spanish intensive care units and extubated on a scheduled basis were included in the studies.
The previously described methodology15 was similar for the 4 studies. Patients who had not been intubated were excluded (successful non-invasive ventilation or patients with previous tracheostomies), patients in whom weaning from mechanical ventilation was not started, patients who were accidentally extubated, and patients in whom a tracheostomy was performed before or during the process of weaning. The start of weaning was defined as the moment in which the treating physician considered that it was possible that the patient would resume spontaneous breathing after meeting the standard criteria to start the process of weaning. The following variables were recorded: method for the first weaning trial [spontaneous breathing trial (T-tube, low-PSV, CPAP, a different method) or gradual reduction of pressure support ventilation (PSV, SIMV with or without PSV, a different method)], failed first weaning trial, method of weaning in patients with failed first trial [spontaneous breathing trial (T-tube, low level of PSV, CPAP, a different method) or gradual reduction of pressure support ventilation (PSV, SIMV with or without PSV, a different method)], extubation date, use of non-invasive ventilation or oxygen therapy using high-flow nasal cannula after extubation (uncollected in all the studies), need for reintubation, moment of reintubation, and performance of tracheostomy after reintubation. Patients we categorized based on the duration of weaning6 into easy weaning (extubated patients during the first weaning trial), difficult weaning (patients who required up to 7 days to be extubated since the first weaning trial), and prolonged weaning (patients who require > 7 days to be extubated). Patients were followed until they were discharged from the hospital.
The ethical committees from each hospital approved the protocol and the need for informed consent was adjusted to the decision of each one of those committees.
In the studies conducted in 1998 and 2004, each investigator was given a manual describing the data and the definitions that should be collected, as well as written forms for data curation. Investigators filled out a form for each patient included and sent it to the Coordination Center at Hospital Universitario de Getafe, Madrid, Spain. Forms were eventually included in an electronic database. In the studies conducted back in 2010 and 2016, all data was entered through a safe website. Also, before the analysis, all the entries were analyzed to detect data and potentially erroneous atypical values. Cases with data lost in the main variables were not included in the analysis. The STROBE checklist (Strengthening the Reporting of Observational Studies in Epidemiology) was used for cohort observational studies.16
Statistical analysisResults are expressed as mean (standard deviation), median (percentile range 25, percentile 75), absolute frequencies and proportions when appropriate. For continuous variable comparison, the ANOVA or the Kruskall–Wallis test were used while the chi-square test was used to compare the categorical variables.
To estimate time tendencies in the method of weaning a logistics regression model was used with the study year—coded as dummy variable—as independent variable, and with a method of weaning (spontaneous breathing trial or gradual reduction of pressure support ventilation) as dependent variable. To adjust this estimate, a multilevel logistics regression model was used (patients, and regional societies affiliated to SEMICYUC) including age, SAPS II, reason to start mechanical ventilation, administration of sedatives and neuromuscular blockers, number of organ dysfunctions, and days on ventilatory support before starting the process of weaning. The random part of the model included 2 random effects and their possible correlation: the effect that the method of weaning had among different regional societies, and the effect of changes across time in the weaning mode. The measurement of fixed effects was the odds ratio with 95% confidence intervals. To estimate random variability in the weaning method among different Spanish autonomous communities the median odds ratio (MOR) was used. This statistic is defined as the median of the overall odds ratios that can be obtained by comparing 2 patients with identical characteristics treated in 2 different centers picked at random. The MOR measures the variation between the use of the spontaneous ventilation trial vs a gradually decreasing PSV in different geographical regions, which is not explained by the remaining variables included in the model.
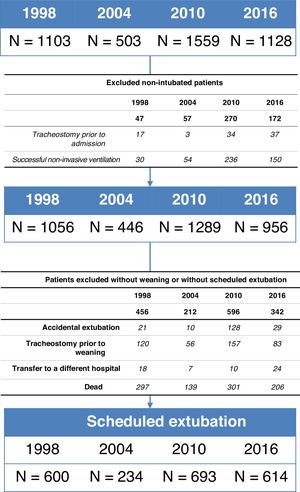
ResultsA total of 2141 patients out of the 4293 included in the 4 studies were scheduled for extubation (Fig. 1). Significant differences were seen (P < .001) in the number of patients who were extubated in each study: 54% (600/1103) in 1998, 46% (234/503) in 2004, 44% (693/1.559) in 2010, and 54% (614/1.128) in 2016. Table 1 shows the comparison of the characteristics when the weaning process was started.
