Cardiovascular failure or shock, of any etiology, is characterized by ineffective perfusion of body tissues, inducing derangements in the balance between oxygen delivery and consumption. Impairment in oxygen availability on the cellular level causes a shift to anaerobic metabolism, with an increase in lactate and hydrogen ion production that leads to lactic acidosis. The degree of hyperlactatemia and metabolic acidosis will be directly correlated to the development of organ failure and poor outcome of the individuals.
The amount of oxygen available at the tissues will depend fundamentally on an adequate level of perfusion pressure and oxygen delivery. The optimization of these two physiologic parameters can re-establish the balance between oxygen delivery and consumption on the cellular level, thus, restoring the metabolism to its aerobic paths. Monitoring variables such as lactate and oxygen venous saturations (either central or mixed) during the initial resuscitation of shock will be helpful to determine whether tissue hypoxia is still present or not. Recently, some new technologies have been developed in order to evaluate local perfusion and microcirculation, such as gastric tonometry, near-infrared spectroscopy and videomicroscopy. Although monitoring these regional parameters has demonstrated its prognostic value, there is a lack of evidence regarding to its usefulness during the resuscitation process.
In conclusion, hemodynamic resuscitation is still based on the rapid achievement of adequate levels of perfusion pressure, and then on the modification of oxygen delivery variables, in order to restore physiologic values of ScvO2/SvO2 and resolve lactic acidosis and/or hyperlactatemia.
La insuficiencia cardiovascular o shock, de cualquier etiología, se caracteriza por la inadecuada perfusión de los tejidos del organismo, produciendo una situación de desequilibrio entre el aporte y la demanda de oxígeno. La disminución de la disponibilidad de oxígeno en el área celular se traduce en un aumento del metabolismo anaerobio, con producción de lactato e hidrogeniones, derivando en la acidosis láctica. El grado de hiperlactatemia y acidosis metabólica va a correlacionarse directamente con el desarrollo de fracaso orgánico y mal pronóstico del individuo.
La llegada de oxígeno a los tejidos depende fundamentalmente de una presión de perfusión del tejido suficiente y de un transporte de oxígeno adecuado. La adecuación de estos dos parámetros fisiológicos va a posibilitar la restauración del equilibrio entre aporte y demanda celular de oxígeno, revirtiendo el proceso de anaerobiosis. La monitorización de variables como el lactato y las saturaciones venosas de oxígeno (central o mixta) durante la fase aguda del shock serán útiles en la determinación de persistencia o resolución de la hipoxia tisular. En los últimos años, han aparecido nuevas tecnologías capaces de evaluar la perfusión local y la microcirculación, como la tonometría gástrica, la espectroscopia en el límite de la luz infrarroja y la videomicroscopia. Aunque la monitorización de parámetros de carácter regional ha demostrado su valor pronóstico, no se dispone de evidencia suficiente que le otorgue utilidad en la guía del proceso de reanimación.
En conclusión, a la espera de disponer de parámetros capaces de proporcionarnos información útil de perfusión local, la reanimación hemodinámica sigue basada en la consecución rápida de valores de presión de perfusión del tejido adecuados, y seguir el proceso de reanimación mediante la modificación de variables de transporte de oxígeno, con la intención de conseguir la restauración de valores fisiológicos de SvO2/SvcO2, así como a la resolución de la acidosis láctica y/o hiperlactatemia.
In routine clinical practice in critical care medicine, one of the main concerns is to ensure the well being of the tissues while specifically treating the background disease causing the primary damage. “Tissue well being” refers to the provision of nutrients and oxygen for the cells, allowing them to continue their basic functions, as referred to both intrinsic cellular function and body tissue/organ organization. When cellular oxygen use is altered, the biological processes are affected – giving rise to impaired organ function. If the harmful stimulus or altered oxygen status persists, the metabolic disorders that develop within the cells can lead to cell death – with the consequent establishment of organic damage, multiorgan failure and even the death of the individual.
