Ventilator-associated pneumonia (VAP) is a frequent cause of morbidity–mortality in critical patients, and is responsible for over 50% of the antibiotics (ATBs) used in the Intensive Care Unit (ICU).1–3
According to the Spanish National Surveillance Study on Nosocomial Infections in the ICU, associated to the European project Hospitals in Europe Link for Infection Control through Surveillance (ENVIN/HELICS) of 2013,4 the number of patients who have suffered some infection in the ICU has gradually decreased over the years from 15.5% in 2009 to 10.6% in 2013. The report underscores the notorious drop in VAP rate, from 11.4 episodes per 1000 days on mechanical ventilation (MV) in 2009 to 6.87 episodes per 1000 days on MV in 2013. On analyzing the successive ENVIN/HELICS reports, we observe a decrease in the number of patients treated with ATBs for infections acquired in the ICU, from 25.78% in 2009 to 20.88% in 2013. However, the total number of patients receiving ATBs remained stable during these years, with rates of between 60% (2010) and 63% (2013). This situation does not seem to correspond to a purely local phenomenon. Recently, Wunderink5 pointed out that the apparent decrease in the incidence of VAP is not correlated to the corresponding decrease in ATB use or mortality in the United States. The explanation for this discrepancy could be the use of ATBs for the management of scantly defined disease conditions different from VAP. In this context, and considering the new surveillance classification proposed by the United States Centers for Disease Control and Prevention referred to events associated to MV,6 the frequency of use of ATBs in the ICU could in fact be higher. Ventilator-associated tracheobronchitis (VAT) is considered to be common in ventilated patients, as evidenced by a recent international survey.7 An interesting finding of this survey is that carbapenems were the most frequent initial empirical treatment in such patients. These results are reinforced by the findings of the ENVIN/HELICS program. According to data from 2013, a total of 1275 antibiotic treatments were administered to treat VAT, with a mean duration of 7.77 days, and a total of 9912 days of ATBs. These figures are similar to those published for VAP, with the administration of 1118 antimicrobial treatments, with a mean duration of 9.11 days, and a total of 10,188 days of ATBs.4
Taking into account the fact that microbial resistance levels are directly related to the amount of ATBs used,8,9 together with the almost certain existence of an overdiagnosis of ventilator-associated infections, including VAP,10 adequate antimicrobial use is a fundamental objective in order to define strategies for avoiding the development of resistances.
In this context, nebulized ATBs could be a valid option for the treatment of infectious complications associated to MV, such as VAT or even VAP.6 The possible use of this type of ATB treatment is based on the idea that an adequate nebulization technique is able to directly release the ATB at the site of infection and reach very high concentrations, with minimum systemic toxicity and effects upon the intestinal flora, and can contribute to reduce the appearance of resistances.11–13 To date, the international guides1 only mention the use of nebulized aminoglycosides or polymyxin as coadjuvant therapy in pneumonia caused by multiresistant gramnegative bacilli that fails to respond adequately to systemic therapy. In this context we should ask ourselves whether this is the only possible scenario for the use of nebulized ATB, or whether there are also other clinical situations in which the use of these formulations may be justified, despite the lack of solid supporting scientific evidence.
In patients suffering from cystic fibrosis, with chronic airway infection/colonization, the use of nebulized ATBs has been associated to a decrease in the number of hospital admissions due to exacerbations, and to improved lung function.14–17 Based on these observations, the ATBs used in nebulized formulations (tobramycin, colistin and aztreonam) have been approved by the different health authorities only for use in this special group of patients. However, the characteristics of the airway in ventilated patients who develop tracheobronchial infection/colonization (as for example in VAT) are similar to those of patients with cystic fibrosis. Both groups of patients have an altered and inflamed respiratory epithelium, with different degrees of infection/colonization. Furthermore, it is now recognized that biofilm development in the endotracheal tube may be similar to that seen in the airway of patients with cystic fibrosis.18,19 This situation favors resistance to ATB treatment on the part of certain microorganisms such as Pseudomonas aeruginosa or Staphylococcus aureus – the main causes of respiratory infections in both groups of patients.11,20–22
However, nebulized ATBs for the treatment of infectious complications related to MV continue to be prescribed on a “compassionate use” basis. The first studies carried out in the 1970s23,24 with polymyxin B through instillation and an atomizer observed an increase in VAP attributable to microorganisms resistant to polymyxin. Although these same investigators demonstrated that this complication could have been due to the prolonged use of polymyxin B, the findings generated great uncertainty among clinicians, and no further studies were made over the next 30 years. Although the instillation of ATBs results in a high drug concentration in tracheal secretions,25 the distribution of the antibiotic is not homogeneous, and the amount distributed within the alveoli is not known.26 In contrast, nebulization generates particles of smaller size and thus offers the theoretical advantage of producing a more homogeneous distribution of the drug throughout the lower airway. The findings of studies in animals27,28 reveal high ATB concentrations in lung tissue, in the distal airway, and in the alveoli. A recent study29 involving 69 ventilated patients with VAP produced by gramnegative bacilli found nebulized amikacin to be adequately distributed within the lung tissues–with high tracheal concentrations reaching 16.2mg/ml upon administering 400mg every 12h.