Characteristics of patients at the beginning of weaning from mechanical ventilation.
| 1998 | 2004 | 2010 | 2016 | |
|---|---|---|---|---|
| N = 600 | N = 234 | N = 693 | N = 614 | |
| Age, years, mean (SD) | 60 (18) | 57 (18) | 61 (18) | 63 (16) |
| Women, n (%) | 206 (35) | 84 (36) | 240 (35) | 204 (33) |
| SAPS II, scores, mean (SD) | 41 (16) | 40 (15) | 44 (17) | 45 (17) |
| Reason for starting mechanical ventilation, n (%) | ||||
| Chronic obstructive pulmonary disease | 88 (15) | 20 (8) | 31 (4) | 28 (5) |
| Asthma | 8 (1) | 1 (0.4) | 6 (1) | 4 (1) |
| Other chronic pulmonary disease | 7 (1) | 5 (2) | 3 (0.4) | 6 (1) |
| Acute respiratory distress syndrome | 9 (1.5) | 5 (2) | 15 (2) | 8 (1) |
| Postoperative respiratory failure | 149 (25) | 38 (16) | 154 (22) | 157 (26) |
| Heart failure | 71 (12) | 20 (8.5) | 63 (9) | 31 (5) |
| Aspiration | 10 (2) | 3 (1) | 15 (2) | 11 (2) |
| Pneumonia | 44 (7) | 21 (9) | 53 (8) | 51 (8) |
| Sepsis | 32 (5) | 18 (8) | 66 (9.5) | 53 (9) |
| Trauma | 54 (9) | 16 (7) | 22 (3) | 21 (3) |
| Cardiac arrest | 13 (2) | 4 (2) | 38 (6) | 31 (5) |
| Other cause | 24 (4) | 15 (6) | 25 (4) | 26 (4) |
| Neurological disease | 105 (17.5) | 65 (28) | 200 (29) | 182 (30) |
| Neuromuscular disease | 4 (1) | 3 (1) | 2 (0.3) | 5 (1) |
| Treatment during mechanical ventilation | ||||
| Sedation, n (%) | 456 (76) | 206 (88) | 599 (86) | 545 (89) |
| Days on sedation, median (P25, P75) | 2 (1.5) | 4 (2. 6) | 3 (2. 5) | 3 (2.5) |
| Neuromuscular blockers, n (%) | 52 (9) | 21 (9) | 73 (10.5) | 71 (12) |
| Days on neuromuscular blockers, median (P25, P75) | 2 (1.4) | 1 (1.3) | 2 (1.3) | 2 (1.3) |
| Complications during mechanical ventilation, n (%) | ||||
| Acute respiratory distress syndrome | 8 (1) | 23 (10) | 25 (4) | 19 (3) |
| Mechanical ventilation-associated pneumonia | 46 (8) | 5 (2) | 28 (4) | 1 (0.2) |
| Sepsis | 35 (6) | 15 (6) | 94 (14) | 83 (15) |
| Cardiovascular failure | 121 (20) | 73 (31) | 297 (43) | 303(49) |
| Renal failure | 49 (8) | 41 (17) | 113 (16) | 90 (15) |
| Liver failure | 10 (2) | 8 (3) | 13 (2) | 9 (1) |
| Hematologic disturbances | 28 (5) | 18 (8) | 30 (4) | 25 (4) |
| Days on mechanical ventilation before starting weaning, median (P25, P75) | 3 (3.6) | 6 (3.10) | 4 (2. 8) | 4 (2.8) |
SAPS, Simplified Acute Physiology Score.
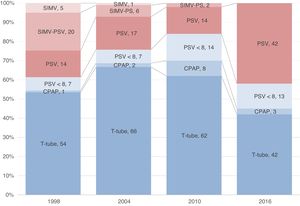
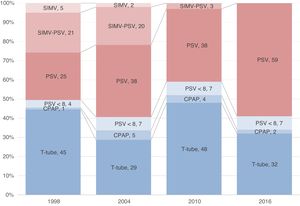
Table 2, and Figs. 2 and 3 show the evolution across time in the use of each weaning method. There is a significant change from the first study with an increased use of gradually decreasing PSV to start weaning and as weaning method in patients with failed first weaning trials. Therefore, the crude and adjusted probability of using gradual reduction of pressure support ventilation (basically PSV) has been gaining traction with the passing of time (Table 3).
