During resuscitation, basic life support (BLS) and automated external defibrillation refer to maneuvers designed to maintain airway patency and support breathing and circulation without equipment other than a barrier device and the use of an automated external defibrillator (AED). We present some of the most important developments incorporated into the new international recommendations for resuscitation 2010. Aspects related to prevention and early detection of cardiac arrest are highlighted, along with the important role of dispatchers of emergency medical services, the importance of high quality CPR and programs of public access defibrillation. We likewise describe sequences of action and basic life support algorithms, and semi-automated external defibrillation.
Durante la resucitación, el soporte vital básico (SVB) y la desfibrilación externa automática hacen referencia a las maniobras de mantenimiento de la permeabilidad de la vía aérea, el apoyo de la respiración y de la circulación, sin el uso de otro equipo que un dispositivo de barrera, y el uso de un desfibrilador externo automático (DEA). Se presentan a continuación algunas de las novedades más importantes que incorporan las nuevas recomendaciones internacionales en resucitación de 2010. Se destacan los aspectos relacionados con la prevención y detección precoz de la parada cardiaca, el papel importante de los teleoperadores de los servicios de emergencias médicas, la importancia de la resucitación cardiopulmonar de alta calidad y de los programas de acceso público a la desfibrilación. Se presentan las secuencias de actuación y algoritmos de soporte vital básico y desfibrilación externa semiautomática.
Cardiac sudden death (CSD) affects about 350,000–700,000 individuals each year in Europe, and 25–30% of the victims present ventricular fibrillation (VF) as initial manifesting rhythm. Probably many more patients have rhythms amenable to defibrillation (DF) at the time of cardiac arrest, but in many cases when the Medical Emergency Service (MES) teams monitor the electrocardiogram (ECG), the rhythm has deteriorated to asystolia. If the rhythm is registered immediately affect arrest, the proportion of victims with VF would be 59–65%. The treatment for cardiac arrest due to VF is immediate cardiopulmonary resuscitation (CPR) by witnesses (chest compressions combined with rescue breathing) and early defibrillation.
Most cases of cardiac arrest of non-cardiac origin are due to respiratory causes such as drowning, particularly in children, and asphyxia. According to the World Health Organization (WHO), in many parts of the world drowning is the main cause of death (http://www.who.int/water_sanitation_health/diseases/drowning/in/); as a result, rescue breathing is perhaps more determinant for resuscitation of the victims.
In most communities, the time taken by the MES team in reaching the site of arrest is 8min, versus 11min for the first defibrillator discharge. Patient survival therefore depends on the start of BLS by the witnesses of the event and the use of an automated external defibrillator (AED) for defibrillation, where available.
The results of the latest international consensus conference of the International Liaison Committee on Resuscitation (ILCOR) held in Dallas in February 2010, and its conclusions, published in October, conform the Guides 2010 on resuscitation. The present study describes the principal aspects of BLS and AED, as well as the novelties from the mentioned conference, published by the European Resuscitation Council (ERC).
The chain of survivalThe actions linking the cardiac arrest victim to survival is known as the chain of survival, which summarizes the vital steps required for successful resuscitation. These steps or actions include early recognition of the emergency situation and activation of the MES, early CPR, early defibrillation and advanced life support (ALS), together with care after resuscitation if the victim recovers from cardiac arrest.
The importance of recognizing the critical situation and/or heart attack, and of avoiding cardiac arrest, as well as of the care following resuscitation, is underscored by the inclusion of these elements in the four-link chain of survival. The first link indicates the importance of recognizing individuals at risk of cardiac arrest, and of calling for help in the hope that rapid patient care can avoid the arrest. The central links of this chain in turn define the integration of CPR and defibrillation as the key components in early resuscitation, in an attempt to restore life. The end link, advanced life support and effective treatment posterior to resuscitation, focuses on the preservation of the vital signs of the patient – particularly referred to the heart and brain.
Description of the links in the chain of survival (Fig. 1):
- 1.
As has been commented, the first link in the chain is alerting the MES after recognizing the situation of cardiac arrest. The number dialed is the same throughout Europe: 112. The alerting person must identify himself, clearly explain what is happening to the patient, identify the precise location, and indicate whether CPR maneuvers will be started. The indications of the dispatcher are to be followed, and the latter must always be the last to hang up.