In critically ill patients, the incapacity to maintain adequate organ perfusion results in cellular dysoxia, which is characterized by an increase in anaerobic metabolism in order to maintain ATP production. This shift from aerobic to anaerobic metabolism gives rise to an accumulation of lactic acid (lactate), hydrogen ions and inorganic phosphates within the cell. Upon gaining access to the bloodstream, such lactate and hydrogen ion production gives rise to lactic acidosis. The degree of hyperlactatemia and metabolic acidosis is directly correlated to the development of organ failure and a poor patient prognosis.1 Another important metabolic manifestation resulting from this imbalance between oxygen transport and consumption is an increase in the degree of extraction of oxygen contained in arterial blood – a parameter that can be quantified by measuring central venous oxygen saturation in either the right atrium (SvcO2) or the pulmonary artery (SvO2). On occasion of the consensus meeting of the different medical societies dedicated to the care of critically ill patients,2 “shock” (or circulatory failure) was taken to represent the evidence of tissue hypoperfusion, defined as an elevation of lactate concentration and/or a reduction of SvcO2 or SvO2. Thus, the clinical definition of shock now extends beyond the classical interpretation of the presence of arterial hypotension, and centers on the presence of tissue dysoxia.
The arrival of oxygen within the tissues is fundamentally dependent upon two factors: (a) the existence of sufficient perfusion pressure; and (b) adequate oxygen transport. Adequate adjustment of these two physiological parameters will allow restoration of the balance between cellular oxygen demand and supply – reverting the process of anaerobiosis. Thus, in accordance with the hemodynamic resuscitation guidelines, normalization of the hypoperfusion metabolic parameters is conditioned to modification of the basic cardiovascular parameters, such as tissue perfusion pressure and blood flow – these being the main determinants, together with hemoglobin, of oxygen transport. The capacity of the cardiovascular system to meet the body oxygen requirements and avoid cellular hypoxia in turn is directly related to patient survival.3
The present article describes the means available for detecting tissue hypoperfusion and its applications to hemodynamic resuscitation.
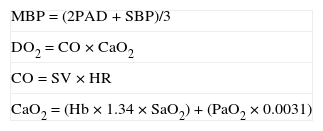
Hemodynamic and macrocirculatory parametersArterial pressureAs has been commented, adequate tissue oxygen supply is not only dependent upon blood flow but also requires a correct tissue perfusion pressure. At mean blood pressure (MBP) values below 60–65mmHg, the vascularization of most tissue beds loses its auto-regulatory capacity, resulting in a drop in intravascular pressure and ineffective maintenance of capillary blood flow. In physiological terms, in order to secure effective microcirculatory flow, there must be a pressure gradient between the two extremities of the circuit. It is therefore important to remember that not only the “global” blood flow is responsible for tissue oxygen supply, and that a minimum pressure gradient is needed in order for real flow to occur at microcirculatory level. Thus, a minimum perfusion pressure is required. In order to quantify this perfusion pressure, use is made of the mean blood pressure (MBP), which reflects the circulatory pressure of the arterial system4 (Table 1).
Formulas.
| MBP=(2PAD+SBP)/3 |
| DO2=CO×CaO2 |
| CO=SV×HR |
| CaO2=(Hb×1.34×SaO2)+(PaO2×0.0031) |
CaO2: arterial oxygen content; DO2: global oxygen transport; HR: heart rate; CO: cardiac output; Hb: hemoglobin; DBP: diastolic blood pressure; MBP: mean blood pressure; PaO2: partial arterial oxygen pressure; SBP: systolic blood pressure; SaO2: arterial oxygen saturation; SV: systolic volume.
From the physiological perspective, it seems reasonable to maintain MBP values above 60–65mmHg, since this would be the point below which most vascular beds lose their local auto-regulatory capacity. However, it must be remembered that other factors can influence the vascularization in each individual patient, such as chronic arterial hypertension, with the consequent adaptive changes in the auto-regulation of tissue blood flow. Unfortunately, few studies have explored different values of MBP with reference to the resuscitation guidelines, and there is even less information regarding associated factors such as chronic hypertension. An observational study of 111 septic shock patients used different values of MBP to define hypotension (60, 65, 70 and 75mmHg); of these values, a MBP of 65mmHg was seen to be the value that best discriminated between survivors and non-survivors both 6 and 48h after admission.5 However, few studies in the literature have explored the effect of reaching different values of MBP in the resuscitation process. In a small study involving 10 patients with septic shock, increasing MBP from 65 to 75 and to 85mmHg did not reveal benefits in terms of improved tissue perfusion, as evaluated from the lactate values, diuresis and gastric tonometry.6 Therefore, the consensus conference on hemodynamic resuscitation held in Paris in 20062 recommended maintaining a MBP of 65mmHg in patients with shock of any origin, except in two special situations: (a) uncontrollable bleeding in trauma patients, where the recommendation was to maintain MBP at 40mmHg until the bleeding is controlled surgically (or with vascular intervention techniques); and (b) in serious head injury patients without systemic bleeding, where the recommendation was to maintain MBP above 90mmHg until correct brain perfusion pressure can be achieved and monitored.
