The way in which outbreaks affect countries depends on multiple factors and its impact is difficult to foresee.1 However, the numbers of infected people and casualties are evidence that despite attempts to plan, the global healthcare systems remain unprepared.2 The intensity of staffing and the sophisticated training required for the care of patients with viral infections during pandemics, result in the fact that a relatively small number of patients can easily overwhelm healthcare systems.3
The identification of variables related to worse outcomes is key for triaging and adapting the intensity of care that each patient requires, allowing effective strategic planning and better administration of human and material resources. Moreover, the need for a sensitive and predictive model is mandatory to avoid a delayed recognition of severely ill patients or those at risk of presenting further complications.4
During the early phase of COVID-19 pandemic Liao et al. propose an early warning score based on an adapted version of the National Early Warning Score 2 (NEWS-2) adding age as a variable, based on actual evidence of being an independent risk factor for survival.5
Considering the high number of patients admitted with COVID-19, a specific early warning system (EWS) including laboratory test results, clinical features and radiological findings, could improve the detection of high-risk patients for optimization and a better management of hospital resources, mainly relevant in low-income countries.6,7
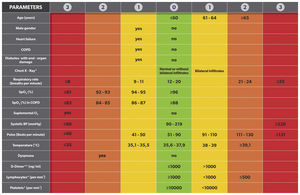
COVID-19 Severity Index was developed as a triage tool based on the NEWS-2 score,8 that could rapidly and reliably be used by frontline healthcare personnel to identify high-risk patients. For the construction of this index, a narrative review was conducted to generate a list of possible predictors based on clinical signs and symptoms, comorbidities, laboratory and radiographic findings. After initial identification of 44 predictive variables of worse outcome, they were subjected to a 2-round Delphi process with participants from different countries around the world, diverse backgrounds and multiple areas of expertise.
At the stage of analysis, each answer was given a number between 0 and 3 (high (3), moderate (2), minimal (1), not applicable (0)) based on the strength of the answer.9 The number for each domain was tabulated to calculate a weighted effect (WE) to help determine the selection threshold. The WE was calculated following the formula below:
WE was calculated for each variable and each expert's opinion. The sum of the WE’s for a given variable was ranked for further selection of those with the greatest value.
Afterwards, a threshold was chosen based on a desired number of predictors. Then, variables with WE above the threshold were included in a final set of predictor variables. Those variables below the threshold were carefully reviewed by the research team and discharged or included in Round 2 for re-evaluation depending on the value obtained. Any additional variables proposed by participants were also evaluated in Round 2.
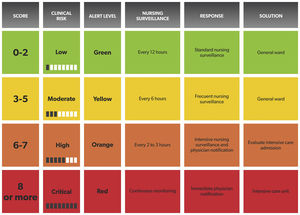
A final set of selected variables was combined with a modified NEWS-2 score to generate the COVID-19 Severity Index (Fig. 1). Patients were divided into four risk categories based on their score (Fig. 2).
This score was studied to test its potential predictive capacity for ICU transfer 24 and 48 h elapse of time. A group of 220 patients with confirmed infection were evaluated; 19 of which were unexpectedly transferred to the ICU; 17 were transferred during the first three days, one at day 5 and another one at day 6 from admission.
A comparison between COVID-19 Severity Index, NEWS score adapted by Liao et al.5 and NEWS-2 score was made. All three EWS were measured on the first, second and third day after hospital admission. For those who were initially admitted into general wards and were later transferred to the ICU, the score was retrospectively applied for the 24, 48 and 72 h prior to the ICU admission, with the intention to identify whether if there were parameters that could predict the need of a more intensive monitoring or not.
A comparative analysis of the area under the curve (AUC) for the different scores evidenced a better capacity of the COVID-19 Severity Index to predict the need for ICU admission. When applied 24 h prior to transferal, the AU-ROC for our score was 0.94 vs. 0.88 for the modified NEWS score developed by Liao et al., and 0.80 for NEWS-2 (Fig. 2). When applied 48 h prior to ICU admission, the AU-ROC for COVID-19 Severity Index was 0.88, 0.84 for the modified NEWS and 0.62 for NEWS-2.
The digital medical record was electronically set for an automatic calculation and constant update of the COVID-19 Severity Index as soon as the latest laboratory results and vital signs were recorded. This provided real-time information for deciding the most suitable area of care for each patient.10
Specifically designed for the current COVID-19 pandemic, COVID-19 Severity Index serves as a reliable tool for strategic planning, organization and administration of resources by easily distinguishing hospitalized patients with higher risk and need of a prompt ICU transfer.
DeclarationsEthics approvalThis project has been approved by the Ethics Committee for Research Protocols at Hospital Italiano de Buenos Aires (Cod. 1290).
Consent of publicationNot applicable.
Data availability statementAll relevant data are within the manuscript and its supporting.
FundingAuthors received no specific funding for this work.
Conflict of interestsAuthors have declared that no competing interests exist.
We would like to thank the experts Marcos Marino, Sergio Giannasi, Fernando Vazquez, Martin Hunter, Leonardo Uranga, Chung Kyu, José Dianti, Manuel Tisminetzky, Bruno Ferreyro, Federico Angriman, Eduardo De Vito, Silvia Quadrelli, Alejandro Chirino, Eduardo Tobar and Pablo Gastaldi for their enthusiastic contribution and suggestions in the modified Delphi process. We would like to thank Lisandro Ziperovich (Zipper Art) for the artwork of this study and Maria de los Angeles Magaz for draft editing. Finally we would like to thank Valeria Burgos, Pablo delgado, Marina Bezzati, Mailen Oubina, Jorge Sinner, Marcelo Risk and Eduardo San Roman for their support and guidance.
Please cite this article as: Huespe I, Carboni Bisso I, Di Stefano S, Terrasa S, Gemelli NA, Las Heras M. COVID-19 Severity Index: A predictive score for hospitalized patients. Med Intensiva. 2022;46:98–101.