- 2.
The second link is basic CPR by the persons witnessing the arrest. High-quality CPR can double or even triplicate survival.
- 3.
The third link in the chain is defibrillation, which should take place as soon as possible. In effect, defibrillation is a key element in the chain of survival, and is one of the few interventions to have been shown to improve the outcome of cardiac arrest with VF. Since the effectiveness of the discharges quickly decreases with passing time, defibrillation ideally should be carried out before the arrival of the MES – the average response time of the latter being no less than 8–10 min. In this context, AED are safe and effective when used by laypersons. Thus, ideally the first intervening person (witness, trained volunteer, fireman, policeman, etc.) should be able to use an AED, and the latter should be available in the first 3–5min of arrest. The new recommendations advocate the installation of AEDs in particularly busy public places, and stress the importance of public access to defibrillation programs.
- 4.
The fourth and final link in the chain is represented by ALS and patient care after resuscitation.
Acute coronary syndrome (ACS) is the most common cause of cardiac sudden death. Recognition of the cardiac origin of chest pain is very important, since the probability of cardiac arrest secondary to acute myocardial ischemia is at least 21–33% in the first hour after symptoms onset.1,2 The telephone call dialing 112 to activate the MES must be made as soon as the first symptoms are identified.3
Recognizing cardiorespiratory arrestIn many cases, even for healthcare professionals, it proves difficult to determine whether an unconscious person is in a state of cardiac arrest. Healthcare professionals, in the same way as laypersons performing resuscitation, have difficulties determining the presence or absence of normal breathing in unresponsive victims, since either the airway is not open, or the patient is gasping. In this context, gasping is present in up to 40% of all cases of cardiac arrest and in the first minutes, and survival is favored when gasping is recognized as a sign of cardiac arrest. Laypersons therefore should be instructed to start CPR if the victim is unconscious and fails to respond or does not breathe normally. Adequate description of the condition of the patient is extremely important when calling the MES. It is very important for the telephone operator or dispatcher to receive information on the breathing of the patient from the person who is calling. Precision in the identification of cardiac arrest on the part of the telephone operators varies considerably. If the operator adequately recognizes the situation, appropriate measures can be taken, such as CPR by witnesses under telephone guidance, and the advanced life support units can ensure an adequate response.
Training of the dispatchers of out-hospital emergency servicesThe telephone operators or dispatchers receiving the emergency calls must be trained through strict protocols in obtaining relevant information from the calling person. This information is based on the recognition of the absence of response and on evaluation of the quality of breathing of the victim. In the presence of a patient who fails to respond and does not breathe normally, a suspected cardiorespiratory arrest (CRA) protocol should be activated immediately. Gasping and short and noisy breathing on the part of the victim are not to be confused with normal breathing. Gasping is present in 40% of the cases in the first minutes of CRA, and patient survival is improved when it is recognized as a sign of arrest.4 Likewise, the dispatchers must be trained to guide the calling person by telephone to perform CPR with chest compressions only. Performing CPR only with compressions is better than performing no CPR maneuvers.5,6 When the calling person has no training in CPR, the telephone operator should insist on the application of chest compressions until the MES arrives. In the first minutes of CRA of cardiac origin, the blood does not suffer important oxygen desaturation, and compressions are a priority concern to ensure a minimum blood flow to the brain and myocardium, with a view to maintaining sensitivity to defibrillation – increasing the chances for restored cardiac rhythm with an effective beat after defibrillation. For every minute of delay in applying defibrillation, survival following VF decreases 10–12%.7,8 It the person witnessing CRA performs CPR, the decrease is only 3–4%/min.8–10 Immediate CPR performed by witnesses on scene can double or even triple survival in cardiac arrest with VF.13
High-quality CPRThe new recommendations underscore the importance of quality cardiac massage as a determinant factor for survival at hospital discharge among patients who have suffered cardiac arrest.
