Temporary pacemakers are commonly used in emergency situations in which bradyarrhythmia causes clinical and hemodynamic instability. The electrocatheters most often used in temporary pacing are passive fixation electrodes, which pose a high risk of dislocation. Different venous accesses have been used for temporary transvenous pacemaker (TTP) placement—each with its own complications. Access via the subclavian vein and the internal jugular vein are the most frequently used options, though they are associated to complications such as pneumothorax, discomfort, pain and dislocation of the electrode. Consequently, in our Unit, and in order to preserve an adequate venous access for permanent cardiac pacing, when temporary pacing is required, all of our medical staff use an externalized active fixation electrocatheter implanted via the femoral route.
To assess the clinical outcomes of this temporary electrostimulation modality, we conducted a retrospective review of the patients admitted to our Unit and requiring TTP placement between October 2018 and January 2020. Only those patients receiving a temporary pacemaker with active fixation electrodes (TPAF) via the femoral route were included in the analysis. The patient demographic data were recorded, along with the complications, duration of temporary pacing, the type of permanent device implanted, stay in the Unit, hospital stay and mortality—both in hospital and after 6 months of follow-up in the pacing clinic dependent upon the Unit.
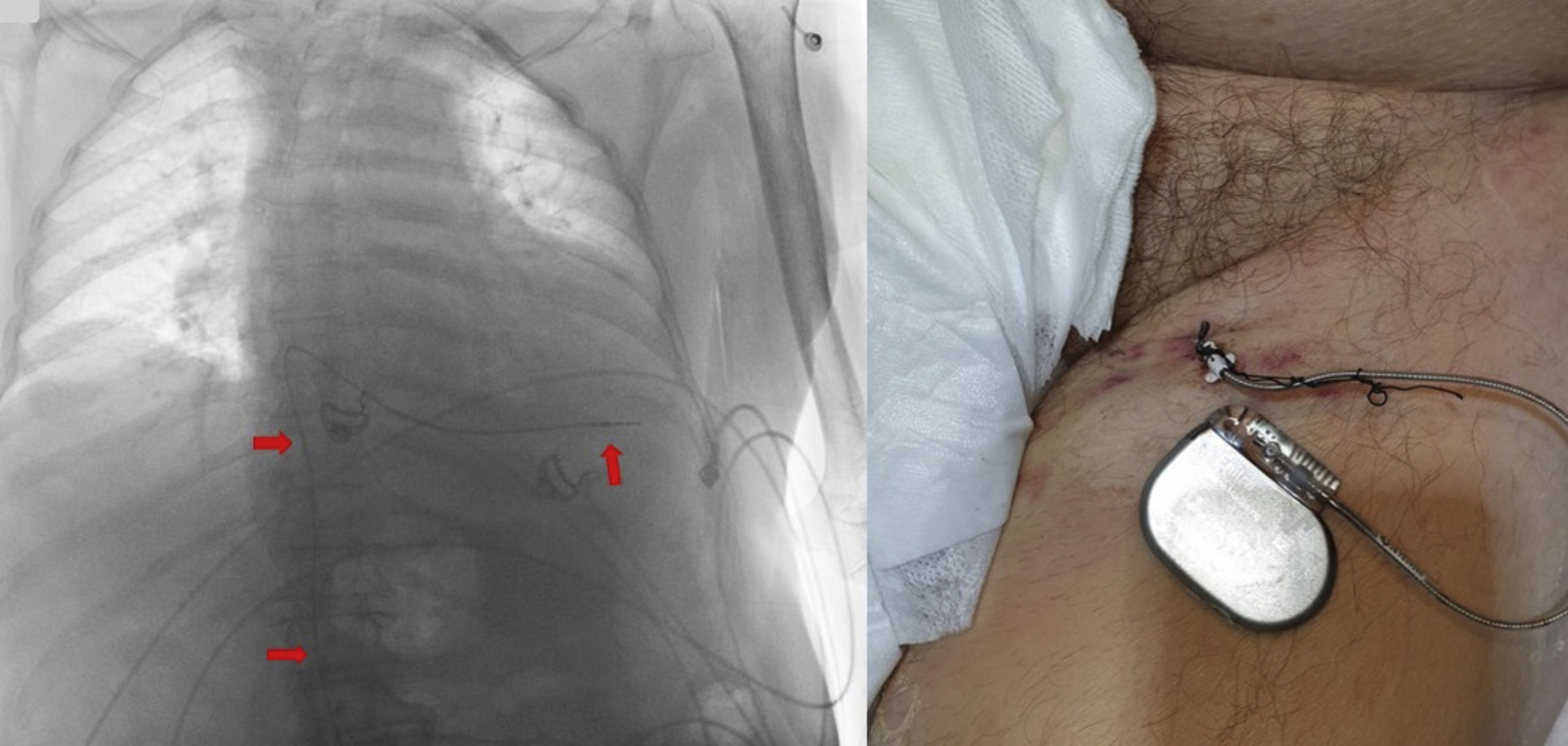
In all cases we used an 85 cm bipolar electrocatheter inserted through a 7F peel-away introducer and advanced under fluoroscopic guidance to the right ventricle. Pacing thresholds of under 1V were considered acceptable. The electrode was affixed to the skin with non-reabsorbable sutures and was connected to a VVI pulse generator VVI (pool of sterilized reusable generators), with a programmed frequency of 60–70 bpm until placement of the definitive device (Fig. 1). All patients remained in the Unit until placement of the definitive device, with allowing of the sitting position.
