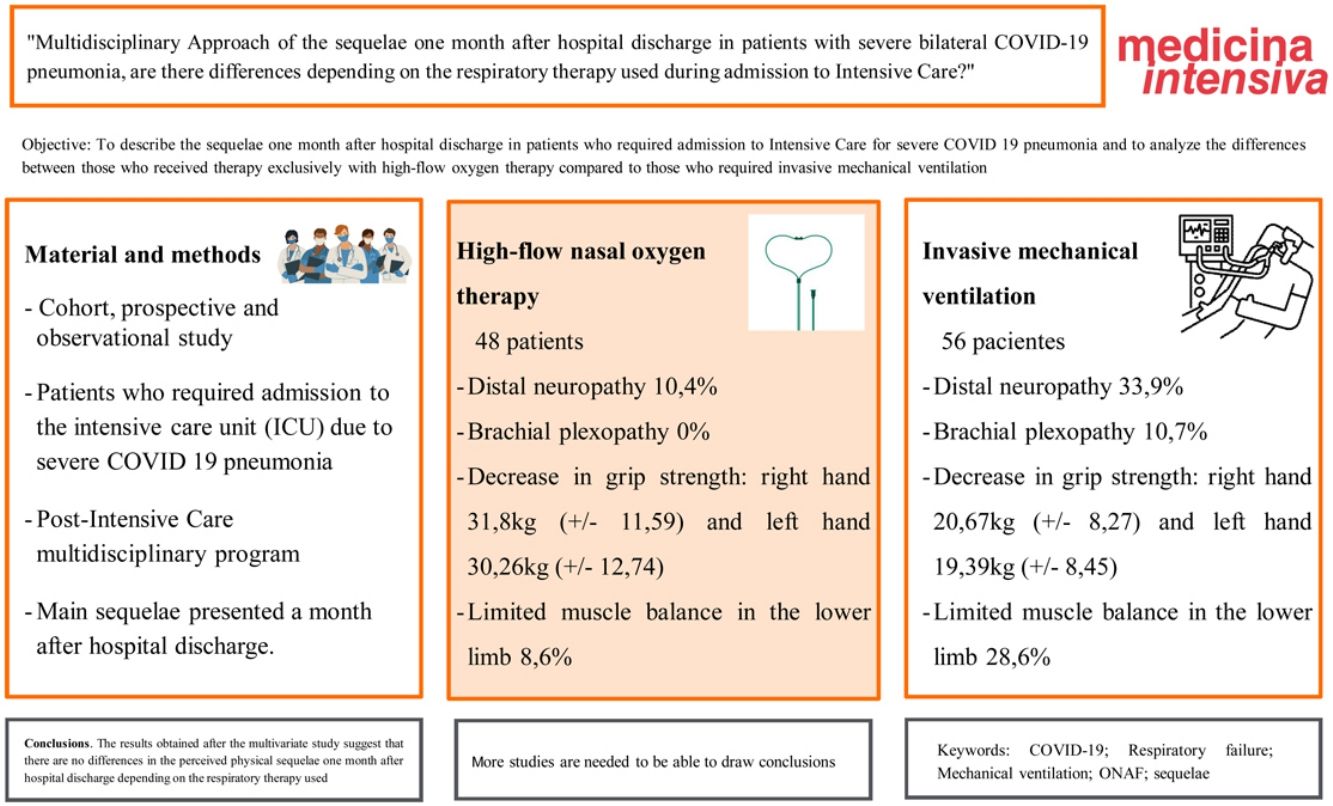
To describe the sequelae one month after hospital discharge in patients who required admission to Intensive Care for severe COVID 19 pneumonia and to analyze the differences between those who received therapy exclusively with high-flow oxygen therapy compared to those who required invasive mechanical ventilation.
DesignCohort, prospective and observational study.
SettingPost-intensive care multidisciplinary program.
Patients or participantsPatients who survived admission to the intensive care unit (ICU) for severe COVID 19 pneumonia from April 2020 to October 2021.
InterventionsInclusion in the post-ICU multidisciplinary program.
Main variables of interestMotor, sensory, psychological/psychiatric, respiratory and nutritional sequelae after hospital admission.
