To evaluate the outcome of tracheotomized patients after reintubation.
MethodSecondary analysis from a prospective, multicenter and observational study including 36 Intensive Care Units (ICUs) from 8 countries was carried out.
PatientsA total of 180 patients under mechanical ventilation for more than 48h, were extubated and reintubated within 48h.
InterventionsNone.
OutcomesICU mortality, length of ICU stay, organ failure.
ResultsFifty-two patients (29%) underwent tracheotomy after reintubation. The median time from reintubation to tracheotomy was 2.5 days (interquartile range (IQR) 1–8 days). The length of ICU stay was significantly longer in the tracheotomy group as compared with the group without tracheotomy (median time 25 days, IQR 17–43 versus 16.5 days (IQR 11–25); p<0.001). ICU mortality in the tracheotomy group was not significantly different (31% vs 27%; p=0.57).
ConclusionsIn our cohort of reintubated patients, tracheotomy is a common procedure in the ICU. Patients with tracheotomy had an outcome similar to those without tracheotomy.
Evaluar el desenlace de pacientes que fueron traqueotomizados tras una reintubación.
DiseñoAnálisis secundario de un estudio de cohorte prospectivo.
ÁmbitoTreinta y seis unidades de cuidados intensivos de 8 países.
Pacientes180 pacientes con ventilación mecánica durante más de 48 horas extubados y que requirieron reintubación en las primeras 48 horas.
IntervencionesNinguna.
Variables de interés principalMortalidad en la Unidad de Cuidados Intensivos, días de estancia en la unidad de cuidados intensivos, fracaso de órganos.
ResultadosCincuenta y dos pacientes (29%) fueron traqueotomizados inicialmente después de reintubación. La mediana de tiempo desde la reintubación a la traqueotomía fue de 2,5 días (rango inter-cuartil: 1, 8). La duración de la estancia en la UCI fue significativamente mayor en el grupo de traqueotomía, en comparación con el grupo inicialmente sin traqueotomía [mediana de 25 días (rango inter-cuartil: 17, 43) versus 16,5 días (rango inter-cuartil: 11, 25); p <0,001]. En el grupo de traqueotomía no se observó una menor mortalidad (31% frente al 27%; p=0,57).
ConclusionesEn nuestra cohorte, la traqueotomía después de reintubación es un procedimiento común pero no ofrece ninguna ventaja significativa.
Tracheotomy is a common practice in patients admitted to the Intensive Care Unit (ICU) and subjected to mechanical ventilation.1–3 The technique offers a number of potential advantages over prolonged translaryngeal intubation in terms of patient comfort, a lesser need for sedation, and improved weaning from the ventilator.3,4 One-third of all the tracheotomies are performed in situations where programmed extubation has failed and reintubation is required.3 However, little information is available on the possible benefits of tracheotomy in the initial days after reintubation. The present study analyzes the outcome of patients with tracheotomy after failure of extubation as compared with patients in whom tracheotomy was not performed.
Patients and methodsA secondary analysis was performed of an international, multicenter prospective study carried out in 36 ICUs in 8 countries (see Appendix A) between September 2005 and December 2006.5 Given the observational and non-interventional nature of its design, the corresponding Ethics Committee approved the study without the need for informed consent.
PatientsWe included adult patients requiring mechanical ventilation for more than 48h and with programmed extubation after a successful spontaneous breathing test. Patients with previous tracheotomy were excluded.