Comparison of all weaning methods.
| 1998 | 2004 | 2010 | 2016 | |
|---|---|---|---|---|
| N = 600 | N = 234 | N = 693 | N = 614 | |
| Method used for the first weaning trial, n (%) | ||||
| Spontaneous breathing trial | 373 (62) | 175 (75) | 587 (85) | 357 (58) |
| Support gradual reduction | 227 (38) | 59 (25) | 106 (15) | 257 (42) |
| Failed first trial, n (%) | 305 (51) | 87 (37) | 212 (31) | 165 (27) |
| Method used for weaning in patients with failed first trials, n (%) | ||||
| Spontaneous breathing trial | 151 (49) | 35 (40) | 124 (58) | 67 (41) |
| Support gradual reduction | 154 (51) | 52 (60) | 88 (42) | 98 (59) |
Evolution in time of the probability of using a gradually decreasing pressure support ventilation vs spontaneous respiratory trial as a weaning method from mechanical ventilation taking the first study conducted in 1998 as the reference.
| First weaning trial | ||||
|---|---|---|---|---|
| Crude probability | Adjusted probabilitya | |||
| Odds ratio | 95%CI | Odds ratio | 95%CI | |
| 1998 | 1 | 1 | ||
| 2004 | 1.18 | 0.78 to 1.58 | 0.99 | 0.68 to 1.43 |
| 2010 | 0.59 | 0.45 to 0.79 | 0.57 | 0.42 to 0.77 |
| 2016 | 2.38 | 1.86 to 3.06 | 2.43 | 1.85 to 3.20 |
| Difficult/prolonged weaning | ||||
| 1998 | 1 | 1 | ||
| 2004 | 2.48 | 1.52 to 4.04 | 2.29 | 1.35 to 3.87 |
| 2010 | 1.31 | 0.91 to 1.89 | 1.23 | 0.81 to 1.88 |
| 2016 | 2.44 | 1.65 to 3.60 | 2.54 | 1.63 to 3.95 |
95%CI, 95% confidence interval.
Significant variability that has not changed across time has been reported regarding the use of weaning methods associated with the Spanish autonomous community where weaning was performed: MOR for the use of a gradually decreasing PSV vs spontaneous breathing trial in 1998: 1.68 (95% confidence interval: 1.15 to 2.20); in 2004: 1.54 (95% confidence interval: 1.17 to 1.91); back in 2010: 1.54 (95% confidence interval: 1.16 to 1.92); in 2016: 1.67 (95% confidence interval: 1.13 to 2.22).
OutcomesAdded to the changes seen in the use of each weaning mode, changes have been reported in the clinical outcomes (Table 4). The number of patients extubated after a first failed weaning trial has increased with the passing of time. Shorter ventilatory support times dedicated to weaning have been reported (from 45% in 1998 down to 36% in 2016). However, weaning time has not decreased in patients with difficult/prolonged weaning trials.
Outcomes.
| 1998 | 2004 | 2010 | 2016 | P | |
|---|---|---|---|---|---|
| N = 600 | N = 234 | N = 693 | N = 614 | ||
| Ventilation days until starting weaning, median (P25, P75) | 3 (2.6) | 6 (3. 10) | 4 (2. 8) | 4 (2. 8) | < .001 |
| Amount of time dedicated do weaning, mean (standard deviation)a | 45 (22) | 31 (17) | 35 (20) | 36 (21) | < .001 |
| Days dedicated to weaning, median (P25, P75) | 2 (1.3) | 1 (1.2) | 1 (1.2) | 1(1.2) | < .001 |
| Classification of weaning, n (%) | < .001 | ||||
| Easy | 298 (50) | 147 (63) | 493 (71) | 449 (73) | |
| Difficult | 260 (43) | 79 (34) | 164 (24) | 149 (24) | |
| Prolonged | 42 (7) | 8 (3) | 36 (5) | 16 (3) | |
| Days dedicated to weaning, median (P25, P75) | |||||
| Difficult weaning | 3 (2.4) | 3 (2.4) | 3 (2.4) | 3 (2.4) | .926 |
| Prolonged weaning | 10 (7.13) | 8.5 (7.10) | 11 (8.15) | 9.5 (8.13) | .214 |
| Reintubation within the first 48 h, n (%) | 91 (15) | 25 (11) | 70(10) | 52 (8) | .002 |
| Tracheostomy in reintubated patients, n (%) | 35 (38) | 7 (28) | 26 (37) | 21 (40) | .767 |
| Days at the ICU setting, median (P25, P75) | 9 (5.14) | 10 (6.16) | 8 (5.15) | 8 (5.15) | .108 |
| Mortality at the ICU setting, n (%) | 37 (6) | 15 (6) | 41 (6) | 63 (10) | .014 |
| Length of stay, median (P25, P75)b | 24 (16.37) | 24 (15.43) | 22 (14.39) | 22 (12.36) | .011 |
| In-hospital mortality, n (%)b | 94 (17) | 34 (15) | 96 (14) | 118 (20) | .043 |
There has been a gradual and significant increase (P = .027) in the use of non-invasive ventilation after extubation: 5% in 2004, 10% in 2010, and 11% in 2016. The rate of failure using this technique has gone down: 25% in 2004, 27% in 2010, and 19% in 2016.