Results104 patients were included. 48 patients received high-flow nasal oxygen therapy (ONAF) and 56 invasive mechanical ventilation (IMV). The main sequelae found were distal neuropathy (33.9% IMV vs 10.4% ONAF); brachial plexopathy (10.7% IMV vs 0% ONAF); decrease in grip strength: right hand 20.67kg (±8.27) in VMI vs 31.8kg (±11.59) in ONAF and left hand 19.39kg (±8.45) in VMI vs 30.26kg (±12.74) in ONAF; and limited muscle balance in the lower limbs (28.6% VMI vs 8.6% ONAF). The differences observed between both groups did not reach statistical significance in the multivariable study.
ConclusionsThe results obtained after the multivariate study suggest that there are no differences in the perceived physical sequelae one month after hospital discharge depending on the respiratory therapy used, whether it was high-flow nasal oxygen therapy or prolonged mechanical ventilation, although more studies are needed to be able to draw conclusions.
Describir las secuelas al mes del alta hospitalaria en pacientes que precisaron ingreso en Cuidados Intensivos por neumonía grave COVID-19 y analizar las diferencias entre los que recibieron terapia exclusivamente con oxigenoterapia con alto flujo con respecto a los que precisaron ventilación mecánica invasiva (VMI).
DiseñoEstudio de cohorte, prospectivo y observacional.
ÁmbitoConsulta multidisciplinar post cuidados intensivos.
Pacientes o participantesPacientes que superaron el ingreso en la unidad de cuidados intensivos (UCI) por neumonía grave COVID 19 desde abril 2020 hasta octubre 2021.
IntervencionesInclusión en el programa multidisciplinar post UCI.
Variables de interés principalesSecuelas motoras, sensitivas, psicológicas/psiquiátricas, respiratorias y nutricionales tras el ingreso hospitalario.
ResultadosSe incluyeron 104 pacientes. 48 pacientes recibieron oxigenoterapia nasal de alto flujo (ONAF) y 56 ventilación mecánica invasiva (VMI). Las principales secuelas encontradas fueron la neuropatía distal (33,9% VMI vs 10,4% ONAF); plexopatía braquial (10,7% VMI vs 0% ONAF); disminución de fuerza de agarre: mano derecha 20,67kg (±8,27) en VMI vs 31,8kg (±11,59) en ONAF y mano izquierda 19,39kg (±8,45) en VMI vs 30,26kg (±12,74) en ONAF; y balance muscular limitado en miembros inferiores (28,6% VMI vs 8,6% ONAF). Las diferencias observadas entre ambos grupos no alcanzaron significación estadística en el estudio multivariable.
ConclusionesLos resultados obtenidos tras el estudio multivariable sugieren no existir diferencias en cuanto a las secuelas físicas percibidas al mes del alta hospitalaria en función de la terapia respiratoria empleada, ya fuera oxigenoterapia nasal de alto flujo o ventilación mecánica prolongada, si bien son precisos más estudios para poder obtener conclusiones al respecto.
Coronavirus disease 2019 (COVID-19) is a relatively new disorder in our setting, having been first reported in Wuhan (China), in December 2019. On 11 March 2020, it was officially declared a pandemic by the World Health Organization (WHO), in view of the alarming spread and severity of the disease.
The appearance of this new infection and the exponential increase in the number of patients requiring admission to the Intensive Care Unit (ICU) due to severe hypoxemia secondary to bilateral pneumonia not only collapsed the ICUs1 but also multiplied the number of patients with more-or-less disabling sequelae caused by prolonged ICU stay, respiratory distress, aggressive treatment (including maneuvering in prone decubitus)2 and the virus itself. To date, a dozen studies have evaluated aspects such as cognitive impairment, 3 motor sequelae with an impact upon patient quality of life4 (pain or malaise, anxiety or depression, personal care and routine activities), perceived fatigue,5 intolerance of exercise, dyspnea in response to moderate physical exertion, limitations referred to physical capacity, and effects upon psychological health6,7 – making it necessary to adopt a multidisciplinary approach to these cases in view of their complexity.
This new situation has led some hospitals to create tools for monitoring these complex patients. In this regard, specific circuits have been incorporated in different centers, along with special implication on the part of the Ítaca Group (collaborative and working group for the prevention, diagnosis, monitoring and treatment of patients with post-intensive care syndrome [PICS]), launching the CoronaPICS study at Spanish national level to describe the characteristics of PICS in COVID-19 survivors, among other objectives.