It is nevertheless important to remember that although certain MBP values ensure correct tissue perfusion pressure, this variable has been shown to be scantly sensitive in detecting tissue hypoperfusion; accordingly, a normal MBP value does not rule out the presence of hypoperfusion.7
Global oxygen transportSince we are referring to the adequacy of oxygen supply to the cells, in order to allow the latter to perform their normal activities, the monitorization of global oxygen transport (DO2), as a measure of oxygen flow towards the tissues, has been one of the most extensively studied parameters in critical care situations. The tissues can maintain their metabolic activity, in terms of oxygen consumption (VO2), despite significant reductions in DO2 thanks to adaptive mechanisms that result in increased extraction of the O2 transported in blood (VO2 independent of DO2). However, beyond certain values of DO2, and despite the increase in O2 extraction, a drop in tissue metabolic activity is effectively observed. Thus, VO2 becomes dependent upon DO2. This DO2 value is referred to as the critical DO2, and has been estimated in different studies as approximately 4–8mlO2/kg/min.8
DO2 is provided by cardiac output (CO) and arterial oxygen content (CaO2) (Table 1) – the latter depending mainly on hemoglobin (Hb) and arterial oxygen saturation (SaO2). Of these three factors, the one most subject to short-term changes as a compensatory mechanism is CO. Thus, the immense majority of interventions aimed at increasing DO2 are based on an increase in CO.
In a series of observational studies published back in the 1980s and 1990s, the group led by Shoemaker recorded increased survival among the patients presenting higher DO2 values, both in situations of high surgical stress and in situations of cardiovascular failure related to sepsis.9,10 On the basis of these findings, different groups carried out studies in which resuscitation was guided according to a pre-established DO2 value – normally 600mlO2/min/m2 – with variable results. From the detailed analysis of these studies we can draw the conclusion that hemodynamic resuscitation guided by DO2 values does offer benefit in terms of prognosis when applied to the adequate patient groups (high risk surgical patients) and at the adequate time (with no benefit in late resuscitation).11 Despite the success shown by resuscitation according to DO2 values in this selected population, questions remain regarding the usefulness of this parameter in other critical patient populations. In fact, and from a physiopathological perspective, a series of doubts may be raised as to its clinical usefulness.
The amount of oxygen reaching the cells depends on a number of both central and peripheral factors. The central factors could be summarized as those encompassed within the concept of DO2 (CO, Hb and SaO2). The peripheral factors in turn would comprise the redistribution of CO to the different organs and local regulation of the microcirculation, determined mainly by the autonomous control of vascular tone and the local humoral responses of the microcirculation. Unfortunately, since DO2 only offers information on this central component of oxygenation, it is scantly sensitive in clinical practice–because it can fail to detect anomalies in regional perfusion. Thus, although the concept of DO2 and VO2 is important, its sole application in guiding a resuscitation protocol is probably to simplistic,12 particularly in septic patients, where we find a greater degree of dysfunction and heterogeneity of the microcirculation.
Venous oxygen saturations (central and mixed)Mixed venous oxygenation (SvO2) is probably the best isolated indicator of the adequacy of global oxygen transport (DO2), since it represents the amount of oxygen remaining in the systemic circulation after its passage through the tissues.13 Mixed venous oxygenation could be said to inform us about the “oxygen reserve” or balance between oxygen transport (DO2) and consumption (VO2). Its use in clinical practice was facilitated over a decade ago by the availability of fiber optic pulmonary artery catheters allowing the continuous monitorization of SvO2.14 More recently, the improvements in survival among septic patients treated on an early basis according to treatment objectives centered on the measurement of venous oxygen saturation has generated renewed interest in such monitorization.15
Increases in VO2 or decreases in Hb, CO or SaO2 result in a drop in SvO2. A reduction of CO or excessive VO2 initially may be compensated by an increase in the arteriovenous oxygen difference – this normally resulting in decreased SvO2. This is an early compensatory mechanism and can precede the rise of lactate in blood.16 It is important to note that the relationship between the changes in CO and SvO2 is not linear; accordingly, a given decrease in the latter parameter may correspond to a comparatively greater decrease in cardiac output.
From the practical perspective, values of SvO2<60–65% under acute patient conditions should alert us to the presence of tissue hypoxia or inadequate perfusion. However-and this is another important concept in relation to SvO2-although a low value should alert us to the presence of inadequate tissue perfusion, as has been explained, a normal value does not guarantee adequate oxygenation in all organs if vascular regulation is altered. Thus, given its “global character”, SvO2 is not without some of the limitations found with the measurement of DO2, since it is unable to assess local perfusion deficits. Consequently, in situations where the microcirculation is greatly altered, with shunt and heterogeneous flow phenomena, SvO2 may present increased values coexisting with situations of intense tissue hypoxia.
