To identify factors related to mortality in adult trauma patients, analyzing the clinical, epidemiological and therapeutic characteristics at the pre-hospital levels, in the Emergency Care Department and in Intensive Care.
DesignA retrospective, longitudinal descriptive study was carried out. Statistical analysis was performed using SPSS, MultBiplot and data mining methodology.
SettingAdult multiple trauma patients admitted to the Salamanca Hospital Complex (Spain) from 2006 to 2011.
Main variables of interestDemographic variables, clinical, therapeutic and analytical data from the injury site to ICU admission. Evolution from ICU admission to hospital discharge.
ResultsA total of 497 patients with a median age of 45.5 years were included. Males predominated (76.7%). The main causes of injury were traffic accidents (56.1%), precipitation (18.4%) and falls (11%). The factors with the strongest association to increased mortality risk (p<0.05) were age>65 years (OR 3.15), head injuries (OR 3.1), pupillary abnormalities (OR 113.88), level of consciousness according to the Glasgow Coma Scale≤8 (OR 12.97), and serum lactate levels>4mmol/L (OR 9.7).
ConclusionsThe main risk factors identified in relation to the prognosis of trauma patients are referred to the presence of head injuries. Less widely known statistical techniques such as data mining or MultBiplot also underscore the importance of other factors such as lactate concentration. Trauma registries help assess the healthcare provided, with a view to adopt measures for improvement.
Identificar los factores relacionados con la mortalidad de los pacientes adultos politraumatizados, analizar las características clínicas, epidemiológicas y terapéuticas en los niveles prehospitalario, Servicio de Urgencias y Cuidados Intensivos.
DiseñoEstudio retrospectivo, longitudinal y descriptivo. Análisis estadístico a través del programa SPSS, MultBiplot y la metodología de minería de datos.
ÁmbitoPacientes adultos politraumatizados ingresados en el Complejo Hospitalario de Salamanca entre los años 2006 y 2011.
Variables de interés principalesVariables demográficas, clínicas, terapéuticas y analíticas desde el lugar del accidente hasta el ingreso en la UCI. Variables evolutivas durante el ingreso en la UCI y hasta el alta hospitalaria.
ResultadosSe incluyó a 497 pacientes, con una mediana de edad 45,5 años. Predominio de varones (76,7%). La causa principal del traumatismo fueron los accidentes de tráfico (56,1%), precipitaciones (18,4%) y caídas (11%). Los factores con mayor asociación a un incremento del riesgo de mortalidad (p<0,05) fueron la edad > 65 años (OR 3,15), el traumatismo craneoencefálico (OR 3,1), las alteraciones pupilares (OR 113,88), el nivel de consciencia según la escala de Glasgow ≤ 8 (OR 12,97) y las cifras de lactato > 4mmol/L (OR 9,7).
ConclusionesLos principales factores de riesgo identificados en relación con el pronóstico de los pacientes politraumatizados son los relacionados con la presencia de traumatismo craneoencefálico. Mediante la utilización de distintas técnicas estadísticas menos conocidas como la minería de datos o el MultBiplot también se destaca la importancia de otros factores como el lactato. Los registros de traumatismos ayudan a conocer la asistencia sanitaria realizada para poder establecer medidas de mejora.
Severe trauma is regarded as one of the disorders with the greatest healthcare and economic impact in society today. Worldwide, it is the leading cause of mortality in young adults, and involves the highest incidence of potential life years lost. According to the World Health Organization (WHO) in its 2011 statistical report on data referred to 2008,1 the mortality rate associated to trauma worldwide is 78 deaths/100,000 inhabitants, ranging between 107 deaths/100,000 inhabitants in Africa and 63 deaths/100,000 inhabitants in Europe. The main causes of trauma are traffic and work accidents, while other causes comprise falls, sports accidents, etc.