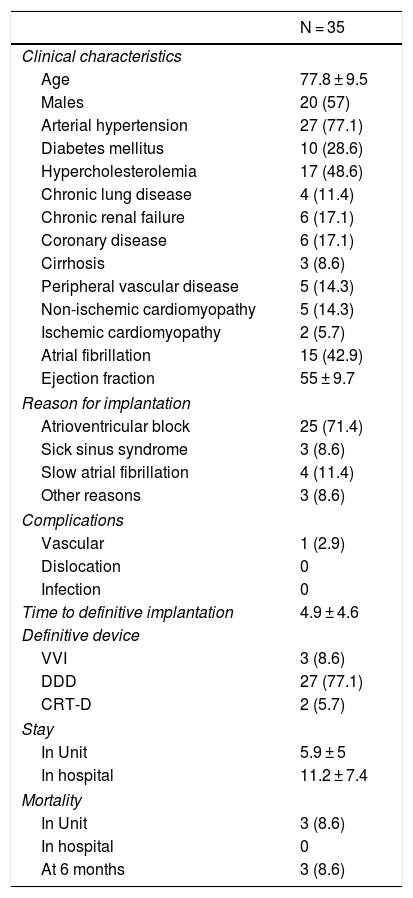
A total of 35 patients were analyzed. Their clinical characteristics, reason for implantation, complications, time to definitive placement, stay in the Unit and hospital stay and survival are reported in Table 1. Continuous variables are reported as the mean ± standard deviation (SD), and dichotomic variables as numbers and percentages. Time is expressed in days.
Patient clinical characteristics, reason for implantation, complications, time to definitive placement, stay in the Unit and hospital stay and survival.
| N = 35 | |
|---|---|
| Clinical characteristics | |
| Age | 77.8 ± 9.5 |
| Males | 20 (57) |
| Arterial hypertension | 27 (77.1) |
| Diabetes mellitus | 10 (28.6) |
| Hypercholesterolemia | 17 (48.6) |
| Chronic lung disease | 4 (11.4) |
| Chronic renal failure | 6 (17.1) |
| Coronary disease | 6 (17.1) |
| Cirrhosis | 3 (8.6) |
| Peripheral vascular disease | 5 (14.3) |
| Non-ischemic cardiomyopathy | 5 (14.3) |
| Ischemic cardiomyopathy | 2 (5.7) |
| Atrial fibrillation | 15 (42.9) |
| Ejection fraction | 55 ± 9.7 |
| Reason for implantation | |
| Atrioventricular block | 25 (71.4) |
| Sick sinus syndrome | 3 (8.6) |
| Slow atrial fibrillation | 4 (11.4) |
| Other reasons | 3 (8.6) |
| Complications | |
| Vascular | 1 (2.9) |
| Dislocation | 0 |
| Infection | 0 |
| Time to definitive implantation | 4.9 ± 4.6 |
| Definitive device | |
| VVI | 3 (8.6) |
| DDD | 27 (77.1) |
| CRT-D | 2 (5.7) |
| Stay | |
| In Unit | 5.9 ± 5 |
| In hospital | 11.2 ± 7.4 |
| Mortality | |
| In Unit | 3 (8.6) |
| In hospital | 0 |
| At 6 months | 3 (8.6) |
Data reported as n (%) or mean ± standard deviation.