The present study examines the sequelae one month after hospital discharge among patients with severe bilateral pneumonia due to COVID-19 from a multidisciplinary approach involving Intensive Care Medicine, Physical Medicine and Rehabilitation, Endocrinology and Nutrition, Mental Health and Pulmonology. The studies available to date8 include COVID-19 survivors following admission to intensive care, with no distinction regarding the type of respiratory care provided during admission. The present study thus seeks to determine whether there are differences between patients subjected to high-flow oxygen therapy alone and those in which escalation to invasive mechanical ventilation is required.
Patients and methodsA prospective observational study was carried out among patients requiring admission to the ICU of Hospital Virgen de la Victoria (Málaga, Spain) in the period between April 2020 and October 2021 due to severe COVID-19 pneumonia. The patients admitted to the ICU were all amenable to aggressive measures, with oxygen requirements>15lpm and PaO2/FiO2<200.
The study included the survivors registered in the postCOVID Multidisciplinary Care circuit, who were assessed in a “single-step consultation” by Physical Medicine and Rehabilitation, Endocrinology, Pulmonology, Mental Health and Intensive Care Medicine.
We excluded patients referred from other hospitals, since our center is the reference hospital for the area of the Costa del Sol and Serranía de Ronda, and also foreign patients, due to difficulties in securing their follow-up.
The following information was recorded on the first visit, corresponding to one month after hospital discharge:
- •
Case history, with previous quality of life, independence for basic activities of daily living, need for walking aids, tiredness, physical exercise habits, pain and weakness.
- •
Data referred to admission: days of ICU and hospital stay, respiratory therapy used, days of IMV, treatment administered, days of muscle relaxation and cycles of prone decubitus.
- •
Sequelae: ear, nose and throat (ENT), psychological/psychiatric, use of benzodiazepines and antidepressants, oxygen therapy at discharge, dyspnea (modified Medical Research Council [mMRC] scale), spirometry, weight loss following admission to hospital, body cell mass (BCM) and body cell mass index (BCMI).
- •
Exploration: global joint balance and global muscle balance (mMRC scale), grip strength with hand dynamometer, respiratory muscle pressures: peak inspiratory pressure (Pimax) and peak expiratory pressure (Pemax), and 6-minute walking test (6MWT).
- •
Quality of life scales/questionnaires: FACIT-F, EuroQol-5D, Barthel scale. Montreal cognitive assessment (MoCA) test.
Following assessment of the patients, and if they presented a defect of some kind, they were invited to enter an on-site or home integral rehabilitation program (Fig. 1) based on the following characteristics:
The indications for the on-site rehabilitation program were:
- •
COVID-19 patients with a negative PCR test, able to walk without aids, stable, with dyspnea in response to moderate-major exertion and/or tiredness in response to moderate exertion, frailty with Short Physical Performance Battery (SPPB) score<10 and/or need for oxygen therapy.
- •
Good cognitive level and collaboration capacity.
The indications for the home rehabilitation program were:
- •
Frail patients with no need for oxygen therapy.
- •
Patients unable to attend the on-site rehabilitation program.
The study was carried out in abidance with the Declaration of Helsinki and the principles of Good Clinical Practice, and was approved by the Ethics Committee of Hospital Virgen de la Victoria (Málaga, Spain)(Project ref. POSTUCI21 - 1654-N-21).
Subject identity was kept confidential. Each patient was identified by a number, making it possible to link the data between the different consultations, and a database was generated from which to extrapolate the information and draw conclusions in the present study. The patients were duly informed of the descriptive nature of the study in terms of its baseline characteristics, and gave informed consent to the use of their anonymized data and to long-term monitoring. The patients were free to withdraw their consent at any time. Only one patient rejected the signing of consent to the analysis of the data obtained.
Statistical analysisThe demographic characteristics of the patients were reported as the mean and standard deviation (SD) in the case of continuous variables, and as absolute values and percentages in the case of categorical variables.