Cardiac massageCardiac massage should be performed as follows: the resuscitating person is to position himself alongside the victim and place the base of the palm of the hand on the center of the chest of the patient. The base of the other hand is then placed parallel over that of the first, intercrossing the fingers of both hands, and compressing the chest of the patient with both arms extended and vertical – depressing the sternum at least 5cm but no more than 6cm. The pressure is then relaxed completely to allow the chest of the patient to expand, but without removing the hands from the chest. The compression maneuvers are to be performed at a rate of between 100 and 120/min. The compressions and decompressions should have the same duration. If the resuscitating person is able to do so, two rescue breathings should be interspaced with a sequence of 30 compressions/two ventilations.
As a result of a lack of strength, out of fear of causing injury, and particularly due to fatigue, some resuscitators compress the chest less deeply than indicated. There is documented evidence that a minimum compression of 5cm results in a greater rate of spontaneous circulatory recovery (SCR) than compression with a depth of 4cm or less. Damage produced by cardiac massage has not been shown to be directly related to the depth of chest compression, and there are no studies indicating a limit to the depth of compression; in any case, however, a depth of 6cm should not be exceeded.
Rescue breathingIn order to be effective, rescue breathing should be carried out as follows: the resuscitating person should open the patient airway by means of the forehead-chin maneuver, clamping the nose with the thumb and index finger of the hand placed on the forehead and, after a normal inspiration, should insufflate air into the mouth of the patient, using the lips to seal the mouth, while confirming the rising chest of the victim. The resuscitator then should draw back from the patient, breathe in again, and repeat the maneuver once the air has passively emerged from the chest of the patient. Two respirations should be made in 5s. Immediately afterwards, another sequence of 30 compressions should be started.
CPR only with compressionsWitnesses of a cardiac arrest who have had no training in CPR can perform cardiac massage alone, following the real-time indications of a trained dispatcher. In this case uninterrupted chest compressions are indicated at a rate of at least 100/min, but no more than 120/min.11,12
Lastly, feedback for the resuscitating person is important to guarantee quality CPR. During resuscitation, devices can be used allowing immediate warning/feedback. The data recorded by the resuscitation equipment can also be used for resuscitation quality control.
Elimination of a predetermined period of CRP before defibrillation in out-hospital arrest not witnessed by the MESDifferent studies have demonstrated the beneficial impact of immediate CPR upon patient survival, and the negative consequences of a delay in defibrillation.7,11,13 Other studies have analyzed the convenience of applying a period of CPR before starting defibrillation in non-evidenced cardiac arrest, or in those cases where some time has elapsed until the start of CPR. Review of the evidence for the 2005 guides resulted in the recommendation for the MES to perform 2min (5 cycles of 30:2) of CPR before defibrillation in cases of prolonged arrest (over 5min). The studies presented were carried out in arrests in which the time to response exceeded 4–5min, and in which the paramedics or physicians of the MES performed 1.5–3min of CPR before defibrillation. This protocol improved SCR as well as survival at hospital discharge14,15 and after 1 year in patients with out-hospital VF, compared with the cases in which immediate defibrillation was carried out. In two randomized, controlled trials, a period of 1.5–3min of CPR before defibrillation, performed by the MES personnel, did not improve either SCR or survival at discharge in VF, independently of the response time of the MES.16,17 Other studies likewise have failed to demonstrate improvements in SCR or survival at discharge with initial CPR,18,19 although one reported a more favorable neurological prognosis 30 days and 1 year after arrest.22
There is scientific evidence that cardiac massage while placing the electrodes and loading the AED improves patient survival. Therefore, the MES team should perform CPR while the AED is being prepared, the electrodes are placed on the patient, and the device is being charged, with a view to minimizing the interruption of chest compressions. However, the new recommendations do not specify a concrete duration of CRP (2–3min) before analyzing cardiac rhythm and administering a discharge, where indicated. If some MES, following the 2005 indications, apply a certain duration of chest compressions before defibrillation, they may continue with this practice, in view of the lack of conclusive data indicating the need for changes in this sense.