The management of patients with severe trauma starts at the site of injury, where the pre-hospital healthcare services play a key role. This initial patient care has been protocolized through a series of recommendations that are regularly updated on the basis of scientific evidence–the reference of which is found in the methodology proposed by the Prehospital Trauma Life Support program, which prioritizes treatment of the most life-threatening injuries at the trauma site, and the Advanced Trauma Life Support (ATLS) program, once the patient reaches the reference hospital.2 Following the pre-hospital phase, initial in-hospital care3 is mainly the responsibility of the Emergency Care Departments and Intensive Care Units (ICUs). Early identification of the factors related to severity and the adoption of appropriate management measures has a clear impact on the patient prognosis and possible sequelae.
The present study describes the management of severe trauma and polytraumatized patients at the three healthcare levels in the province of Salamanca (Spain). A description is provided of the different variables that influence the final outcome starting from the actual site of injury, whether epidemiological or related to patient care, including clinical, laboratory test, diagnostic and therapeutic parameters.
Patients and methodsA retrospective descriptive study was made of the polytraumatized patients admitted to the ICU of Salamanca Hospital Complex during the years 2006–2011. The data considered to be most relevant within each link of the patient care chain were collected by reviewing the patient case histories:
- -
Epidemiological variables: patient age, gender, type of accident (traffic, accidental fall <50cm or >50cm, sports, assault [knife or gun wounds], injuries caused by cattle, and others), origin (pre-hospital or transferred from another hospital–fundamentally Avila or Zamora), and personal history.
- -
Pre-hospital and in-hospital emergency care clinical, diagnostic and therapeutic variables:
- •
First care, form of transport and time to arrival in hospital: basic life support, advanced life support (ALS), medicalized helicopter, others.
- •
Clinical particulars: blood pressure (BP), heart rate, oxygen saturation, respiratory frequency, initial Glasgow Coma Scale (GCS) score, with the identification of verbal, ocular and motor response and pupillary alterations (anisocoria or non-reactive mydriasis).
- •
Treatment: oxygen therapy, advanced airway management (orotracheal intubation, laryngeal mask, Fastrach® or others), venous access, chest drain, need for vasoactive drugs, need for cardiopulmonary resuscitation, and fluid therapy.
- •
Diagnostic measures and timing: plain X-rays of the chest and pelvis, ECO-FAST, computed tomography (brain, cervical, thoracic or abdominopelvic), laboratory tests and blood lactate measurements.
- •
- -
Variables in the ICU:
- •
Time to admission to the ICU from arrival in hospital, and origin (Emergency Care, Radiology, operating room, other hospital, or others).
- •
Clinical and laboratory test data upon admission.
- •
Evolutive data after 6 and 24h: water balance, adrenalin dose (if required), transfusion of blood products and coagulation factors, lactate, and PaO2/FiO2 ratio.
- •
Complications:
- ∘
Renal failure.
- ∘
Infections: ventilator-associated pneumonia (VAP), catheter-related infections, urinary infections, central nervous system (CNS) infections, abdominal infections, or others.
- ∘
- •
Variables related to mechanical ventilation: days of mechanical ventilation, performance of tracheotomy in the ICU (percutaneous or surgical), transfer to ward with tracheotomy, or decannulation in the ICU.
- •
- -
Evolutive parameters:
- •
Days of stay in the ICU and in hospital.
- •
Death in the ICU or in the hospital ward.
- •
Severity scores: Acute Physiology and Chronic Health Evaluation–II (APACHE-II), Injury Severity Score (ISS) and Extended Glasgow Outcome Scale (GOS-E) at hospital discharge, and Glasgow Coma Scale (GCS) at discharge from the ICU and at hospital discharge.
- •
- -
Diagnostic variables: types of trauma and acute management:
- •
Traumatic brain injury (TBI): surgical treatment (evacuating surgery, decompressive craniectomy, external ventricular drainage), intracranial pressure (ICP) monitoring with attention to initial ICP and maximum measured ICP, medical treatment (hyperosmolar therapy, barbiturate coma with recording of its start and duration), and the Marshall classification.