The participants were classified into two groups according to the respiratory therapy provided during admission to the ICU: high-flow nasal oxygen (HFNO) or invasive mechanical ventilation (IMV). The descriptive analysis of the sociodemographic and clinical parameters was carried out using the chi-square statistic for the equality of means and the Levene test for the quality of variances in the case of quantitative variables. The chi-square test was used in the case of qualitative variables, with application of the Fisher exact test where required, in order to determine possible statistically significant differences between the studied variables and the type of respiratory treatment provided, with a level of confidence of 95%.
A binomial logistic regression model was developed, with multivariate analysis to evaluate predictors of brachial plexopathy, limited muscle balance in the lower limbs, and distal neuropathy. Those variables showing a statistically significant association in the univariate analysis were entered into the multivariate analysis.
All analyses were made using the SPSS version 24 statistical package. Statistical significance was considered for P<.05.
ResultsA total of 360 patients were admitted to the ICU of Hospital Virgen de la Victoria (Málaga, Spain) in the period between April 2020 and October 2021. Of these, 104 were included in the post-COVID-19 multidisciplinary consultation. With regard to the remaining 256 patients, 127 died during hospital admission, 74 failed to meet the study inclusion criteria (28 individuals referred from other centers, 45 foreign patients, and a single subject who declined to participate in the monitoring phase), and 55 patients were lost to follow-up after hospital discharge.
The clinical and sociodemographic characteristics of the patients in relation to the respiratory treatment provided (HFNO or IMV) are shown in Table 1. Of the 56 patients subjected to IMV, 29 were intubated directly upon admission, 14 in the first 24h of admission, 7 at 48h of admission, and 6 after this time. High-flow nasal oxygen was the respiratory treatment prescribed prior to orotracheal intubation in all cases. There was a statistically significant difference (P<.001) in the number of days of ICU stay, with an average of 8.97 days (SD 3.86) in the patients subjected to HFNO versus 32.82 days (SD 21.03) in those subjected to IMV, as well as in the number of days of hospital stay, with an average of 24.12 (SD 16.72) and 67.23 (SD 59.06), respectively.
Baseline sociodemographic and clinical characteristics of the COVID-19 patients according to the respiratory treatment provided (high-flow nasal oxygen [HFNO] or invasive mechanical ventilation [IMV]).
| HFNO | IMV | P | |
|---|---|---|---|
| N=48 | N=56 | ||
| Age, mean (SD) | 56.43 (15.83) | 59.16 (10.45) | .312 |
| Over 60 years of age, n (%) | 23 (47.9) | 31 (55.4) | .449 |
| Gender | .512 | ||
| Male, n (%) | 36 (75) | 45 (80.4) | |
| Female, n (%) | 12 (25) | 11 (19.6) | |
| Comorbidity, n (%) | |||
| Arterial hypertension | 22 (45.8) | 28 (50) | .672 |
| Diabetes | 12 (25) | 17 (30.4) | .544 |
| Dyslipidemia | 14 (29.2) | 8 (32.1) | .743 |
| Smoking, n (%) | .250 | ||
| Non-smoker | 22 (45.8) | 32 (57.1) | |
| Smoker | 3 (6.3) | 1 (1.8) | |
| Ex-smoker | 23 (47.9) | 23 (41.1) | |
| History of respiratory disease, n (%) | 8 (16.7) | 15 (26.8) | .669 |
| COPD | 1 (2.1) | 2 (3.6) | |
| Asthma | 3 (6.3) | 6 (10.7) | |
| OSAS | 4 (8.3) | 7 (12.5) | |
| Kidney disease, n (%) | 1 (2.1) | 1 (1.8) | .712 |
| History of heart disease, n (%) | 6 (12.5) | 5 (8.9) | .555 |
| Ischemic heart disease | 2 (4.2) | 3 (5.4) | |
| Arrhythmias | 2 (4.2) | 1 (1.8) | |
| Valve disease | 1 (2.1) | 1 (1.8) | |
| Others | 1 (2.1) | 0 (0) | |
| History of orthopedic disease, n (%) | 3 (6.3) | 5 (8.9) | .447 |
| Previous fractures | 1 (2.1) | 3 (5.4) | |
| Osteoarthritis | 1 (2.1) | 0 (0) | |
| Myalgia | 0 (0) | 1 (1.8) | |
| Arthrosis | 1 (2.1) | 1 (1.8) | |
| BMI, n (%) | .326 | ||
| Normal (18.5−24.9) | 5 (10.4) | 2 (3.6) | |
| Overweight (25−29.9) | 13 (27.1) | 18 (32.1) | |
| Obesity 1 (30−34.9) | 12 (25) | 20 (35.7) | |
| Obesity 2 (35−39.9) | 11 (22.9) | 7 (12.5) | |
| Morbid obesity (>40) | 7 (14.6) | 9 (16.1) | |
| BMI, mean (SD) | 32.85 (6.87) | 33.05 (7.10) | .885 |
| APACHE score, mean (SD) | 8.18 (3.17) | 9.07 (4.41) | .284 |
Abbreviations: N: number of patients; SD: standard deviation; COPD: chronic obstructive pulmonary disease; OSAS: obstructive sleep apnea syndrome; BMI: body mass index.