Follow-upThe included patients were evaluated daily to identify the criteria for conducting a spontaneous breathing test: (a) resolution or improvement of the condition leading to the need for mechanical ventilation; (b) patient alertness and capacity to communicate; (c) core temperature <38°C; (d) absence of vasoactive medication (with exclusion of dopamine <5μg/kg/min); and (e) a PaO2/FiO2 ratio of >200 with positive end-expiratory pressure (PEEP) no greater than 5cmH2O. When the patients met these criteria, a spontaneous breathing test was performed with a T-tube or continuous positive airway pressure (CPAP), or supportive pressure ≤7cmH2O. After 5min and at the end of the spontaneous breathing test, we recorded the following variables: arterial blood gas values, tidal volume measured with a spirometer or from the ventilator, respiratory frequency, heart rate, systolic blood pressure, and the Richmond agitation-sedation scale (RASS). The physician in charge determined whether the patient presented any of the following signs of poor tolerance: a respiratory frequency of >35rpm, SatO2<90%, a heart rate of >140bpm, or an increase or decrease in heart rate of over 20% with respect to the basal rate, systolic blood pressure >200mmHg or <80mmHg, and agitation, perspiration or anxiety. The patients who failed to tolerate the spontaneous breathing test received mechanical ventilation. In these patients, a daily spontaneous breathing test was made until the time of extubation. To the effects of the study, the analysis included the data corresponding to the spontaneous breathing tests that were followed by extubation.
The patients who tolerated the spontaneous breathing test were extubated in the subsequent 120min after the start of the test and were subjected to follow-up during the next 48h or until discharge from the ICU – whichever occurred first. The decision to remove the tube was taken by the physician in charge of the patient. Given the observational and non-interventional nature of the study, the criteria for indicating reintubation were not protocolized.
In the case of reintubation, we recorded the date and time, as well as the reason for reintubation, previously classified as: upper airway obstruction (defined as stridor and/or laryngeal edema), increased respiratory effort (defined as a respiratory frequency >35rpm and/or use of the accessory muscles), diminished consciousness (defined as a score of under 0 on the Richmond agitation-sedation scale), hypoxemia (defined as SatO2<90% despite FiO2>0.5), or respiratory acidosis (defined as arterial pH<7.30 with PaCO2>50mmHg). The reintubated patients were followed-up on during the new period of mechanical ventilation for a maximum of 15 days. During this time, a daily registry was made of the appearance of new complications after reintubation such as acute respiratory distress syndrome, sepsis, ventilator-associated pneumonia (VAP), or organ failure (cardiovascular, renal, hepatic, hematological), defined as a score of over two points on the Sepsis-related Organ Failure Assessment (SOFA) scale.
During the follow-up period, the performance and date of tracheotomy were recorded (the indications of tracheotomy were not protocolized), or the date of the second extubation was registered. The reintubated patients were classified into two groups according to the performance or not of tracheotomy: tracheotomy group (patients subjected to tracheotomy after first reintubation) and non-tracheotomy group. The patient condition at discharge from the ICU was documented in all cases.
Statistical analysisThe data are expressed as percentage, mean (standard deviation) and median (interquartile range), as applicable. Continuous variables were compared using the Student t-test or Mann–Whitney U-test, while categorical variables were compared using the chi-squared test or the Fisher exact test. Multiple linear regression analysis was performed to identify the independent variables associated to the duration of stay in the ICU. The following variables were included in the model: age, SAPS II score, initial reason for mechanical ventilation, days of mechanical ventilation prior to first extubation, tracheotomy and post-reintubation complications. Statistical significance was considered for p<0.05. The SPSS version 17.0 statistical package (SPSS Inc., Chicago, IL, USA) was used throughout.
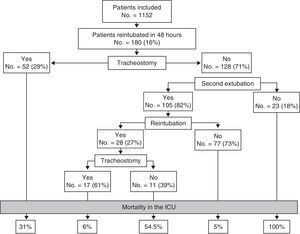
ResultsFrom a cohort of 1152 patients subjected to programmed extubation, we analyzed 180 reintubated patients (16%), divided into two groups: 52 patients (29%) tracheotomized after reintubation and 128 patients in principle not subjected to tracheotomy (Fig. 1). The median time from reintubation to tracheotomy was 2.5 days (interquartile range 1.8). Table 1 compares the basal characteristics of the two groups. In the tracheotomy group there were more patients requiring mechanical ventilation due to neurological disease (23% vs 11%, p=0.04), while the non-tracheotomy group was characterized by more patients with pneumonia (19% vs 6%, p=0.03). The patients with tracheotomy had a higher incidence of sepsis and ventilator associated pneumonia after reintubation (Table 1).