- •
Other traumatisms: spine and spinal cord injury, and facial, thoracic, abdominal, pelvic, orthopedic and genitourinary trauma.
- •
A Microsoft Access database was created for posterior statistical analysis using the SPSS statistical package, MultBiplot and data mining methodology. Multivariate binary logistic regression analysis was performed, calculating the odds ratio (OR) of the factors considered pertinent in relation to mortality, adjusted for age and gender, with the corresponding 95% confidence intervals (95%CI). Likewise, data mining was used, applying different algorithms with the purpose of selecting the most influential parameters in relation to mortality, along with other algorithms for the prediction of outcomes referred to death, and the development of a series of decision trees.
Those patients in whom correct review of the case history was not possible due to problems locating the data or because of missing relevant information (e.g., laboratory test results or hospital admission and discharge reports) were excluded from the study.
ResultsDuring the study period we selected a total of 497 out of 562 possible patients diagnosed with severe trauma or polytraumatism. The high percentage of excluded patients (11.2%) was fundamentally due to the fact that Salamanca Hospital Complex is the Neurosurgery reference center for the provinces of Avila and Zamora, and the Chest Surgery reference center for Avila, Zamora and Leon (20% of the patients in the study came from other provinces). Consequently, in many cases there were difficulties in obtaining the required pre-hospital and/or hospital emergency care information, and those patients for whom the data could not be obtained from reviewing the case histories were excluded from the study.
The mean pre-hospital care time among the 359 patients for whom this parameter could be recorded was 62.36min, with a standard deviation of 31.1min (median 60min). Due to the peculiarities of the healthcare infrastructure of the province of Salamanca, two well differentiated groups can be identified regarding the care times: the first group corresponding to the city of Salamanca and the second to ALS of Bejar and Ciudad Rodrigo, together with the helicopter of the Matacan airbase. The difference in mortality rate between the two groups was 3.6% (13% vs 16.5%), though this difference was not statistically significant in terms of an increased mortality risk in those patients for whom the time of transfer to the hospital center was longer: OR 1.399 (0.671–2.892); p=0.778.
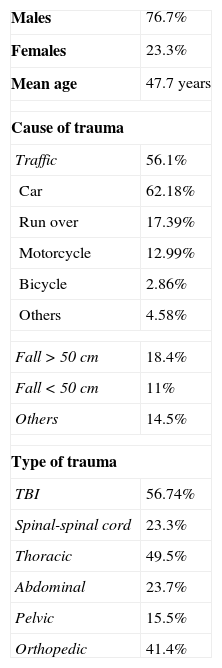
The epidemiological characteristics, causes of trauma and the types of traumatisms are reported in Table 1. The high percentage of pedestrians run over in the traffic accident group is significant; indeed, in the population over 65 years of age, this was found to be the main type of traffic accident (48% of the cases). A patient age of over 65 years was associated to a three-fold increase in mortality risk in our series (OR 3.15 [1.781–5.593]); p<0.001. With regard to the different types of traumatisms, TBI was the most frequent injury among those patients requiring admission to the ICU, and was associated to a significant three-fold higher mortality risk (OR 3.095 [1.570–6.099]). Forty-four percent of the patients presented an ISS>25 points, this being associated to a mortality risk 28 times higher than in patients with ISS<25 points. The overall mortality rate among the patients in our study was 14.5%.
Epidemiological characteristics, and causes and types of trauma.