The obtainment of mixed venous blood from the pulmonary artery or right ventricle requires right-side catheterization. The possibility of determining the oxygen saturation of central venous blood, which is more easily accessible, has been the subject of debate for a long time. In effect, the problem is that oxygen saturation in the superior or inferior vena cava may not be identical to that of mixed venous blood, due to variations in flow and oxygen consumption between the upper and lower parts of the body. As an example, in situations of shock, oxygen extraction increases in non-vital territories such as the hepatosplanchnic region, leading to a decrease in inferior vena cava oxygen saturation – with a resulting increase in the difference between mixed venous blood saturation and the saturation value that can be registered with a catheter positioned in the superior vena cava. Recently, good correlation and parallelism have been observed between mixed venous blood saturation and saturation obtained with a catheter located in the superior vena cava (SvcO2) in critical patients, in a range of clinical situations,17 though SvcO2 effectively may overestimate SvO2 by about 5%.18,19 Pragmatically, the presence of SvcO2<60% in the general critical patient population is associated with increased mortality,20 and in septic patients resuscitation based on therapeutic objectives maintaining SvcO2≥70% improves morbidity and mortality.15 Recently, the Surviving Sepsis Campaign has acknowledged the numerical difference between SvO2 and SvcO2, recommending SvO2 65% and SvcO2 70% in the resuscitation of these pacientes.21
Mixed venous blood or blood from the superior cava vein can be analyzed with a co-oximeter on a discontinuous basis or, ideally, saturation can be continuously monitored using fiber optic technology incorporated to pulmonary artery or central venous catheters. These systems for the continuous measurement of venous oxygen saturation are based on the reflectance spectrophotometry principle.22,23 Two fiber optic channels are used to transmit and receive light beams of wavelengths selected according to the reflectance characteristics of total hemoglobin and oxyhemoglobin. The relative fraction of total hemoglobin corresponding to oxyhemoglobin represents oxygen saturation. These systems must be calibrated before insertion and, in general, recalibration is required if they are disconnected from the optic module. Recalibration is also advisable every 24h and before any important therapeutic intervention is carried out, according to the changes in venous blood saturation-even in the absence of warnings or alerts referred to signal quality.22,23
LactateThe point where oxygen consumption begins to decrease when tissue oxygen transport progressively decreases coincides with the moment in which lactate concentration increases.24 On the other hand, a relationship has been demonstrated between lactate concentration and a situation of dependency between oxygen transport and consumption25 and the presence of low SvcO215 values. These observations have led to the concept that elevated lactate concentrations are indicative of tissue hypoxia and anaerobic metabolism. However, it must be taken into account that the mitochondrial redox state is not reflected by lactate concentration but by the lactate/pyruvate ratio, or by the acetoacetate/betahydroxybutyrate ratio. Likewise, other mechanisms not related to cellular hypoxia and anaerobic metabolism may explain the elevation of lactate concentration in the critical patient. These mechanisms include the following: (a) increased glycolytic rates characteristic of inflammatory situations; (b) diminished liver lactate clearance as has been described in patients with sepsis, liver failure, liver surgery or heart surgery; (c) mitochondrial dysfunction in the context of cytopathic hypoxia (worsening of mitochondrial function due for example to the formation of nitric oxide and peroxynitrite); (d) worsening of pyruvate dehydrogenase function (needed for pyruvate entry to the Krebs cycle, the activity of which is inhibited in sepsis); and (e) the administration of drugs such as antiretroviral agents (nucleoside reverse transcriptase inhibitors (NRTIs), which induce alterations in mitochondrial function), metformin (particularly in renal failure), adrenalin (which induces an increase in glycolysis) and ethyleneglycol (laboratory artifact), cyanide or methanol intoxication (which inhibit the cellular respiratory chain).