Maintenance of cardiac massage while loading the AEDWarranted by the scientific evidence, the new recommendations underscore the importance of high-quality cardiac massage, with the minimization of interruptions, for improving patient survival. Following these indications, chest compression is to be continued while the AED is placed and used. These defibrillators are safe and easy to use by laypersons, and allow defibrillation of the patient before arrival of the MES. Defibrillation technology advances quickly and now allows the evaluation of cardiac rhythm while CPR is performed, and the resuscitating person can continue the chest compressions while the AED analyzes the rhythm and indicates the convenience or not of delivering a discharge. In this way it is possible to minimize the time between interruption of the chest compressions and administration of the discharge (pre-discharge pause). A delay of only 5–10s suffices to lessen the efficacy of defibrillation.20–22 The pre-discharge pause can be reduced to less than 5s if massaging is continued during loading of the AED, and if the team is guided by an effective person. Rigorous but rapid checking is required to ensure that nobody is in physical contact with the patient at the moment of the discharge. The risk of someone on the resuscitating team receiving a discharge can be lessened if all members wear gloves during the intervention. After defibrillation, chest compression should be resumed immediately in order to reduce the post-discharge pause. The entire process should be carried out without interrupting cardiac massage for more than 5s.
Defibrillation is a key link in the chain of survival, and one of the few interventions truly capable of improving survival in cardiac arrest due to VF. The success of discharges decreases rapidly with passing time. It is very difficult for defibrillation to be carried out by the MES in the first few minutes of arrest. The intervention of trained volunteers has improved the outcome at hospital discharge, and if defibrillation is carried out in the first 3min of arrest, the survival rate can reach 75%.