| Males | 76.7% |
| Females | 23.3% |
| Mean age | 47.7 years |
| Cause of trauma | |
| Traffic | 56.1% |
| Car | 62.18% |
| Run over | 17.39% |
| Motorcycle | 12.99% |
| Bicycle | 2.86% |
| Others | 4.58% |
| Fall>50cm | 18.4% |
| Fall<50cm | 11% |
| Others | 14.5% |
| Type of trauma | |
| TBI | 56.74% |
| Spinal-spinal cord | 23.3% |
| Thoracic | 49.5% |
| Abdominal | 23.7% |
| Pelvic | 15.5% |
| Orthopedic | 41.4% |
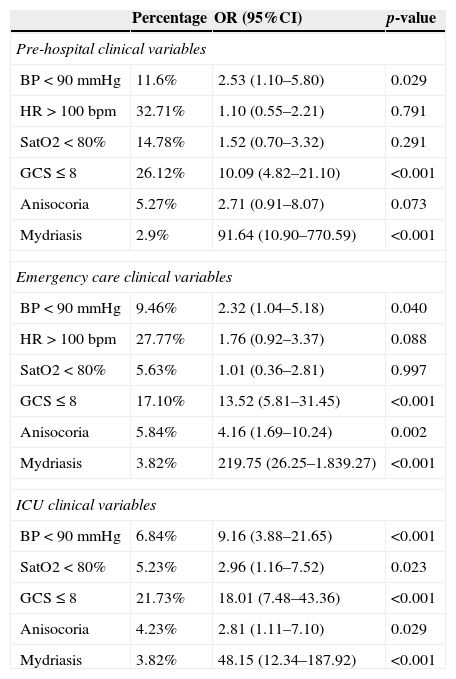
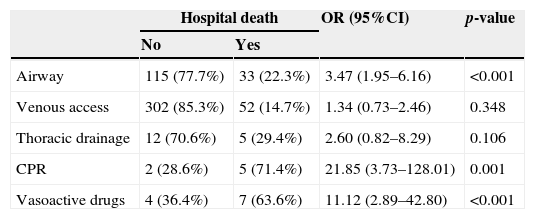
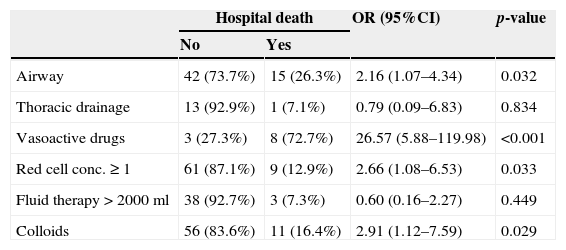
Table 2 shows the clinical variables studied in each link of the patient care chain and their relation to increased mortality risk according to the calculated odds ratio. At all three levels, neurological impairment as assessed by the GCS, pupillary alterations and hypotension was related to increased mortality risk. On jointly considering the pre-hospital, emergency care and ICU data, a GCS≤8 was found to be associated to a 12.97-fold increase in mortality risk (OR 12.969 [3.518–47.812]). Regarding the therapeutic techniques used by the pre-hospital and emergency care services (Tables 3 and 4), increased in-hospital mortality risk was seen to be associated to a need for vasoactive drugs and lung isolation maneuvers at both care levels. It should be mentioned that 4% of the patients with GCS≤8 reached the Emergency Care Department without lung isolation, though no statistically significant association to increased mortality was observed.
Binary logistic regression analysis of the most significant clinical variables at pre-hospital level, in emergency care, and in the ICU, in relation to hospital mortality.
| Percentage | OR (95%CI) | p-value | |
|---|---|---|---|
| Pre-hospital clinical variables | |||
| BP<90mmHg | 11.6% | 2.53 (1.10–5.80) | 0.029 |
| HR>100bpm | 32.71% | 1.10 (0.55–2.21) | 0.791 |
| SatO2<80% | 14.78% | 1.52 (0.70–3.32) | 0.291 |
| GCS≤8 | 26.12% | 10.09 (4.82–21.10) | <0.001 |
| Anisocoria | 5.27% | 2.71 (0.91–8.07) | 0.073 |
| Mydriasis | 2.9% | 91.64 (10.90–770.59) | <0.001 |
| Emergency care clinical variables | |||
| BP<90mmHg | 9.46% | 2.32 (1.04–5.18) | 0.040 |
| HR>100bpm | 27.77% | 1.76 (0.92–3.37) | 0.088 |
| SatO2<80% | 5.63% | 1.01 (0.36–2.81) | 0.997 |
| GCS≤8 | 17.10% | 13.52 (5.81–31.45) | <0.001 |
| Anisocoria | 5.84% | 4.16 (1.69–10.24) | 0.002 |
| Mydriasis | 3.82% | 219.75 (26.25–1.839.27) | <0.001 |
| ICU clinical variables | |||
| BP<90mmHg | 6.84% | 9.16 (3.88–21.65) | <0.001 |
| SatO2<80% | 5.23% | 2.96 (1.16–7.52) | 0.023 |
| GCS≤8 | 21.73% | 18.01 (7.48–43.36) | <0.001 |
| Anisocoria | 4.23% | 2.81 (1.11–7.10) | 0.029 |
| Mydriasis | 3.82% | 48.15 (12.34–187.92) | <0.001 |
Multivariate binary logistic regression analysis of the pre-hospital techniques in relation to hospital mortality, adjusted for age and gender.