None of the positioned electrocatheters presented dislocation, though one of them had to be removed due to bacteremia secondary to urinary infection. The only recorded complication directly related to the implant was a femoral artery pseudoaneurysm that was resolved through percutaneous intervention. Of the three deaths recorded in the Unit, two corresponded to patients with cardiogenic shock upon admission, while the third patient was 86 years old, with multiple disease conditions, and developed pneumonia with secondary septic shock. There were no perforations in our series.
The active fixation electrode offers greater stability than the electrodes traditionally used for temporary cardiac pacing. The most common complication associated with the use of TTP is dysfunction resulting from dislocation of the electrode. The reported incidence of this problem is 10%–60%, and is higher when passive fixation electrocatheters are used.1 To our knowledge, this is the only series to date in the international literature on the use of temporary pacemakers with active fixation electrodes (TPAF) via the femoral route—its most important finding being the absence of dysfunction due to dislocation of the electrocatheter. A recent literature review on the use of TPAF recorded a dislocation rate of 1.7%, though in all of these cases the venous accesses used were the subclavian vein or the internal jugular vein.1 In a study published in 2020 and involving 158 patients subjected to TPAF implantation via the jugular or the subclavian route for temporary pacing due to withdrawal of the permanent device because of infection, Cipriano et al. recorded a temporary electrocatheter dislocation rate of 5.1%.2 though in this study the patients were allowed to walk around.
The only TTP complication recorded in our series (a femoral artery pseudoaneurysm) was related to the venous access procedure, and resulted in a slight prolongation of hospital stay. Likewise, none of the three recorded deaths could be attributed to complications inherent to TTP implantation, and were rather associated to the patient comorbidities.
Some authors have related TTP placement via the femoral route to an increased incidence of deep venous thrombosis and pulmonary thromboembolism,3 though in our series there were no cases of thrombosis either during hospital stay or during the 6 months of follow-up. This route has also been associated to an increase in infections. However, in our series no infections were documented during either hospital stay or the 6-month follow-up period. This fact could be attributable to the correct observation of strict hygiene and to the fact that the duration of TPAF was short (4.9 ± 4.6 days).
The use of TPAF has been related to an increase in cost, because the active fixation electrocatheter is more expensive.4 However, this is compensated by a lower incidence of complications compared with passive fixation electrocatheters,5 mainly in the form of electrode dislocation—which in the case of traditional TTP sometimes makes it necessary to use different electrodes—and the risk of perforation associated to repeated manipulation. Likewise, since the pulse generators are reusable, the overall cost of the procedure is not incremented. The presentation of this technique therefore highlights the safety for the patient of carrying an electrode more stable than the traditional electrodes, avoiding the risk of dislocations. Since the number of TTP procedures in our Unit is low due to the short time interval to definitive pacemaker implantation, TPAF placement via the femoral route is fundamentally used in situations in wait of resolution of the cause of bradycardia (intoxications, myocardial necrosis or myocarditis) or in wait of a full echocardiographic study (performed in the Unit) to determine the type of definitive device (traditional generator, resynchronization therapy and/or defibrillator), or because the patient has reported to the Unit on non-working days.
In conclusion, and considering the limited size of our study sample, the results obtained suggest that TPAF via the femoral route is a safe temporary pacing strategy. Nevertheless, further studies of a multicenter nature are needed, involving larger patient samples, in which the results are also compared against those of passive fixation electrodes—thereby reinforcing the importance of the Department of Intensive Care Medicine in relation to cardiac pacing in this country.
Please cite this article as: Keituqwa Yáñez I, Navarro Martínez J, García Valiente M, Rodríguez González FJ, Nicolás Franco S. Resultados del uso de marcapasos transitorios con electrodos de fijación activa implantados por vía femoral. Med Intensiva. 2022;46:96–98.