In chemical reactions that lead to lactate production from glucose, hydrogen ions are not produced; as a result, lactate production does not give rise to acidosis. The coexistence of hyperlactatemia and acidosis is a coincidence not due to any causal relationship but to the fact that both changes (hyperlactatemia and acidosis) can have common causes. Lactate concentration is not related to the pH value, base excess or the anion gap.26,27 Acidosis under conditions of cellular hypoxia is due to the formation of hydrogen ions during ATP hydrolysis that are not reused for the formation of ATP, due to the absence of available oxygen. Therefore, the coexistence of hyperlactatemia with acidosis could be used to define whether the cause of increased lactate concentration is due to cellular hypoxia or to other causes.28
The lactate concentration values in blood are associated to mortality.29,30 In a group of patients in which lactate concentration was determined during pre-hospital monitorization, mortality was correlated to the degree of hyperlactatemia,31 and in a multivariate analysis only lactate was associated to hospital mortality. In a group of critical patients with acidosis, mortality among the individuals with metabolic acidosis was greater than in those with non-metabolic acidosis. The patients with lactic acidosis suffered greater mortality than the patients with acidosis secondary to an increase in the strong ion gap differences or to hyperchloremic acidosis.32 In a multivariate analysis, lactate concentration, the strong ion gap difference, phosphate concentration and age were identified as independent predictors of mortality. Lastly, observational studies using a therapeutic algorithm have shown that in patients in which lactate concentration is not normalized, the mortality rate is higher than that in patients in which the concentration is normalized.33 To date, only one randomized clinical trial has evaluated the effect of interventions aimed at correcting hyperlactatemia. This study, conducted in heart surgery patients, reported a decrease in mortality in those patients in which oxygen transport was increased when the lactate concentration values increased or failed to normalize.34
The recommendations of different scientific societies include the determination of lactate during resuscitation of patients in shock. The Society of Critical Care Medicine considers lactate concentration in blood (≥4mmol/l) as one of the indications for starting goal-guided therapy in severe sepsis.35 The trauma resuscitation guides of the Eastern Association for the Surgery of Trauma recommend the utilization of lactate concentration as one of the resuscitation goals or objectives, recognizing that there is no evidence on the impact of this intervention upon mortality.36 The international consensus conference on hemodynamic monitorization in shock (Paris, 2006) established that: (a) lactate is recommended as a marker for the diagnosis and determination of shock stage; (b) despite its limitations, lactate is a good surrogate marker of tissue hypoperfusion in shock; (c) the gradual reduction of lactate concentration in blood, and the correction of acidosis probably reflect the restoration of blood flow to the organs; and (d) the determination of lactate and base excess is useful in septic shock patients. The final recommendations of the conference include the proposal to perform serial determinations of base excess or lactate as prognostic predictors.2
In those studies that have compared resuscitation protocols including the monitorization of lactate concentration, the application of such a protocol leads to increased administration of fluids, vasoactive drugs, blood transfusions, neuromuscular blockers, sedatives and analgesics.37
The determination of lactate concentration is inexpensive and reproducible. Only correct interpretation on the part of the physician of the physiology of lactate metabolism can allow correct interpretation of the meaning of an increase in lactate concentration. As with any other monitorization method, clinical outcome is not conditioned by the lactate measurement as such but rather by physician response to the measured variable. The existing evidence suggests that: (a) lactate determination is useful for stratifying patient risk; (b) lactate should be measured directly, since it cannot be estimated from other variables such as pH or base excess; (c) the elevation of lactate concentration in blood in the acute phase of resuscitation is very probably indicative of tissue hypoxia, and actions must be taken to restore perfusion and tissue oxygenation; (d) moderate lactate elevations in apparently resuscitated patients are difficult to interpret, but may be explained by occult hypoxia of certain tissues and other mechanisms unrelated to tissue hypoxia or anaerobic metabolism (e.g., diminished pyruvate dehydrogenase activity, increased glycolysis, reduced liver clearance); and (e) it is not clear whether the determination of blood lactate concentration as a therapeutic guide during the resuscitation of shock patients improves the prognosis.
The assessment of lactate concentration requires accuracy of measurement. The values obtained corresponding to blood from different compartments (capillary blood, venous blood and mixed venous blood) are similar, though slightly higher in venous blood, due to cell metabolism. The concentration can increase if the determination is not made immediately, due to the persistence of glycolysis in the blood sample – particularly under conditions of leukocytosis and increased hematocrit. In order to avoid this effect, it is advisable to perform determination less than 15min after extraction, or to store the sample at −4°C. The infusion of Ringer lactate does not affect lactate determination, provided blood sampling is carried out at a distance from the infusion site. The use of renal filtration techniques slightly lowers the lactate concentration, but does not interfere with monitorization of its concentration. It should be taken into account that the use during the dialysis technique of replacement fluids containing lactate can give rise to an increase in the concentration of lactate.