Oxygen therapy with high-flow nasal cannula was only reported in the study from 2016. A total of 8% of all extubated patients received oxygen therapy with high-flow nasal cannula (69% as prevention of respiratory failure after extubation, and 31% as treatment of such respiratory failure). The rate of reintubation of patients treated with this therapy was 37%.
It has been reported that the rate of reintubation within the first 48 h (Table 4) plummets. The mortality rate of patients who need intubation has gradually been going down with the passing of time: 24% in 1998, 24% in 2004, 16% in 2010, and 21% in 2016 (P = .585).
DiscussionThe main observation from our analysis is that weaning from mechanical ventilation has changed since the 1990s. The main changes seen are a wider use of a gradually decreasing PSV parallel to a lesser use of spontaneous breathing trial; SIMV with or without PSV has become a somehow marginal mode, and the non-use of new ventilatory support methods is supposed to be more physiological [adaptive support ventilation (ASV), neurally adjusted ventilatory assist (NAVA), proportional assist ventilation (PAV), automatic tube compensation (ATC)] probably because these modes only come in a specific brand of ventilators. Also, because scientific evidence on the role played by weaning from mechanical ventilation is limited.17
The question here is whether these changes have followed an evidence and/or physiology-based tendency. It somehow seems amazing that the leading mode of weaning from mechanical ventilation is reducing ventilatory support, basically PSV. This can be a consequence of the gradual increase of PSV as the leading mode of ventilatory support.14 It can be logical somehow to think that, after a patient has improved the condition that made him dependent upon mechanical ventilation, the treating physician preferred to reduce support until levels that allow extubation would be reached. However, when spontaneous breathing trial is used for weaning, the use of the T-tube and CPAP is more common compared to a low-PSV. These findings are similar to those reported by Burns et al.18. In a survey intended to study the different clinical practices worldwide regarding weaning practices, these authors proved that those who responded to the survey used 2 techniques preferably: PSV with PEEP, and the T-tube.
A meta-analysis that included 31 publications concluded that a spontaneous breathing trial with PSV has 6% more chances of success compared to the T-tube trial (95% confidence interval: 2% to 10%).19 A different meta-analysis—including 16 studies—where work of breathing was measured in 239 patients proved that a PSV trial between 5 cmH2O and 8 cmH2O reduces work of breathing by 30%, effort by 30%, and the index of rapid shallow breathing by 20%. However, work of breathing with the T-tube tuned out to be more accurate compared to the physiological conditions reported after extubation.20 One last meta-analysis that included 10 randomized clinical trials and 3165 patients21 showed no statistically significant differences regarding the rate of successful extubation between the T-tube trial compared to the PSV trial (odds ratio, 0.91; 95% confidence interval: 0.78 to 1.07). These results, although limited by the heterogeneity of the studies included in the meta-analysis question whether a spontaneous breathing trial without assist can cause work of breathing overload with the corresponding greater potential for failure.
Regarding patients on difficult/prolonged weaning trials, a gradual increase in the use of PSV was reported. Evidence regarding weaning for these patients comes from randomized trials conducted in the 1990s. The 2 largest studies were conducted simultaneously,8,9 and had a similar design. However, a few differences seen on the methodology used could be partially responsible for the variable results reported. Brochard et al.8 demonstrated that patients allocated for a gradually decreasing PSV weaned faster compared to those allocated for weaning with SIMV or with the T-tube trial. Esteban et al.9 demonstrated that the best method for weaning was a daily trial of spontaneous respiration with the T-tube.