Comparison of the basal characteristics and complications after reintubation in both groups.
| Tracheotomy (No.=52) | No tracheotomy (No.=128) | p-Value | |
| Basal characteristics | |||
| Age, mean (SD), years | 62 (17) | 61 (18) | 0.83 |
| Females, n (%) | 22 (36) | 46 (42) | 0.42 |
| SAPS II upon admission, mean (SD), points | 45 (15) | 44 (13) | 0.49 |
| Cause of start of mechanical ventilation, n (%) | |||
| Chronic obstructive pulmonary disease | 7 (13) | 15 (12) | 0.75 |
| Asthma | – | 1 (0.8) | 1.00 |
| Acute respiratory failure | |||
| Postoperative | 7 (13) | 20 (16) | 0.71 |
| Pneumonia | 3 (6) | 24 (19) | 0.03 |
| Sepsis | 5 (10) | 13 (10) | 0.91 |
| Trauma | 4 (7) | 9 (7) | 1.00 |
| Congestive heart failure | 2 (4) | 6 (5) | 1.00 |
| Cardiac arrest | 2 (4) | 3 (2) | 0.63 |
| Acute respiratory distress syndrome | – | 8 (0.3) | 0.11 |
| Aspiration | – | 6 (5) | 0.18 |
| Others | 9 (17) | 8 (6) | 0.04 |
| Neurological disease | 12 (23) | 14 (11) | 0.04 |
| Neuromuscular disease | 1 (2) | 1 (1) | 0.49 |
| Mechanical ventilation prior to extubation, median (interquartile range), days | 9 (5, 12) | 7 (4, 10) | 0.07 |
| Richmond agitation-sedation score at the time of extubation, n (%) | |||
| −5 to −1 | 8 (15) | 32 (25) | 0.16 |
| 0 | 36 (69) | 79 (62) | 0.34 |
| +1 to +4 | 8 (15) | 17 (13) | 0.71 |
| Richmond agitation-sedation score before reintubation, n (%) | |||
| −5 to −1 | 13 (25) | 26 (20) | 0.49 |
| 0 | 28 (54) | 80 (63) | 0.24 |
| +1 to +4 | 11 (21) | 22 (17) | 0.53 |
| Time to reintubation, median (interquartile range), h | 13 (6, 23) | 13 (6, 24) | 0.72 |
| Reason for reintubation, n (%) | |||
| Upper airway obstruction | 12 (9) | 4 (8) | 0.72 |
| Increased respiratory effort | 57 (44.5) | 32 (61.5) | 0.04 |
| Diminished consciousness | 17 (13) | 6 (11) | 0.75 |
| Hypoxemia | 27 (21) | 5 (10) | 0.07 |
| Respiratory acidosis | 15 (12) | 5 (10) | 0.68 |
| Complications after reintubation | |||
| Acute respiratory distress syndrome, n (%) | 7 (13.5) | 15 (12) | 0.75 |
| Ventilator associated pneumonia, n (%) | 21 (40) | 34 (27) | 0.07 |
| Sepsis, n (%) | 16 (31) | 22 (17) | 0.04 |
| Organ failure, n (%) | |||
| Cardiovascular failure | 18 (35) | 31 (24) | 0.15 |
| Renal failure | 7 (13.5) | 14 (11) | 0.63 |
| Liver failure | 4 (8) | 11 (9) | 1.00 |
| Hematological failure | 6 (11.5) | 6 (5) | 0.09 |
SD: standard deviation.
The tracheotomy group had a significantly longer stay than the non-tracheotomized patients (Table 2). In the multiple linear regression analysis, three variables were associated with a longer stay in the ICU: days of mechanical ventilation prior to extubation (p<0.001), post-reintubation sepsis (p<0.001) and tracheotomy (p=0.025).