People trained in the use of the AED must be able to perform quality CPR until the MES arrives on scene. The guides stress the importance of performing immediate CPR with high-quality compressions on an early and uninterrupted basis. Compression should only be interrupted for as briefly as possible to perform ventilation, analyze the cardiac rhythm or deliver a discharge, and should be resumed immediately after defibrillation. If two resuscitators are available, one should prepare the AED, position the electrodes on the naked chest of the patient and connect the defibrillator, while the other should perform the chest compressions – interrupting them only to analyze the rhythm, check that nobody is in contact with the patient, and apply the discharge.
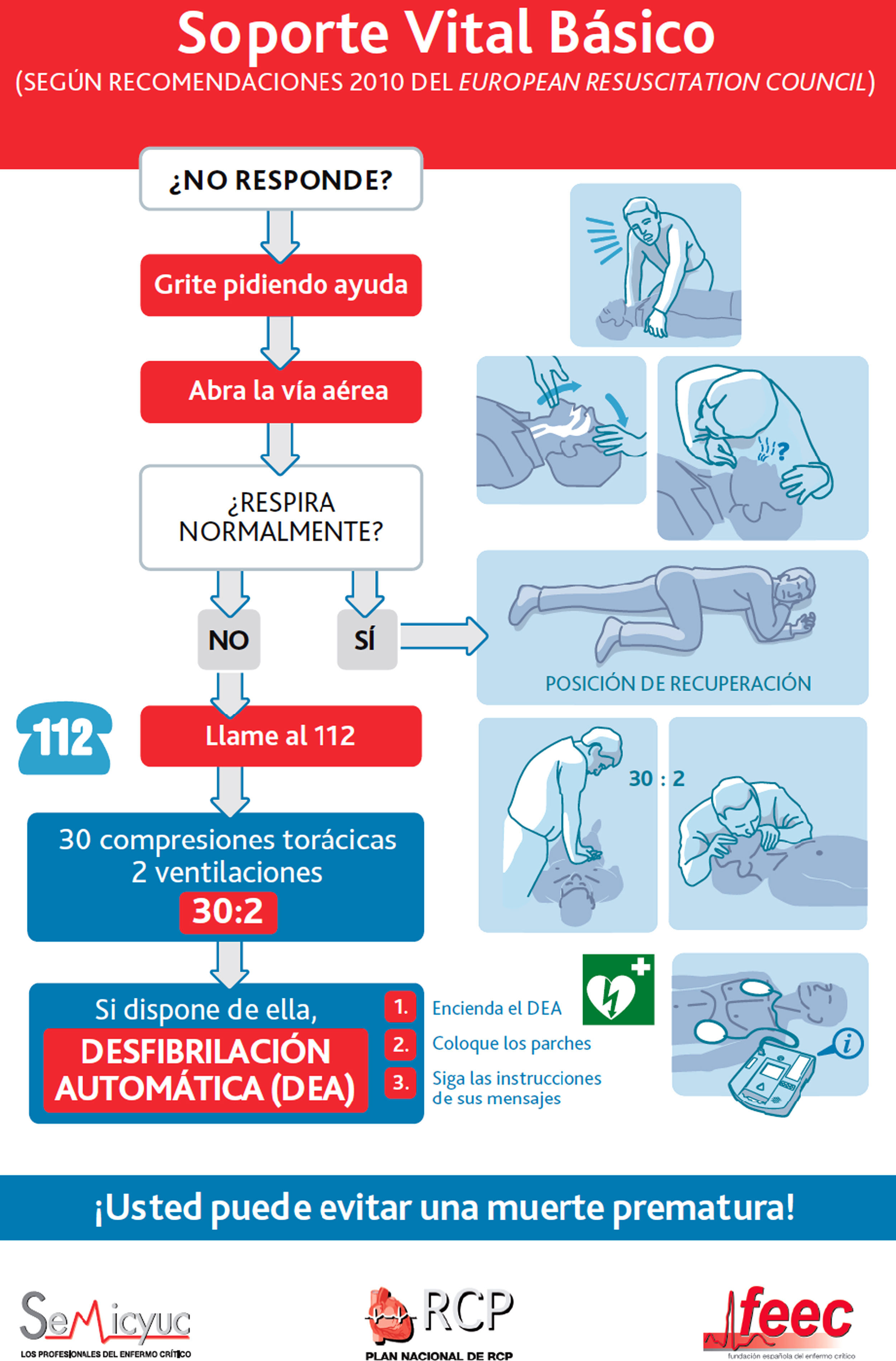
Sequence of BLSThe sequence of maneuvers is described in Fig. 2.
Use of an AEDAED are safe and effective, even when used by laypersons, and make it possible to apply defibrillation long before the arrival of professional help. The resuscitators should continue CPR with minimum interruption of the chest compressions while the AED is being placed and during its use. The resuscitators should follow the verbal instructions immediately, and particularly must ensure the resumption of CPR. The standard AED can be used with children over 8 years of age. In the case of children between 1 and 8 years of age, pediatric patches/electrodes should be used, together with an attenuator or pediatric operating mode, if available. If not available, the AED should be used as is. The use of these devices is not recommended in infants under 1 year of age.
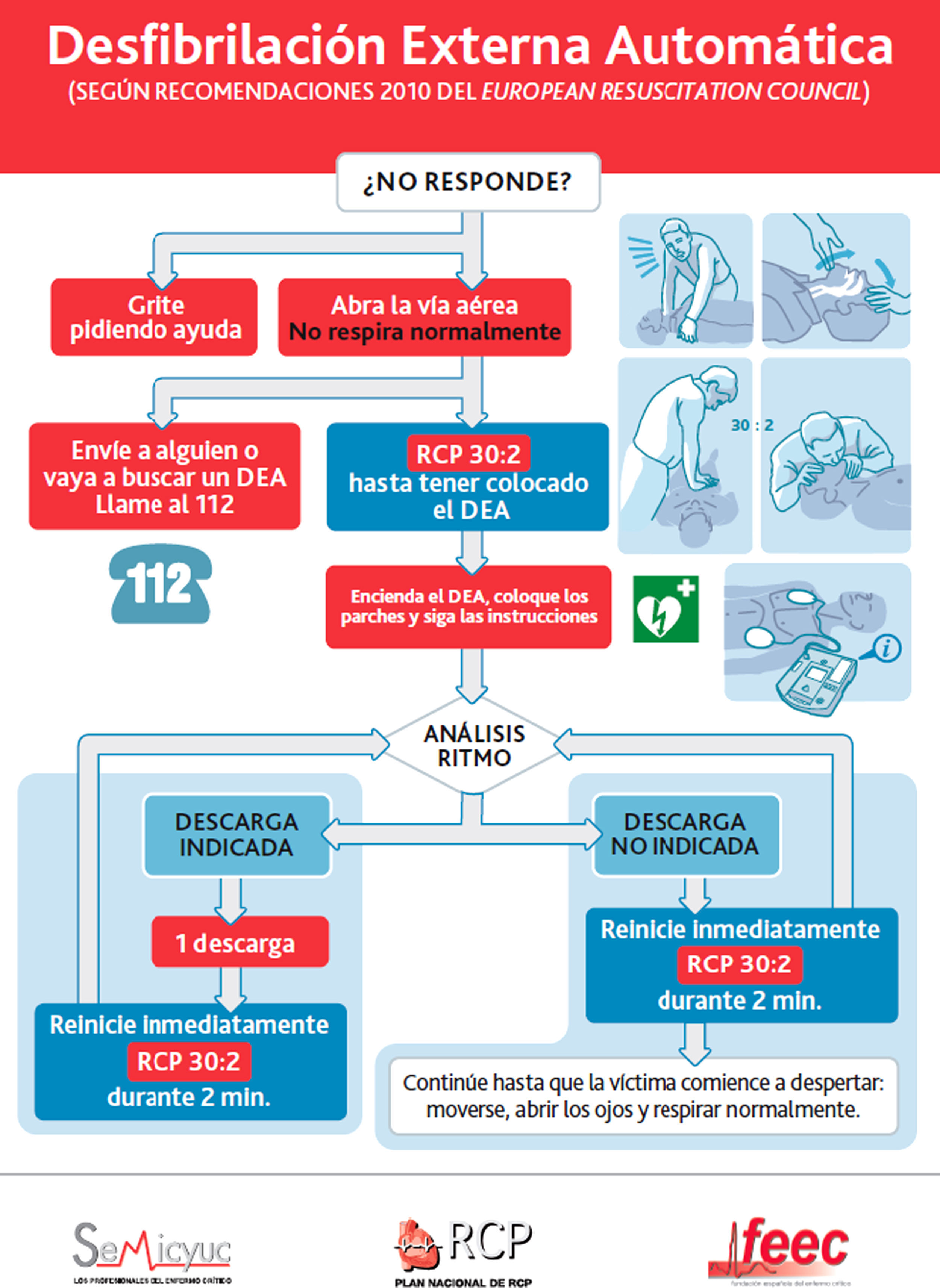
Sequence of BLS and use of the AEDThe sequence of interventions is shown in Fig. 3.