Acid–base equilibriumIn addition to its impact upon lactate production, tissue hypoperfusion in the patient with cardiovascular failure produces an anion increment secondary to anaerobic metabolism and a CO2 washout defect globally resulting in an alteration of the pH value. In the era before the easy availability of lactate testing in most hospital laboratories, the standard base excess (SBE) was used as surrogate value. However, in the same way as with lactic acid, tissue hypoxia is not the only cause of alterations in acid–base equilibrium in the critical patient with hemodynamic instability. Hyperchloremic acidosis of intrinsic or iatrogenic cause, renal failure, hypoalbuminemia, toxicity caused by certain drugs or hypophosphatemia are frequent alterations in critical patients that can also produce alterations in acid–base equilibrium. In addition, the methods for calculating SBE lose reliability in critically ill patients on assuming normality of the set of ions and cations that have not been measured. Calculation of the anion gap, and in particular of the strong ion gap (SIG), allows us to unmask such situations and quantify the contribution of the different imbalances to the overall SBE alteration. Nevertheless, SIG also has limitations, and to date it has not been shown to be superior to the measurement of base excess as a guide to resuscitation and/or prediction of mortality.38–40 Thus, SBE evaluation is useful for classifying the nature of the pH alteration in shock patients, while SIG allows us to quantify and define the cause of the disorder.
Standard base excess and the lactate values upon admission are of similar usefulness as prognostic indicators in critical patients, though lactate evolution in the first 48h has been shown to be superior to the evolution of SBE – since other disorders determinant of SBE and different from cellular hypoxia may appear or worsen.41–43 An SBE cutoff value of <−2mEq/l is similar in usefulness to <−5mEq/l in determining the presence of metabolic acidosis and in assessing the prognosis.43 In addition, SBE also complements the interpretation of lactate, since the presence of lactic acidosis is associated to a poorer prognosis than isolated lactate elevation without SBE alterations. When hyperlactatemia is not accompanied by SBE alterations, other causes of lactate elevation different from tissue hypoperfusion must be discarded.44
Arteriovenous CO2 differenceThe arteriovenous pCO2 difference, whether corresponding to mixed venous blood – P(v-a)CO2 – or central venous blood – P(vc-a)CO2 – has been regarded as a marker of the capacity of the cardiovascular system to eliminate the CO2 produced in the peripheral tissues.45,46 In fact, P(v-a)CO2 is inversely correlated to the cardiac index in different situations of cardiovascular failure.47,48 In a recent study, P(vc-a)CO2 has demonstrated its value in the detection of hypoperfusion in already resuscitated patients in which SvcO2 values of over 70% had been reached.49 Based on the supplied evidence, P(vc-a)CO2 values above 6mmHg could indicate the persistence of peripheral hypoperfusion, even with “normalized” SvcO2 values. However, the usefulness of this parameter in resuscitation algorithms, as well as its best cutoff value, remains to be established.
Study of regional circulation and microcirculationAlthough the initial objectives of hemodynamic monitorization center on the restoration of global macrocirculatory variables, in recent years the evidence that heterogeneity in the perfusion of tissues and microcirculatory alterations play a key role in the development of organ failure has led to growing interest in new technologies designed to evaluate regional circulation and microcirculation. However, it is important to remember that despite the prognostic value shown by many of these variables, their impact in application to the guiding of resuscitation has not been evaluated. A description is provided below of the main technologies currently available for the study of regional circulation and microcirculation.
Mucosal CO2 monitorization: gastric tonometry and sublingual capnometryWhen referring to regional tissue oxygenation parameters, the study of partial CO2 pressure (pCO2) in the mucosal membranes deserves special mention. CO2 is a natural product of aerobic cellular metabolism. Under conditions of anaerobiosis, the production of CO2 is increased. Thus, the CO2 concentration found in the tissues depends on the degree of production of CO2 (fundamentally based upon basal metabolism and/or the degree of anaerobiosis) and on the degree of tissue perfusion (not only due to anaerobiosis, but also to the washout of such CO2).50 The CO2 value in the tissues is influenced by arterial pCO2; accordingly, a more correct way to assess mucosal pCO2 is calculation of the gradient between the latter and arterial pCO2 – this being referred to as the of CO2 gap (pCO2-gap), as mentioned on evaluating the systemic arteriovenous CO2 difference.