The APACHE II was similar in both groups, with an average of 8.18 (SD 3.17) in the HFNO group versus 9.07 (SD 4.41) in the IMV group.
The symptoms one month after hospital discharge are reported in Table 2. There were differences between the two ventilatory assist groups in terms of the ear, nose and throat sequelae, with the observation of cases of aphonia, glottic granuloma, tracheal stenosis, hypoacusia and tracheostomy fistula in the IMV group.
Symptoms detected one month after hospital discharge.
| HFNO | IMV | P | |
|---|---|---|---|
| N=48 | N=56 | ||
| Post-ICU weight loss (kg), mean (SD) | 8.54 (4.59) | 13.64 (8.78) | <.001 |
| BCM (kg), mean (SD) | 31.96 (8.74) | 26.87 (6.84) | .007 |
| BCMI (kg/m2), mean (SD) | 11.16 (2.83) | 9.20 (2.15) | .001 |
| ENT, n (%) | 1 (2.1) | 22 (39.3) | .001 |
| Psychological/psychiatric disorders, n (%) | 17 (35.42) | 23 (41.07) | .350 |
| Insomnia, n (%) | 11 (22.91) | 16 (28.57) | .512 |
| Use of benzodiazepines, n (%) | 11 (22.91) | 19 (33.93) | .217 |
| Use of antidepressants, n (%) | 10 (20.83) | 18 (32.14) | .195 |
| Dyspnea mMRC, n (%) | .267 | ||
| Grade 0 | 19 (39.6) | 18 (32.1) | |
| Grade 1 | 18 (37.5) | 15 (26.8) | |
| Grade 2 | 8 (16.7) | 17 (30.4) | |
| Grade 3 | 3 (6.3) | 6 (10.7) | |
| Home oxygen therapy, n (%) at hospital discharge | 22 (45.8) | 17 (30.4) | .104 |
| Joint balance, n (%) normal | 31 (88.6) | 35 (71.4) | .059 |
| Muscle balance, n (%) normal | 27 (77.1) | 24 (49) | .009 |
| Pain disorders, n (%) | 14 (29.2) | 22 (39.3) | .633 |
| Brachial plexopathy, n (%) | 0 (0) | 6 (10.7) | .024 |
| Distal neuropathy, n (%) | 5 (10.4) | 19 (33.9) | .005 |
| Equinovarus, n (%) | 2 (4.3) | 6 (10.71) | .260 |
| Aids, n (%) | |||
| No aids | 43 (89.6) | 42 (75) | |
| Stick/walker | 3 (6.3) | 13 (23.2) | |
| Wheelchair | 2 (4.2) | 1 (1.8) | .055 |
| MoCA, mean (SD) | 19.5 (10.31) | 20.52 (8.77) | .741 |
| Fatigue/tiredness, n (%) | 34 (70.8) | 45 (84.9) | .087 |
Abbreviations: BCM: body cell mass – total body mass; BCMI: body cell mass index – total body mass index; ENT: ear, nose and throat; mMRC: modified Medical Research Council dyspnea score; MoCA: Montreal cognitive assessment score.
The physical sequelae showing significant differences between the groups in the rehabilitation clinic were distal neuropathy (P=.005) and the limitation of muscle balance in the lower limbs (P=.024). Brachial plexopathy was only observed in the IMV group (P=.024). There were no differences in terms of the pain conditions evaluated (arm-neck pain, neuropathic pain, lumbosciatic pain, facet syndrome, multiple enthesopathy and meralgia paresthetica).