Comparison of the main outcome variables.
| Tracheotomy (No.=52) | No tracheotomy (No.=128) | p-Value | |
| Days from reintubation to discharge from the ICU, median (interquartile range) | 16 (7, 29) | 8 (4, 15) | <0.001 |
| Survived | 15 (5, 31) | 8 (5.14) | <0.001 |
| Deceased | 16 (12, 29) | 8 (2, 19) | <0.001 |
| Days of stay in the ICU, median (interquartile range) | 25 (17, 43) | 16.5 (11, 25) | <0.001 |
| Survived | 25 (14, 48) | 16 (11, 24) | <0.001 |
| Deceased | 26 (42, 23) | 20 (11, 31) | <0.001 |
| Mortality in the ICU, n (%) | 16 (31) | 34 (27) | 0.57 |
The mortality rate in the ICU proved similar in both groups: 31% in the tracheotomy group versus 27% in the non-tracheotomy group (relative risk of tracheotomy: 1.16; 95% confidence interval: 0.70–1.90; p=0.57).
The mortality rate was similar in the patients with early tracheotomy (in the first 3 days after reintubation) and in those in which tracheotomy was performed after the third post-extubation day: 32% versus 29% (p=0.82).
DiscussionThe main finding of this observational study is that tracheotomy in patients who have required reintubation does not offer advantages in terms of the duration of stay in the ICU or mortality as compared with patients in which tracheotomy is not performed after the first reintubation.
In recent years there has been a significant increase in the number of tracheotomies performed in patients subjected to mechanical ventilation,6 this being partially conditioned by introduction of the percutaneous technique in routine clinical practice.7,8 Tracheotomy, in comparison to prolonged translaryngeal intubation, has demonstrated advantages in terms of patient comfort, a lesser need for sedation, oral intake, improved oral hygiene, or a faster recovery of speech.9 There is greater controversy regarding its possible advantages related to other clinical outcomes such as the incidence of ventilator associated pneumonia,10 faster weaning from mechanical ventilation,11 patient safety12,13 or, most importantly, mortality and the duration of stay in the ICU.
A recent metaanalysis14 including 7 randomized clinical trials comparing early tracheotomy versus late tracheotomy or prolonged intubation has found that early tracheotomy does not reduce mortality during the first 90 days of stay (relative risk: 0.86; 95% confidence interval: 0.65–1.13). Early tracheotomy likewise is not associated with a shortening of stay in the ICU (weighted mean difference: −6.93 days; 95% confidence interval: −16.50 to 2.63).
In addition to either early or late, tracheotomy can be classified in relation to the course of mechanical ventilation: during ventilatory support, during weaning from mechanical ventilation or after the failure of extubation and the start of a new episode of mechanical ventilation. In a previous analysis by our group, we found that in one-third of the patients tracheotomy was performed after the failure of extubation.5 To date, no study had evaluated the effect of tracheotomy in the subgroup of patients who are tracheotomized after reintubation due to post-extubation respiratory failure.
Our study has shown that independently of other variables, patients with tracheotomy after reintubation had a longer stay. In contrast to other observational studies4,15–18 in which tracheotomized patients were reported to have lesser mortality in the ICU, in our patient cohort the mortality rate was similar in both groups–this observation probably being related to differences in the populations included in the studies.
Our study has a number of limitations. Firstly, the limited sample size may have accounted for some of the observations, and precluded the use of more sophisticated statistical analyses such as for example a trend index to determine the individual probability of tracheotomy, which would have allowed a better estimation of the effect of tracheotomy upon the primary outcome variable. Secondly, the observational, non-interventional nature of the study implies that neither the decision to reintubate nor the decision to perform tracheotomy was protocolized, and was left to the criterion of the physician in charge of the patient. In this context, there may have been selection bias, since on one hand tracheotomy was more frequent in patients in which coma constituted the indication of ventilation–this population presenting a poorer prognosis19–while on the other hand tracheotomy is usually decided in patients considered to have a more favorable vital prognosis. In our study there were no differences in severity upon admission to the ICU, though no severity index was recorded at the time of reintubation or at the time of tracheotomy.
In conclusion, we have not found tracheotomy after failed extubation to offer advantages over the maintenance of translaryngeal intubation. In any case, these findings must be considered to serve the purpose of generating hypotheses, and the true effect of tracheotomy after reintubation must be evaluated in the context of a randomized, prospective and controlled clinical trial.