Public access to defibrillation (PAD) programsPublic access to defibrillation programs should be targeted to public places such as airports, train or subway stations, sports centers, industrial centers, commercial centers, stadiums, offices, casinos and airplanes, i.e., places where cardiac arrest can be witnesses and where trained resuscitators can quickly appear on scene. PAD programs involving laypersons as resuscitators and with short response times, using police personnel as first intervening persons, have resulted in survival rates of between 49 and 74%. Accordingly, PAD programs can only offer success if trained resuscitators and AEDs in sufficient number are available.20,21
However, the great potential benefit of AEDs has not yet been materialized, since these devices are generally located in public places, and almost 80% of all cardiac arrests occur in the home or in residential areas. PAD programs and the use of AEDs by first intervening resuscitators can serve to increase the number of victims that receive CPR by witnesses, and early defibrillation. When developing such a program, the community supervisors must assess factors such as adequate emplacement of the AED, based on previous incidence or population concentration studies; the training of a team in charge of monitoring and maintaining the devices; the training of people who probably will use the AEDs; and, if possible, identify those individual volunteers agreeing to use the device on the victims of cardiac arrest.
The installation of AEDs in residential areas has not been studied to date, and the acquisition of an AED for individual use in the home – even among individuals considered to be at high risk of cardiac arrest – has not been evaluated.
In order for AED installation and the PAD program to offer maximum effectiveness, the American Heart Association (AHA) has underscored the need to incorporate a series of elements23:
- 1.
Organization and planning of the response in the event of an emergency situation.
- 2.
Training of the possible resuscitators both in handling of the AED and in applying CPR.
- 3.
Connections to the local MES.
- 4.
Establishment of a continued quality improvement process, analyzing from adequate operation of the AEDs and the required electrodes to adequacy of the response system and competence of the resuscitators.