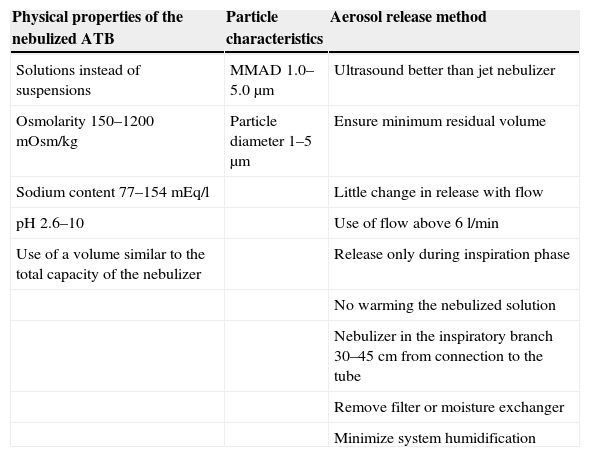
Despite these results, the main concern of intensivists in using nebulized ATBs refers to the capacity of the drug to penetrate the lung tissues. Although tissue penetration is good in healthy volunteers,30 it is less certain in patients with lung tissue consolidation. Animal models23 evidence good nebulized amikacin concentrations even in poorly ventilated areas. Luyt et al.31 recorded a high concentration of amikacin in lung consolidation zones among patients with VAP due to gramnegative bacilli. Although in most cases the concentrations obtained in alveolar fluid are far above the minimum inhibitory concentration of the main pathogens responsible for VAP, such concentrations appear to be closely related to the quality of nebulization and the type of nebulizer used.32,33 The “ideal” and “safe” conditions described in Table 1 appear to be easy to reach with modern nebulizers–particularly the vibration (ultrasound) devices.32,33 Compliance with these conditions is essential if we wish not only to reach the treatment objectives but also to avoid serious complications such as severe bronchospasm produced by the nebulization of substances not suited to this administration route. On the other hand, Lu et al.,34 in a phase II trial, found that amikacin and ceftazidime treatment administered via the intravenous route or in nebulized formulation exhibits similar efficacy in patients with VAP due to sensitive Pseudomonas aeruginosa strains. Notoriously, and although the clinical failure rate was similar in both groups, the persistence of colonization or recurrence due to resistant microorganisms was only observed in the intravenous treatment group.
“Ideal” characteristics in order to adequately administer nebulized antibiotics and avoid complications.
| Physical properties of the nebulized ATB | Particle characteristics | Aerosol release method |
|---|---|---|
| Solutions instead of suspensions | MMAD 1.0–5.0μm | Ultrasound better than jet nebulizer |
| Osmolarity 150–1200mOsm/kg | Particle diameter 1–5μm | Ensure minimum residual volume |
| Sodium content 77–154mEq/l | Little change in release with flow | |
| pH 2.6–10 | Use of flow above 6l/min | |
| Use of a volume similar to the total capacity of the nebulizer | Release only during inspiration phase | |
| No warming the nebulized solution | ||
| Nebulizer in the inspiratory branch 30–45cm from connection to the tube | ||
| Remove filter or moisture exchanger | ||
| Minimize system humidification |
Different studies in critical patients35–38 have shown that nebulized ATBs may be an adequate option as coadjuvant treatment for VAP produced by multiresistant bacilli. A particularly interesting study is that published by Kwa et al.,38 who recorded a favorable clinical response in 85.7% of the patients with VAP due to multiresistant bacilli administered nebulized colistin as sole ATB treatment.
Although the evidence on VAP management with nebulized ATBs is admittedly scarce in reference to the adequacy or inadequacy of nebulized drug penetration capacity in consolidated lung tissues, another frequent complication of MV, specifically VAT (an infection limited to the airway), could also be a clear target for treatment with nebulized ATBs, affording good clinical resolution.39–41 This type of treatment strategy could significantly lessen the use of broad spectrum ATBs via the systemic route in patients with this disorder (over 9900 days of ATB treatment according to data from the ENVIN-HELICS). Furthermore, we must remember that systemic ATBs are associated to low drug levels in alveolar fluid, as well as to strong pressure upon the local flora and the appearance of multiresistance phenomena.
Lastly, there is no doubt that well designed studies are needed to confirm the above considerations. Our opinion is that on the basis of the existing evidence, the treatment of VAT with nebulized ATBs could reduce the development of VAP and the need for systemic antibiotics. However, the impact of this strategy in terms of a decrease in multiresistance phenomena remains to be evaluated in the context of future studies.
FundingThis study has been financed in part by grants FIS PI13/02011 and AGAUR 2014/SGR926.
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to this study.
AR has received compensation for conferences on behalf of Pfizer, Gilead, Astellas, Novartis, Thermo-Fisher Roche and MSD.
FB has received compensation for conferences on behalf of Pfizer, Astellas, Novartis and MSD.
Please cite this article as: Rodríguez A, Barcenilla F. Antibióticos nebulizados. ¿Una opción adecuada para el tratamiento de la infección respiratoria relacionada con la ventilación mecánica? Med Intensiva. 2015;39:97–100.