On occasion of the first rehabilitation visit (Table 3), the patients underwent a walking test, the measurement of Pimax and Pemax, and a grip strength test. Males obtained better results (P=.010) in terms of Pimax in the HFNO group, with an average of 112.10 cmH2O (SD 33.04 cmH2O), versus 89.81 cmH2O (SD 34.71 cmH2O) in the IMV group. The isometric grip test using hand dynamometry evidenced a decrease, with a mean right-hand grip strength of 20.67kg (±8.27) in the IMV group versus 31.8kg (±11.59) in the HFNO group, and a mean left-hand grip strength of 19.39kg (±8.45) in the IMV group versus 30.26kg (±12.74) in the HFNO group.
Functional tests: Rehabilitation. Walking test and grip test. Respiratory function tests: spirometry and respiratory pressures.
| HFNO | IMV | P | |
|---|---|---|---|
| Walking test, n (%) | N=16 | N=30 | .220 |
| Normal distance | 12 (75) | 17 (56.7) | |
| Distance<350m | 4 (25) | 13 (43.3) | |
| Stops, n (%) | N=30 | N=30 | .83 |
| 0 | 14 (87.5) | 26 (86.7) | |
| 1 | 1 (6.3) | 3 (10) | |
| 2 or more | 1 (6.3) | 1 (3.3) | |
| Oxygen, n (%) | 1 (6.3) | 2 (6.7) | .726 |
| Hand dynamometer (kg), mean (SD) | N = 35 | N = 46 | |
| Right hand (kg) | 31.8 (11.59) | 20.67 (8.27) | <.001 |
| Left hand (kg) | 30.26 (12.74) | 19.39 (8.45) | <.001 |
| Spirometry | N = 32 | N = 34 | |
| FVC (%), mean (SD) | 85.57 (17.61) | 90.80 (27.49) | .389 |
| FEV1, mean (SD) | 87.31 (17.99) | 89.03 (20.22) | .724 |
| FEV1/FVC, mean (SD) | 82.34 (8.43) | 84.16 (15.26) | .549 |
| Respiratory pressures | |||
| Males | N = 28 | N = 38 | |
| Pimax, mean (SD) | 112.10 (33.04) | 89.81 (34.71) | .010 |
| Pemax, mean (SD) | 107 (27.38) | 97.07 (28.34) | .166 |
| Females | N = 9 | N = 8 | |
| Pimax, mean (SD) | 76.22 (45.88) | 62.25 (19.52) | .423 |
| Pemax, mean (SD) | 72.66 (19.15) | 74.12 (25.82) | .898 |
Abbreviations: FVC: forced vital capacity; FEV1: forced expiratory volume in the first second; FEV1/FVC; Pimax: Peak inspiratory pressure; Pemax: peak expiratory pressure.
Of the 104 patients subjected to multidisciplinary post-ICU monitoring, 23 did not require rehabilitation. With regard to the remaining 81 patients, 36.54% required group rehabilitation and 41.35% home rehabilitation (P=.056).
In relation to the other scales used, the Barthel index was 95.28 points (SD 14.44) in the HFNO group and 89.12 points (SD 20.70) in the IMV group. The EuroQol-5D in turn showed a statistically significant difference in terms of perceived quality of life at 6 months between the two groups (P=.004), with no differences at the first control visit (P=.301) or in terms of the rest of the items assessed by this index. The FACIT-F likewise showed no significant differences at 6 months (P=.099).
The multivariate analysis (Table 4) performed to explore risk factors associated with brachial plexopathy, limited muscle balance in the lower limbs and distal neuropathy revealed no significant correlations.