Financial supportThis study has been funded by the CIBER de Enfermedades Respiratorias, Instituto Carlos III, Spain.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The collaborating investigators who participated in this study were:
Argentina: Coordinator: Carlos Apezteguia (Hospital Profesor A. Posadas, El Palomar, Buenos Aires). Investigators: Fernando Villarejo, Enrique Pezzola, Juan Hidalgo (Hospital Profesor A. Posadas, Buenos Aires); Margarita Tavella, Roberto Villa (Hospital de Clínicas José de San Martín, Buenos Aires); Luis Pablo Cardonet, Ana Rosa Diez, Verónica Fernandes (Hospital Provincial del Centenario, Rosario); Christian Casabella, Fernando Palizas Jr (Clínica Bazterrica, Buenos Aires); Gonzalo Ferrara, America Toro (HIGA San Martín de la Plata, Buenos Aires); Enrique Pablo Centeno, Martin Eduardo Arzel (Hospital de González Catán); Ariel Chena, Graciela Zakaik (Hospital Luis Lagomaggiore, Mendoza); Martin Deheza, Marina Papucci (Hospital General de Agudos Bernardino Rivadavia, Buenos Aires); Pablo Pratesi, Javier Álvarez (Hospital Universitario Austral, Derqui); Miriam Moseinco, Marcelo Engel (Sanatorio Otamendi y Miroli, Buenos Aires); Alejandra Balbiani, Orlando Hamada (Hospital San Juan de Dios, Ramos Mejia); Patricia Spinelli, Imelda Perdomo (Sanatorio Trinidad San Isidro); Sergio Lasdica, Rogelio Urizar (Hospital Municipal de Coronel Suárez Dr. Raúl Caccavo).
Bolivia: Fredi Sandi Lora, Fernando Renjel Jáuregui (Hospital Obrero número 1, La Paz).
Colombia: Coordinator: Marco A. González (Clínica Medellín y Universidad Pontificia Bolivariana, Medellín). Investigators: Marcela Granados (Fundación del Valle del Lilly, Cali), Rubén Camargo (Hospital General del Norte), Carmelo Dueñas (Hospital Bocagrande, Cartagena), Guillermo Ortiz (Hospital Santa Clara, Bogota), Francisco Molina (Clínica Universitaria Bolivariana, Medellín).
Saudi Arabia: Yaseen Arabi (King Fahad National Guard Hospital, Riyadh), Jamal A. Alhashemi (King Abdulaziz University, Jeddah).
Spain: Coordinator: Federico Gordo (Hospital del Henares, Coslada).
Eva Manteiga, Oscar Martínez, Oscar Peñuelas (Hospital Universitario de Getafe); Jordi Ibáñez (Hospital Son Dureta, Palma de Mallorca); Marta López (Hospital Marqués de Valdecilla, Santander); Enrique Calvo Herranz (Fundación Hospital Alcorcón); Luís Eugenio Palazón (Hospital General Universitario Reina Sofía, Murcia); Enrique Fernández Mondéjar (Hospital Virgen de las Nieves, Granada), Rafael Fernández (Hospital de Sabadell); Noelia Lázaro, Santiago Macias (Hospital General de Segovia); Ángela Alonso (Hospital de Fuenlabrada); Raúl de Pablo (Hospital Príncipe de Asturias, Alcalá de Henares), Guillermo Muñiz Albaiceta (Hospital Central de Asturias, Oviedo); Margarita Mas (Hospital de Móstoles); Gemma Rialp (Hospital Son LLàtzer, Palma de Mallorca), Arantxa Mas (Fundación Altahaia, Manresa).
United States: Marcos I. Restrepo, Antonio Anzueto (South Texas Veterans Health Care System Audie L. Murphy Division and University of Texas Health Science Center, San Antonio, Texas).
Uruguay: Cristina Santos (Hospital de Clínicas de Montevideo).
Venezuela: Fernando Pérez (Hospital de Clínicas de Caracas).
Please cite this article as: Peñuelas O, et al. Desenlace de los enfermos traqueotomizados después de la reintubación. Med Intensiva. 2012. http://dx.doi.org/10.1016/j.medin.2012.03.013.
Study presented by Óscar Peñuelas in June 2010 as an oral communication at the XLV National Congress of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC).