Non-invasive ventilatory support (non-invasive ventilation, high-flow oxygen therapy, and CPAP) is useful in patients with heart failure and decompensated chronic obstructive pulmonary disease,1 but not that much in pneumonia.2
The current coronavirus pandemic (COVID-19) presents as a bilateral pneumonia with rapidly progressive respiratory failure and a high need for invasive ventilatory support. During the first pandemic wave of COVID-19 in Spain and due to the lack of ventilators, patients had to remain on non-invasive support until ventilators became available.
Anticipating the high probability of new pandemics in the future, it is of paramount importance to know whether sparing invasive ventilation only for end-stage patients is effective.
We present the experience of 22 Spanish hospitals during the first pandemic wave of COVID-19 (from March 1, 2020 through May 30, 2020). Adult patients admitted in the ICU, semi-critical care or pneumology ward setting with COVID-19 related moderate/severe respiratory failure (PaO2 < 80 or SpO2 < 90 with a FiO2 > 0.40) were included. Each center research ethics committee omitted the need for informed consent forms due to the observational nature of the study.
A total of 876 patients were analyzed. Of these patients, 615 (70%) required intubation. A total of 238 (39%) died, which is representative of a 27% overall mortality rate in this group. Mean age was 61 ± 12 years being a factor associated with the need for invasive ventilation and mortality (see Appendix B electronic additional data).
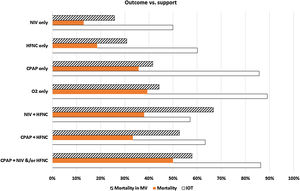
These were the ventilatory support systems used: HFNC in 431 patients (49%), oxygen therapy in 282 patients (32%), NIV in 62 patients (7%), and CPAP in 28 (3%). The combined use of these ventilatory support systems was far less common: CPAP + HFNC in 30 patients (3%), NIV + HFNC in 21 patients (3%), and CPAP + NIV with or without HFNC in 22 patients (3%). Fig. 1 shows the MV, overall mortality, and mortality rates in patients on MV.
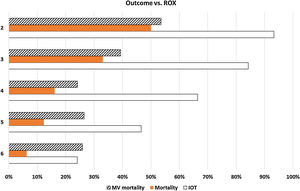
In patients who received HFNC, the ROX index (SpO2/FiO2/respiratory frequency) at the maximum FiO2 reached there was an inverse relationship with the need for intubation (Fig. 2). Patients with ROX indices ≥6, 5, 4, 3, and 2 required intubation 24%, 47%, 66%, 84%, and 93% of the times, respectively. Mortality was higher with ROX indices ≥6, 5, 4, 3, and 2 in 6%, 12%, 16%, 33%, and 50% of the cases, respectively. The mortality rate of patients on MV was similar with ROX indices ≥6 (26%), 5 (26%), and 4 (24%), but higher with ROX indices of 3 (39%), and 2 (54%). The ROX index is a marker of severity and need for MV, but it is not used within the first 24 h,3 but with the worst oxygenation data. Therefore, in many cases, these were the data available prior to intubation. Thus, the very high rates of intubation and mortality in patients with ROX indices of 2 or 3 suggest that, if possible, patients should be intubated before reaching such severe indices.
Only in patients treated with HFNC the sample was large enough to be able to build a logistics regression multivariable model associated with mortality at the ICU setting. The variables that were eventually significant were age (OR, 1.09 [1.06–1.12]), the ROX index (OR, 0.65 [0.51−0.81]), and a worse SpO2 (OR, 0.92 [0.88−0.98]). Using regression coefficients, the anticipated mortality rate was assessed and compared with the one actually seen (Appendix B Fig. 1 of Supplementary data). Thus, 4 groups of higher risk were defined to help us make more informed decisions.