Since the anatomical characteristics of the intestinal mucosa make it particularly vulnerable to hypoxia, gastric tonometry was the technique that initially generated special interest. Values of pCO2-gap above 20mmHg were able to discriminate between survivors and non-survivors in a general critical patient population.51 In addition, in severe septic patients, gastric pCO2 showed greater prognostic value when other hemodynamic flow variables had been corrected.52 In a multicenter prospective study, Gutiérrez et al.53 showed resuscitation guided to maintain normal gastric mucosal pH values (pHi) to be associated to improved prognosis in patients with initial pHi>7.35. In contrast, no beneficial effects were observed in the group of patients with an initial pHi below this value. Other prospective studies have not been able to demonstrate the benefit of using gastric tonometry in the resuscitation process.54 Unfortunately, gastric tonometry has largely been obviated as a result of technical difficulties such as the complexity of the measurements and the interference of factors such as enteral nutrition or duodenogastric reflux.
Posterior technological developments led to the possibility of measuring pCO2 in the sublingual mucosa in a noninvasive manner, by means of electrodes. In this context, pCO2 in the sublingual mucosa had shown (in the same way as gastric tonometry) its prognostic value in different critical patient populations.50,55 Recently, the group led by Vincent reported an inverse correlation between sublingual pCO2 values and the perfused capillary density in the sublingual mucosa in a septic patient population.56 This technology, while very attractive, has not yet been developed for clinical use, and is presently confined to experimental studies.
Spectroscopy (NIRS)Near-infrared spectroscopy (NIRS) is based on the capacity of different chromophores present in tissues to absorb light in the wavelength range of 700–1000nm. Analysis of the light emitted and the light received allows this technology to offer a noninvasive and continuous semiquantitative calculation of the degree of oxyhemoglobin saturation in the recorded area (StO2).57 NIRS can only sense blood vessels with a caliber of under 1mm; it therefore provides a value that reflects the amount of oxyhemoglobin present in the compartment composed of arterioles, capillaries and venules.57 Under basal conditions, 75% of the blood in the skeletal muscles is located in the venous compartment. As a result, in healthy individuals, StO2 mainly reflects local venous oxygen saturation. In healthy volunteers, basal StO2 values of 86±6% have been reported in the thenar prominence.58
The usefulness of StO2 in the detection of tissue hypoxia has been examined in different groups of diseases. In experimental models of hemorrhagic shock, StO2 has been seen to decrease parallel to the drop in MBP, SvO2 and DO2.59 The correlation of the absolute StO2 value to a global hypoperfusion parameter such as SvcO2 has been assessed in different critical patient populations.60,61 Thus, in septic patients, StO2 values under 75% are strongly predictive of low SvcO2.61 In a multicenter prospective study of trauma patients, StO2 values below 75% were associated to greater organ failure and mortality – with a predictive value similar to that of base excess.62 Unfortunately, the absolute StO2 value appears to have low sensitivity in detecting tissue hypoperfusion, and there is important overlap between pathological values and the values obtained under normal conditions.63
The analysis of the changes in StO2 produced by transient ischemic maneuvering (vascular occlusion test, VOT) as a dynamic tool for better exploring microcirculatory dysfunction has added to the clinical value of this technology. The deoxygenation (DeOx) and reoxygenation gradients (ReOx) have been evaluated mainly in groups of septic patients, and alterations of their values have been shown to have prognostic implications.64–66 Thus, Creteur et al. have found that the evolution of the ReOx gradient in septic patients in the first 72h after admission allow discrimination between survivors and non-survivors.66 However, the usefulness of both gradients in guiding the resuscitation process has not been explored to date.
Videomicroscopy: orthogonal polarization spectral (OPS) and sidestream darkfield imaging (SDF)Orthogonal polarization spectral (OPS) and sidestream darkfield imaging (SDF) are two videomicroscopic techniques, based on the same physical principles that have recently been developed for use at the patient bedside to obtain microcirculatory images in real time. These techniques are fundamentally on the erythrocyte hemoglobin light absorption and reflection properties at a certain wavelength (530nm). Since this light is absorbed by hemoglobin, the end composition of the resulting image is formed by the erythrocyte flow in gray/black within the capillaries (absorbed light), with the rest of the tissue appearing in light color (reflected light). We thus have an image of the capillaries though retroillumination of the circulating erythrocytes, though the capillaries not containing erythrocytes are not seen. The main difference between the two technologies is that polarized light is used in OPS, while pulses of green light are used in SDF. The portable nature of these technologies (involving devices the size of a minicamera) makes them particularly attractive.
The mucosal membranes are ideal structures for monitorization with these techniques, since they are very thin and accessible from the exterior. The oral mucosa and specifically the sublingual mucosa are the points most commonly used in clinical practice. Different semiquantitative indexes have been used in processing and interpreting the images obtained, with a view to assessing the quality of regional perfusion.67 No consensus-based normal reference values have been found in the literature; the evidence is therefore derived from the use of these variables as relative values that are compared with the same values from control groups, or the same group in another phase of the study design.