Multivariate analysis of risk factors associated to brachial plexopathy (A), limited muscle balance in the lower limbs (B), and distal neuropathy (C).
| 1. Brachial plexopathy | ||
|---|---|---|
| OR (95%CI) | P | |
| Weight loss (kg) in ICU | 1.046 (0.953−1.147) | .344 |
| Prone decubitus | 1.175 (0.779−1.771) | .443 |
| 2. Limited muscle balance in the lower limbs | ||
|---|---|---|
| OR (95%CI) | P | |
| Age | 1.045 (0.977−1.117) | .199 |
| BCMI | 0.803 (0.570−1.130) | .208 |
| Days of ICU stay | 0.986 (0.943−1.030) | .515 |
| Prone decubitus | 1.248 (0.888−1.755) | .202 |
| HFNO/IMV | 2.417 (0.334−17.504) | .385 |
| 3. Distal neuropathy | ||
|---|---|---|
| OR (95%CI) | P | |
| Tracheostomy | 7.988 (0.923−69.107) | .059 |
| Weight loss (kg) in ICU | 1.088 (0.988−1.198) | .088 |
| Days of ICU stay | 0.850 (0.701−1.031) | .100 |
| Days of hospital stay | 1.016 (0.995−1.037) | .127 |
| Days of mechanical ventilation | 1.126 (0.949−1.336) | .174 |
| Prone decubitus | 1.153 (0.819−1.624) | .415 |
The present study evidenced no statistically significant differences in the perceived physical sequelae following hospital discharge according to the respiratory treatment provided (prolonged IMV or HFNO). Likewise, no significant differences were recorded among the patients requiring rehabilitation. Despite the absence of statistical significance, however, over twice as many patients in the IMV group required group rehabilitation compared with the HFNO group – this possibly generating uncertainty regarding the results obtained. The home rehabilitation protocol was the same as the on-site protocol, except for supervision by a physiotherapist in the latter case. This resulted in more individualized treatment as well as patient commitment to come to the rehabilitation sessions, a positive attitude towards the program, and good adherence. In the case of the home program there was no supervision, and rehabilitation fundamentally depended on patient awareness of the need for the treatment.
From the respiratory perspective, practically twice as many patients in the IMV group presented mMRC grade 2–3 dyspnea. Of note was the absence of statistical significance regarding the need for oxygen therapy at discharge, with no lesser percentage in the HFNO group versus the IMV group. These findings are interesting and may give rise to hypotheses regarding the duration of distress and lung repair time. The fact that the patients subjected to high-flow therapy9 showed no significant differences versus the IMV group basically raises two hypotheses: (a) lesser duration of stay in intensive care and a shorter total hospital stay, spending the last days of respiratory distress at home; and (b) noninvasive support involving a risk of lung damage self-inflicted by the patients, with a negative impact upon the perceived symptoms.10,11
The present study was carried out to explore the possible differences in terms of patient sequelae according to the type of respiratory care provided during admission to the ICU, since few studies have established direct comparisons between the two groups, and no recommendations have been established regarding the ideal moment to start HFNO and its possible effects.12,13 In the studies found in the literature, ICU survivors had dyspnea and lung function scores similar to those of patients not requiring admission to the ICU, despite poorer results in the computed tomography (CT) scans and poorer performance in terms of activities of daily living.14 With regard to the respiratory function tests based on Pimax and Pemax, and maximum ventilatory volume, studies have focused on different patient profiles,22,23 with the observation of correlations between grip strength as an indicator of peripheral muscle strength and respiratory muscle strength compared with healthy subjects. Our study recorded significant differences in the number of days of ICU and hospital stay according to the type of respiratory treatment required during admission (P<.001), with no differences in the respiratory tests performed, such as spirometry (FVC, FEV1 and FEV1/FVC). Significant differences were only recorded for Pimax among male patients.
Post-intensive care syndrome17–19 is characterized by clinically significant depressive symptoms, anxiety and posttraumatic stress,20 with the coining of terms such as post-COVID-19 syndrome, persistent post-COVID-19 syndrome (PPCS) or prolonged COVID-19.21 Studies have been carried out on the quality of life or sequelae following hospital discharge in non-critical COVID-19 pneumonia cases,22 examining the impact of the condition on lung function, health-related quality of life, and perceived dyspnea. There have been descriptions of the appearance of cognitive impairment in mild symptomatic COVID-19, evaluated with the MoCA test, though the pathogenesis underlying this complication is not clear.3 With regard to the impact upon daily quality of life as assessed with the EuroQol-5D-5L, differences have been recorded4 in ICU survivors versus mild to moderate cases. Other studies23 have evidenced alterations in terms of mobility, self-care, pain, anxiety or depression and routine activities in both groups, with a slight difference in pain in the ICU group.