| Hospital death | OR (95%CI) | p-value | ||
|---|---|---|---|---|
| No | Yes | |||
| Airway | 115 (77.7%) | 33 (22.3%) | 3.47 (1.95–6.16) | <0.001 |
| Venous access | 302 (85.3%) | 52 (14.7%) | 1.34 (0.73–2.46) | 0.348 |
| Thoracic drainage | 12 (70.6%) | 5 (29.4%) | 2.60 (0.82–8.29) | 0.106 |
| CPR | 2 (28.6%) | 5 (71.4%) | 21.85 (3.73–128.01) | 0.001 |
| Vasoactive drugs | 4 (36.4%) | 7 (63.6%) | 11.12 (2.89–42.80) | <0.001 |
Multivariate binary logistic regression analysis of the therapeutic and fluid therapy measures in emergency care in relation to hospital mortality, adjusted for age and gender.
| Hospital death | OR (95%CI) | p-value | ||
|---|---|---|---|---|
| No | Yes | |||
| Airway | 42 (73.7%) | 15 (26.3%) | 2.16 (1.07–4.34) | 0.032 |
| Thoracic drainage | 13 (92.9%) | 1 (7.1%) | 0.79 (0.09–6.83) | 0.834 |
| Vasoactive drugs | 3 (27.3%) | 8 (72.7%) | 26.57 (5.88–119.98) | <0.001 |
| Red cell conc.≥1 | 61 (87.1%) | 9 (12.9%) | 2.66 (1.08–6.53) | 0.033 |
| Fluid therapy>2000ml | 38 (92.7%) | 3 (7.3%) | 0.60 (0.16–2.27) | 0.449 |
| Colloids | 56 (83.6%) | 11 (16.4%) | 2.91 (1.12–7.59) | 0.029 |
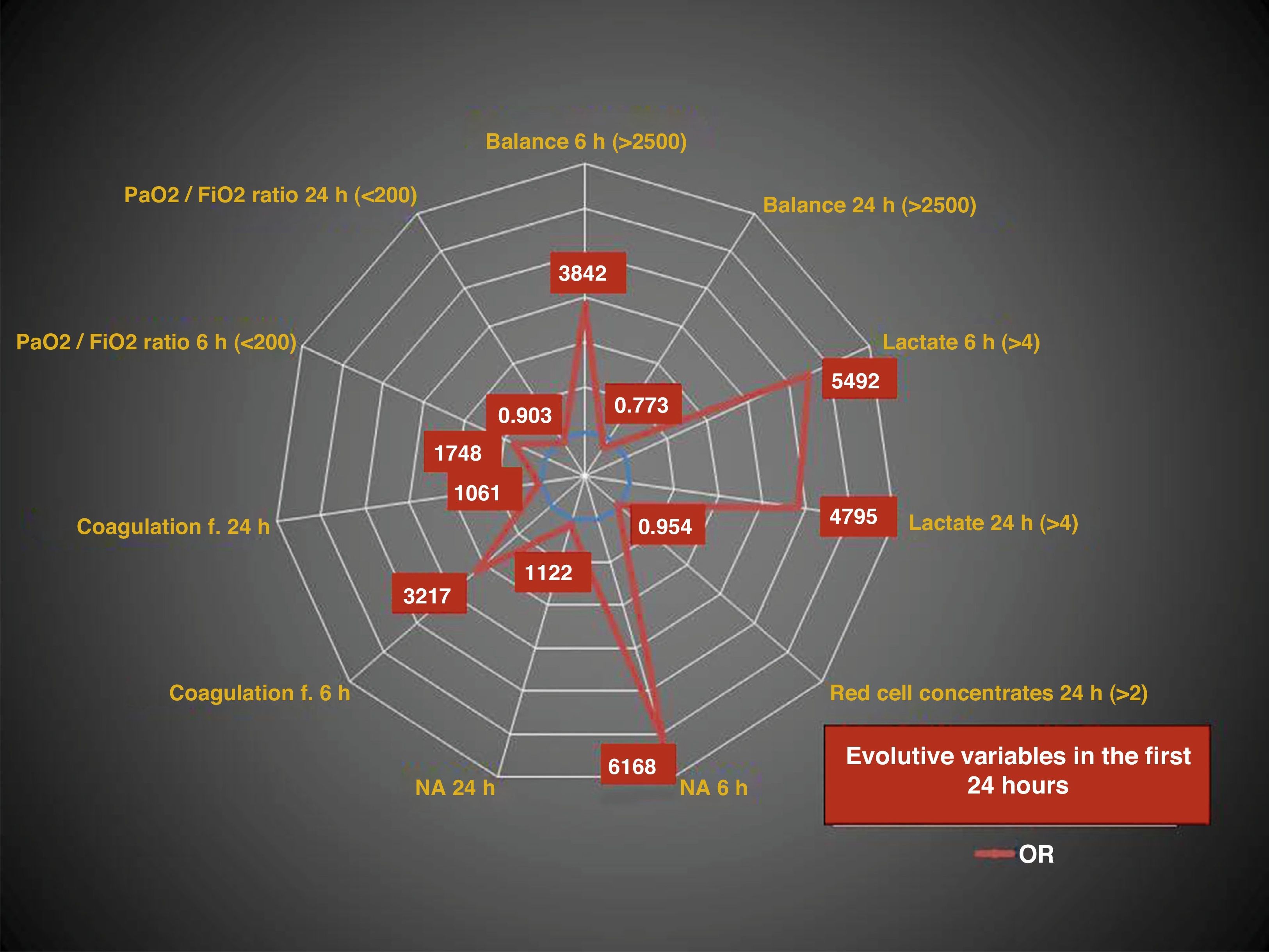
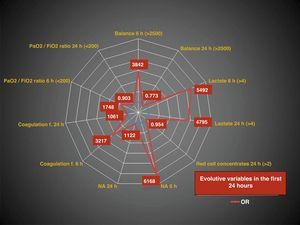
Among the in-hospital laboratory test parameters, elevated lactate concentration was seen to be associated to increased mortality risk, particularly when found to be persistently high (>4mmol/l) over the first 24h of management (Fig. 1). The adoption of measures to ensure normal oxygenation, ventilation and blood pressure values was related to a decreased mortality risk in the period covering pre-hospital to emergency care. This trend was not observed upon admission to the ICU, though many mediating factors could have been involved, such as the time to admission to the ICU, the origin of the patients, the need for surgery before admission to the ICU, etc. The persistence of hypotension upon admission to the ICU was correlated to an almost four-fold higher mortality risk compared with hypotension upon admission to emergency care. The administration of vasoactive drugs in the first 6h of in-hospital care was associated to a more than 6-fold increase in mortality risk (OR 6.168 [2.598–14.645]), and a positive water balance of over 2500ml was associated to a three-fold increase in mortality risk (OR 3.842 [2.020–7.305]). The use of colloids during admission to emergency care implied an almost three-fold increase in mortality risk (OR 2.910 [1.067–8.036]); p=0.029.