The videomicroscopic application that has generated most information in the literature is the study of distributive shock, represented mainly by septic shock.68,69 The most important distinguishing characteristic in distributive shock is that despite restoration of the capacity to generate blood flow, good tissue perfusion is not guaranteed.70 Elbers and Ince71 have defined different microcirculatory patterns within distributive shock, ranging from pattern I (capillary stasis) to pattern V (capillary hyperdynamism). Two observational studies in septic shock patients have reported poorer initial perfusion indexes in patients who died versus the survivors.72 Likewise, the survivors were the subjects showing the fastest improvement of these perfusion indexes.73 This technology, therefore, allows us to come exceptionally close to the last frontier of tissue perfusion. However, despite the fact that the perspectives for use are very good in the research setting, its clinical application poses some important limitations: (a) distributive shock is characterized by great heterogeneity between different tissue compartments, and so the sublingual microcirculation may not be representative of the rest of tissues68; (b) laborious image processing is required to obtain the functional capillary density, as a result of which the technique is rather cumbersome for clinical use; and (c) there are difficulties in obtaining static images for posterior processing, since the device must be held manually within the mouth of the patient.
Thus, although local perfusion monitorization with the described new technologies has been seen to be of prognostic value, at present, and with the exception of a single gastric tonometry study,53 none of these parameters have generated evidence supporting their usefulness in guiding the resuscitation process.
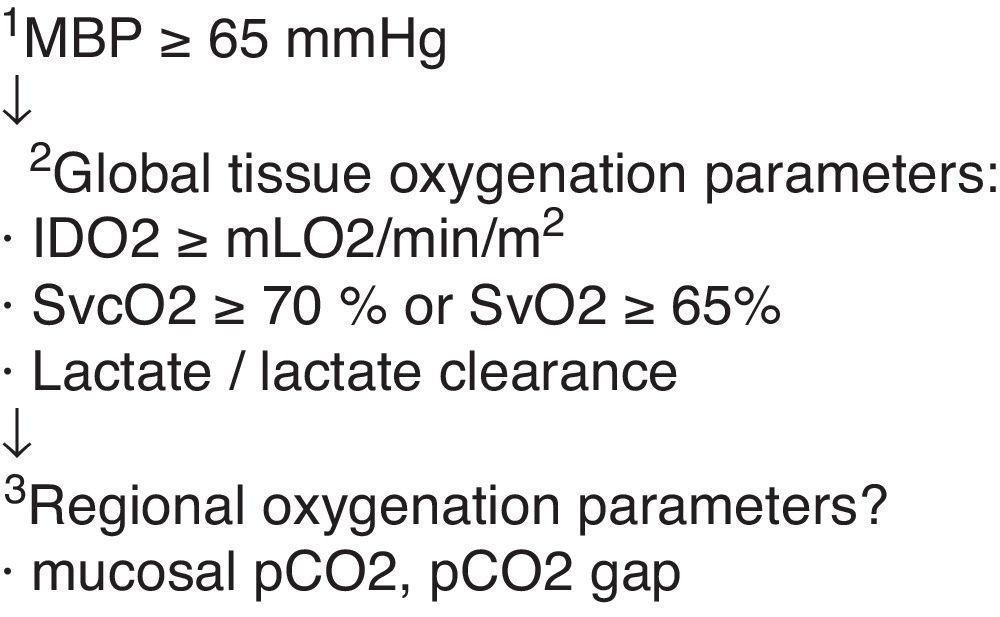
ConclusionsHemodynamic resuscitation should aim to rapidly secure adequate tissue perfusion pressure values (MBP), and the resuscitation process should be guided by physiological and metabolic variables of use in detecting global tissue dysoxia. At present, the most useful variables in the detection of tissue hypoxia are blood lactate and venous oxygen saturations (SvO2 and SvcO2). Thus, hemodynamic resuscitation should focus on restoring physiological values of SvO2/SvcO2, and on the resolution of lactic acidosis and/or hyperlactatemia (Fig. 1).
Finally, the future of hemodynamic resuscitation could involve the use of variables capable of assessing the degree of perfusion on a more localized basis. In this context, although the monitorization of regional parameters is attractive and has demonstrated its prognostic value, the existing evidence is still too limited to allow such parameters to be applied in guiding the resuscitation process.
Please cite this article as: Mesquida J, et al. Objetivos de la reanimación hemodinámica. Med Intensiva. 2011;35:499–508.