There is a great geographical variability regarding the use of the mode of weaning. Therefore, all the studies show that 2 patients with identical characteristics will be weaned differently if treated in 2 different units selected at random. Other studies have proven similar results.18
This study has several limitations. The first one being that we considered that the weaning process started when the treating physician thought that the patient was ready to resume spontaneous breathing. However, we don’t know whether the patient met the criteria for weaning at that time. As a matter of fact, it could be that the differences seen in the number of extubated patients after the first failed weaning trial would have been conditioned by this definition. Closely associated with it, we would have the finding of the use of gradual reduction of pressure support ventilation as the first method of weaning from mechanical ventilation. Like we said before, we can deduce that as patients improve in the indication that triggered the start of mechanical ventilation, we should move into an assist support method (basically PSV) with gradual reduction of such support until achieving a level that allows extubation without being able to establish manifestly where the line is drawn between ventilatory support and weaning from ventilatory support. Secondly, the changes seen in the type of patients included in each study may have influenced the mode of weaning used. Therefore, there is a gradual increase of neurological patients who may have peculiarities regarding the process of weaning and extubation.22 Thirdly, no information was collected on the implementation of sedation and mechanical ventilation weaning protocols23 or in the exact duration of spontaneous breathing trials, which has a significant impact on the outcomes of weaning.24–26 Fourthly, the impact complications like ICU setting-acquired muscle weakness27 or delirium28 have in the duration of weaning has not been studied. Finally, the correlation between the classification of weaning and mortality based on the size of the sample was insufficiently study (since patients were classified in the categories defined in the consensus conference, the prolonged weaning group has, in certain years, a small sample size, and it’s therefore unfeasible for any kind of assessable statistical analysis). A recent weaning categorization has not been applied either based on the duration of weaning—the WIND classification29,30—because the design of the studies does not allow estimates of the duration of weaning in patients with tracheostomy or reintubation since these 2 settings are considered final events without any further follow-up.
In conclusion, over the last 2 decades, significant changes have been made in the different processes of weaning from mechanical ventilation. However, we should mention that the tendency of these changes regarding the gradually wider use of PSV is not based on the best pieces of evidence collected from clinical trials31 or physiological studies.32 These changes have not been associated with significant changes in the clinical outcomes.
Authors’ contributionsFernando Frutos-Vivar, Oscar Peñuelas, and Andrés Esteban coordinated the 4 clinical trials conducted, had access to data from all the studies, and take full responsibility on the reliability of this data.
Study design: Andrés Esteban, Fernando Frutos-Vivar, Oscar Peñuelas, and Antonio Anzueto.
Data curation (investigators in 3 or 4 studies): Antonio García-Jiménez, Raúl de Pablo, Manuel Valledor, Miquel Ferrer, Miguel León, José María Quiroga, Susana Temprano, Inmaculada Vallverdú, Rafael Fernández, and Federico Gordo.
Statistical analysis: Alfonso Muriel, Oscar Peñuelas, and Fernando Frutos-Vivar.
Data interpretation: Alfonso Muriel, Oscar Peñuelas, and Fernando Frutos-Vivar.
Manuscript drafting: Fernando Frutos-Vivar.
Manuscript critical review: Oscar Peñuelas, Alfonso Muriel, Jordi Mancebo, Antonio García-Jiménez, Raúl de Pablo, Manuel Valledor, Miquel Ferrer, Miguel León, José María Quiroga, Susana Temprano, Inmaculada Vallverdú, Rafael Fernández, Federico Gordo, Antonio Anzueto, and Andrés Esteban.
Manuscript final approval: Fernando Frutos-Vivar, Oscar Peñuelas, Alfonso Muriel, Jordi Mancebo, Antonio García-Jiménez, Raúl de Pablo, Manuel Valledor, Miquel Ferrer, Miguel León, José María Quiroga, Susana Temprano, Inmaculada Vallverdú, Rafael Fernández, Federico Gordo, Antonio Anzueto, and Andrés Esteban.
Conflicts of interestNone reported.
We wish to thank all investigators associated with Appendix B annex 1 (see Supplementary data).
Please cite this article as: Frutos-Vivar F, Peñuelas O, Muriel A, Mancebo J, García-Jiménez A, de Pablo R, et al. Ventilación mecánica en España, 1998–2016: cambios en la desconexión de la ventilación mecánica. Med Intensiva. 2022;46:363–371.