An unexpected twist was the huge amount of healthcare professionals who suggested the prone position to their patients during spontaneous breathing since it only proved effective for the management of acute respiratory distress syndromes treated with mechanical ventilation.4 A total of 225 patients (27%) were placed in the prone position and 136 (60%) of these showed clinical improvement. The progression of patients in the prone position was similar to those who remained in other positions with respect to intubation (56% vs 68%), mortality (22% vs 26%), and mortality after being treated with invasive ventilation (39% vs 38%). There was a significant difference between those who improved and those who did not, both regarding intubation (40% vs 80%) and mortality (14% vs 34%) with a similar mortality rate among those who required invasive ventilation (35% vs 42%).
All these data should be put into context since they were results obtained in the middle of a pandemic with saturated healthcare services and improvised healthcare areas that lacked the necessary technical resources often with medical personnel and nursing staff who were not experts. None of the treatments were randomized, but instead based on the clinicians’ best judgment, and on the availability of resources and equipment or bed monitoring systems. Disease severity cannot be adjusted either beyond the inclusion criterion of moderate-to-severe respiratory failure.
Also, non-invasive methods could not be tried with the most critically ill patients who required emergency intubations. The decubitus position could not be proposed either when the nursing ratio was so low. Patients who only received oxygen therapy included apparently less critical patients, catastrophic patients, and others whose doctors decided not to use any sort of non-invasive support due to the lack of scientific evidence available or because it would only delay intubation with the corresponding associated morbidity and mortality.
While the mortality rate of intubated patients is similar after using HFNC or NIV, it actually seems that using CPAP or combined methods would only serve to delay intubation with the corresponding deleterious effects for the patients.5–7 In any case, whether this morbidity and mortality would somehow be accepted as a way to «buy extra time» is still under discussion until the proper mechanical ventilators are available since there are data available that suggest that the use of alternative ventilators (anesthesiology control tower systems, portable ventilators) may be associated with a higher mortality rate.8,9
In conclusion, with the data collected we can say that the use of NIV or HFNC is somehow beneficial on the CPAP or the standard oxygen therapy; however, trying different alternatives when one support fails probably only delays intubation with the corresponding added morbidity and mortality. The prone position during spontaneous breathing only buys extra time or serves to identify the subgroup with the worst possible prognosis in those patients who do not improve in the prone position.
FundingNone whatsoever.
Conflicts of interestNone reported.
The authors wish to thank all the healthcare personnel, many of them not involved in the intensive care setting, who still gave us their best so these data could become available.
Francisco-Javier Ramos (Hospital Universitari Vall d'Hebron, Barcelona), Adrián Rodríguez (Hospital Clínico de Zaragoza), Candelaria de Haro (Ciutat Sanitaria Parc Taulí, Sabadell), Gemma Rialp (Hospital Universitari Son Llatzer, Mallorca), José Manuel Gutiérrez (Hospital General de Albacete), Alberto Belenguer (Hospital Universitari Dr. Peset, Valencia), Jorge Rodríguez (Hospital Universitario La Paz-Carlos III, Madrid), Claudia Domínguez-Curell (Hospital Universitario de Canarias, Tenerife), Mónica Magret (Hospital Joan XXIII, Tarragona), Manuel Gracia (Hospital de Jerez de la Frontera, Cádiz), Laura Bellver (Hospital de la Ribera, Valencia), Ferran Roche-Campo (Hospital Verge de la Cinta de Tortosa), Teresa Millan (Hospital Son Espases, Mallorca), Andrea Ortiz (Hospital Comarcal de Vinaroz, Castellón), Aaron Blandino (Hospital Ramón y Cajal, Madrid), Caridad Martin (Hospital General de Segovia), Anxela Vidal (Fundación Jiménez Díaz, Madrid), and Noelia Albala (Hospital Universitario de Salamanca).
Please cite this article as: Fernández R, González de Molina FJ, Batlle M, Fernández MM, Hernandez S, Villagra A, et al. Soporte ventilatorio no invasivo en pacientes con neumonía por COVID-19: un registro multicéntrico español. Med Intensiva. 2021;45:315–317.