In 2015, a new paediatric Acute Respiratory Distress Syndrome (PARDS) definition was published by the Paediatric Acute Lung Injury Consensus Conference (PALICC).1 Contrary to the previous conferences (AECC Barcelona 1994, Berlin 2012),2,3 in this new definition the findings of bilateral infiltrates in the chest imaging is not required, with the appearance of unilateral infiltrates being sufficient. PALICC investigators considered this a point of recommendation because of the lack of evidence of a different outcome in PARDS patients. We report here two patients who have been diagnosed with PARDS using the new definition, but whose outcome did not correspond with the evolution normally expected in patients with this clinical entity.
From November 2011 to December 2015 71 infants from 0 to 12 months old with acute respiratory failure (ARF) required interhospital ground transport with continuous positive airway pressure (CPAP) to the Paediatric Intensive Care Units (PICU) of two tertiary-care hospitals. Infants with neonatal pathologies were excluded. The details of this retrospective cohort of patients have been published elsewere.4 In summary, the causes for ARF were: bronchiolitis (76.1%), wheezing episode (19.7%) and pneumonia (4.2%). No patients required change in the respiratory support or endotracheal intubation during interhospital transport. The maximum respiratory support at PICU were: 1.4% (n=1) high flow nasal cannula, 54.9% (n=39) CPAP, 36.6% (n=26) bilevel positive airway pressure and 5.1% (n=2) invasive mechanical ventilation. None of the patients died. Because patients with transcutaneous oxygen saturation values higher than 97% were excluded,5 the ratio saturation measured via pulse oximetry to fraction of inspired oxygen (S/F ratio) in the referral hospital was calculated in 74.6% (n=53) of patients, while in the PICU it was calculated in 39.4% (n=28) of the cases. The mean±SD S/F before transfer was 322.4±109.3 and upon arrival at PICU 300.6±93.8 (p=0.033), decreasing a median of 59 points during transfer.
The S/F ratio prior to transfer was ≤150 in 4 infants (128.8±27.6), who were diagnosed with bronchiolitis. Chest radiography was performed in only two of these patients and in both the presence of unilateral infiltrates was seen. Their S/F prior to transfer was 136.7±18.6. Both infants were transferred with Helmet interface and Boussignac® CPAP (Vygon, Ecouen, France). They both received CPAP as respiratory support in PICU. These patients did not present cyanotic heart disease or chronic lung disease. Using Kaplan–Meier analysis, no differences were found in duration of total (i.e. invasive and non-invasive) ventilation between these two patients and the rest of the population: 3 [95% CI: 3–-] days for patients with S/F ≤150 and unilateral infiltrates vs. 2 [95% CI: 1.3–5] for the rest (Log Rank test, p=0.930). The median length of stay in PICU was 3.5 [95% CI: 3.5–-] days for patients with S/F ≤150 and unilateral infiltrates vs. 4 [95% CI: 3–7] for the rest (Log Rank test, p=0.259).
A good correlation between the partial pressure of oxygen/fraction of inspired oxygen ratio and the S/F has been demonstrated.5 A ratio S/F ≤150 is required for the diagnosis of severe ARDS, and it is independently associated with the need for endotracheal intubation.6 Invasive ventilation was not initiated in patients with S/F ratio before transfer ≤150 and unilateral infiltrate because they did not meet ARDS criteria according to the current definitions at that time.2,3 In agreement with the new PALICC criteria, the referred patients fulfilled the PARDS definition. Invasive ventilation might have been considered as mandatory respiratory support during transport and in PICU. However, these patients presented a favourable evolution, without the need for endotracheal intubation or a longer duration of ventilatory support or PICU length of stay.
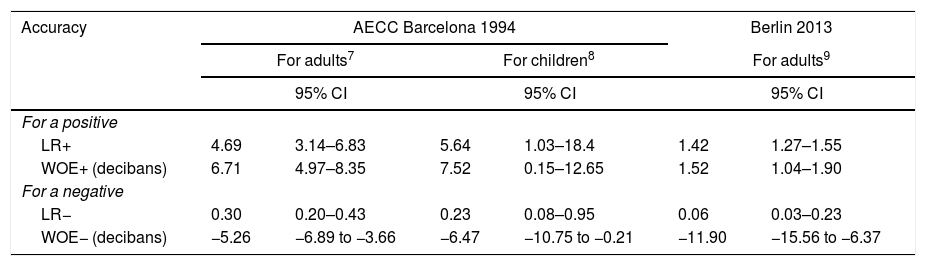
Using autopsy findings as the gold standard, AECC Barcelona definition showed good diagnostic accuracy (Table 1). In adults, the Turig-Good weight of evidence (WOE) was 6.71 decibans (dB) for a positive result, and for a negative result WOE was −5.26dB7; and in children, the WOE for a positive was 7.52dB and for a negative was −6.47dB.8 In order to gain clinical usefulness, the Berlin definition lost accuracy in confirming ARDS diagnosis (for a positive the WOE was only 1.52dB), but retained accuracy in discarding what is NOT an ARDS: WOE for a negative was −11.90dB (95% CI=−15.56 to −6.37).9
| Accuracy | AECC Barcelona 1994 | Berlin 2013 | ||||
|---|---|---|---|---|---|---|
| For adults7 | For children8 | For adults9 | ||||
| 95% CI | 95% CI | 95% CI | ||||
| For a positive | ||||||
| LR+ | 4.69 | 3.14–6.83 | 5.64 | 1.03–18.4 | 1.42 | 1.27–1.55 |
| WOE+ (decibans) | 6.71 | 4.97–8.35 | 7.52 | 0.15–12.65 | 1.52 | 1.04–1.90 |
| For a negative | ||||||
| LR− | 0.30 | 0.20–0.43 | 0.23 | 0.08–0.95 | 0.06 | 0.03–0.23 |
| WOE− (decibans) | −5.26 | −6.89 to −3.66 | −6.47 | −10.75 to −0.21 | −11.90 | −15.56 to −6.37 |
LR: Likelihood Ratio; WOE: Turing-Good weight of evidence; 95% CI: 95% confidence interval.
Because of this clinical observation, in our opinion the PALICC definition is susceptible to producing false positive rates, so the finding of bilateral infiltrates should be reconsidered as an essential tool for the diagnosis of PARDS. If we follow the new paediatric recommendations, only unilateral pulmonary infiltrates on chest radiograph, we will lose the base of our best knowledge: how to know, accurately and confidently, which hypoxaemic respiratory failure is NOT an ARDS.10 We consider the finding of unilateral infiltrates a point of controversy that requires further validation in prospective cohort studies.
FundingThis research did not receive any specific grant from funding agencies in the public commercial, or not-for-profit sectors.
Conflict of interestThe authors declare no conflict of interest.