Rehabilitation is crucial in the multidisciplinary monitoring of patients after hospital discharge24 to facilitate recovery from serious conditions associated with COVID-19, optimize patient independence and facilitate reintegration within the community. Early rehabilitation should be encouraged in this regard.25–27 Our study recorded an association between IMV and brachial plexopathy, distal neuropathy and limited muscle balance in the lower limbs. The multivariate analysis evidenced no statistically significant differences, however.
From the nutritional perspective, significant differences were observed in body cell mass (BCM) and body cell mass index (BCMI)28 in patients requiring IMV, though the findings seem to be related to a longer ICU and hospital stay, resulting in poorer nutritional outcomes in these patients.
The main limitations of the present study are the small sample size involved and the fact that not all the patients were evaluated by all the specialists included in the multidisciplinary program – certain tests (e.g., spirometry) having been limited to those patients with a poorer respiratory outcome at hospital discharge.
Unfortunately, many patients were excluded from the study because our hospital is a reference center for other healthcare areas. Specifically, 74 patients were excluded because they were referred from other hospitals or were foreigners that returned to their countries of origin. In addition, 55 patients were not included in the study due to a lack of information about their sequelae one month after hospital discharge – this situation probably being a consequence of the closing of the post-COVID-19 consultation agendas in the third wave of the pandemic, in January 2021.
Another factor to be taken into account is the medication administered during admission. In this regard, while there were no differences in relation to dexamethasone and tocilizumab, other drugs, specifically lopinavir/ritonavir and hydroxychloroquine, were fundamentally prescribed in patients subjected to IMV. This could generate bias, though on 4 July 2020 these drugs were disadvised by the WHO, accepting the recommendation of the international steering committee of the Solidarity trial, whereby the decrease in mortality among COVID-19 patients did not justify their use. The same applied to interferon beta-1A, which showed no evidence or data indicating a decrease in mortality and/or need for mechanical ventilation.29 Therefore, we do not consider that such treatment in the patients selected during the first wave of the pandemic could have generated bias between the two groups.
Long-term monitoring periods are necessary, involving larger sample sizes, in order to better characterize the consequences of COVID-19.
ConclusionsThe results obtained after the multivariate analysis suggest that there are no statistically significant differences in perceived physical sequelae following hospital discharge according to the respiratory therapy used (HFNO or prolonged mechanical ventilation), though more studies are needed in order to draw firmer conclusions.
Author contributionsMultidisciplinary consultation involved the Departments of Intensive Care Medicine, Physical Medicine and Rehabilitation, Endocrinology and Nutrition, Mental Health and Pulmonology.
The contributors of the different Departments were Dr. José M. García Almeida as specialist in Endocrinology and Nutrition; Dr. Elma Avanesi-Molina as specialist in Mental Health; Dr. Eva Cabrera-César as specialist in Pulmonology; Dr. Pilar Martínez-López as specialist in Intensive Care Medicine; and Adela M. Gómez-González as specialist in Physical Medicine and Rehabilitation.
The article was supervised by Dr. Pilar Martínez-López and Dr. Adela M. Gómez-González, as main creators of the post-COVID-19 consultation, with the collaboration of the hospital Medical Director, Dr. Maria A. Estecha-Foncea. The development of the project, literature search, discussion and conclusions were conducted by Dr. Ana M. Sánchez-García, with external review by Dr. Pedro L. Sánchez-Fernández, Dr. Manuel F. Jiménez-Navarro and Dr. María A. Estecha-Foncea. The Dr.s Nicolás Zamboshi, Carolina Rueda-Molina, Victoria Doncel-Abad, Ana I. Molina-Ramos, Imad Ben-Abdellatif, Marina Gordillo-Resina and Esteban Pérez-Mesa contributed to data compilation. The telephone survey was made by Dr.s Maria Nieto-González, Pilar Nuevo-Ortega and Carmen Reina-Artacho.
The statistical analysis of the data was performed by Dr. Jorge Rodriguez-Capitán and Dr. Rafael J. Jiménez-López.
The corresponding author is Dr. Manuel F. Jiménez-Navarro, belonging to the Instituto de Investigación Biomédica de Málaga (IBIMA), University of Málaga (UMA)(Málaga, Spain).
Conflicts of interestThe authors declare that they have no conflicts of interest.