It has been shown that places in which an AED has been located without all these elements are unlikely to improve survival among cardiac arrest patients, since the mere presence of these devices does not mean that they will be used in the event of need, or that they will be used correctly.23
ILCOR universal AED signThe ILCOR has unanimously approved the suggestion by its work group to adopt a universal sign indicating the presence of an AED. The sign has been designed according to the ISO 7010 norm for safety signs and models. The colors and symbols in turn comply with the ISO 3864-3 norm, and its interpretability has been confirmed according to the ISO 9186-1, rev. 2007 norm, proving to be superior to other designs. The AED sign (Fig. 4) aims to indicate the presence of the device, its location in any room or container, for both public use and to indicate the direction in which to go in order to reach it. The sign should serve to quickly identify an AED in a public place for immediate use on a cardiac arrest victim. To this effect, the AED can be combined with other symbols such as an arrow. The sign can also be accompanied by the letters “AED”, or the equivalent in other languages. The full term “defibrillator” (or equivalent) is not recommended.
It is the aim of the ILCOR to have this sign approved throughout the world by the respective national resuscitation councils. The sign also must be approved by all AED manufacturers for use with their products, and by the signaling industry. The different public organizations and governments in turn should promote the universal adoption of this AED sign.
In this sense, it is to be expected that this universal sign will enhance awareness of the existence of these devices and will contribute to their rapid incorporation in emergency situations in the form of cardiac arrest (https://www.erc.edu/index.php/newsItem/in/nid=204/).
Summary of changes since the guides of 2005Lastly, it should be mentioned that many of the recommendations of the European Resuscitation Council (ERC) Guides 2005 remain without change – either because no new studies have been published, or because the new evidence available since 2005 has simply reinforced the already existing evidence. Nevertheless, the evidence published since 2005 does point to the need to incorporate changes to some parts of the new Guide 2010. In summarized form, the changes of 2010, in relation to the Guides 2005, referred to BLS and AED are the following20:
- •
Emergency telephone operators must be trained to question people who call, using strict protocols for obtaining information. This information should center on recognizing a lack of patient response and on the quality of breathing. In combination with the absence of response, the absence of breathing or any other breathing anomaly should serve to activate the telephone operator protocol for suspected cardiac arrest. The importance of gasping as a sign of cardiac arrest is underscored.
- •
All resuscitators, whether trained or otherwise, should perform chest compressions on victims of cardiac arrest. It remains essential to stress the importance of high-quality chest compression. The aim should be to compress to a depth of at least 5cm, with a frequency of at least 100compressions/min, allowing full chest rebound, and minimizing interruptions of chest compression. Trained resuscitators also should perform ventilations with a compression/ventilation ratio of 30:2. In the case of non-trained resuscitators, CPR only with chest compressions guided by telephone is advocated.
- •
Devices allowing interactive messages during CPR will offer resuscitators immediate feedback, and their use is thus encouraged. The data stored by the resuscitation equipment can be used to supervise and improve the quality of CPR, and supply information to the professional resuscitators during the revision sessions.
- •
These guides underscore the importance of performing early chest compressions without interruptions.
- •
Much greater emphasis is now placed on the need to minimize the duration of the pauses before and after AED discharge; continuation of chest compression during loading of the device is recommended, with immediate resumption of compression after defibrillation. The defibrillator discharge should be completed with no more than a 5-s interruption of the chest compressions.
- •
The safety of the resuscitator remains essential, although these guides recognize that the risk of damage with a defibrillator is very small – particularly when gloves are worn. Attention now focuses on rapid safety checking, in order to minimize the pre-discharge pause.
- •
In the case of cardiac arrest outside the hospital, the MES personnel should provide quality CPR. With the availability of a defibrillator, the device should be placed and loaded, although it is no longer recommended to systematically perform prior CPR, e.g., for a period of 2 or 3min, before the analysis of cardiac rhythm and discharge. If some MES have fully incorporated certain duration of chest compressions before defibrillation to their intervention protocol, they may reasonably continue with this practice, in view of the lack of conclusive data indicating the need for changes in this sense.
- •
Increased development of the PAD programs is encouraged, underscoring the need for an increased distribution of AEDs in both public and residential areas.
Please cite this article as: López-Messa JB, et al. Novedades en soporte vital básico y desfibrilación externa semiautomática. Med Intensiva. 2011;35:299–306.