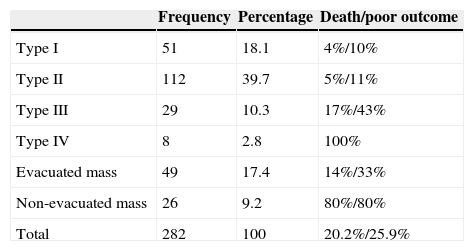
As has been commented, TBI is the most extreme representation of trauma requiring admission to the ICU, and is associated to increased mortality. Of the patients diagnosed with TBI in our study (282 subjects), information referred to the GCS score was available on 275 (97.5%). In this regard, severe TBI (GCS≤8) was more frequent, representing 54.2% of the patients, while moderate TBI (GCS 9–13) accounted for 14.9% and mild TBI (GCS 14–15) represented 30.9%. In relation to the Marshall classification (Table 5), information was available on 97.9% of the patients with TBI–the most frequent lesions corresponding to type ii (39.7%), while the lesions with a poorer prognosis (type iv) and cases involving non-evacuated mass accounted for 2.8% and 9.2%, respectively. Of the patients for whom information regarding the GCS was available, it can be concluded that a decrease in GCS score was associated to a significant 29.3-fold increase in the risk of mortality in the ICU and a 13-fold increase in the risk of mortality in hospital, in patients with GCS≤8 (p<0.001).
Marshall classification of the patients with traumatic brain injury. Description of the patients that died or presented a poor neurological outcome (persistent vegetative state or severe disability) according to the classification, based on the Extended Glasgow Outcome Scale at hospital discharge.
| Frequency | Percentage | Death/poor outcome | |
|---|---|---|---|
| Type I | 51 | 18.1 | 4%/10% |
| Type II | 112 | 39.7 | 5%/11% |
| Type III | 29 | 10.3 | 17%/43% |
| Type IV | 8 | 2.8 | 100% |
| Evacuated mass | 49 | 17.4 | 14%/33% |
| Non-evacuated mass | 26 | 9.2 | 80%/80% |
| Total | 282 | 100 | 20.2%/25.9% |
Regarding the specific monitoring and treatment measures during the stay in the ICU among patients with TBI, data that referred to intracranial pressure (ICP) were available in 88 patients (31.2%), with a mean initial ICP of 23.3mmHg (standard deviation 15.1mmHg) and a mean maximum ICP of 37.6mmHg (standard deviation 32mmHg). If intracranial hypertension is defined as ICP≥20mmHg, then 75% of the monitored patients had intracranial hypertension. In relation to the treatment of intracranial hypertension, all of the patients initially received sedoanalgesia and relaxation, while 50% on some occasion received hyperosmolar treatment in the form of 20% mannitol or 7.5% hypertonic saline solution. When these measures failed to control ICP, 5% of the patients with TBI were subjected to decompressive craniectomy, while 22 patients (7.8%) underwent barbiturate coma induction through the administration of thiopental sodium. The mean time to the induction of barbiturate coma was 38.9h, with a standard deviation of 27.91h and a mean duration of 8.75 days (standard deviation 3.47). External ventricular drainage was only used in two patients (0.7%). Both the initial ICP and a maximum ICP of >30mmHg were associated to increased mortality risk and a poorer neurological outcome – though the results were not statistically significant (p>0.05). In turn, barbiturate coma and decompressive craniectomy were associated to a significantly poorer neurological outcome (p<0.05), but were not correlated to increased mortality risk either in the ICU or in hospital.
Outcome variables and complications in the ICUA total of 334 patients required mechanical ventilation, with a mean duration of 9.27 days. The mortality rate among the patients subjected to mechanical ventilation was 15.9% in the ICU and 19.16% in hospital. Of the total patients, 69 underwent tracheotomy during admission to the ICU (13.9%), with the use of percutaneous tracheotomy in 62 of them (89.9%). Of the tracheotomized patients, 24 were decannulated in the ICU (34.8%), and one patient subsequently died in the ICU and another in the hospital ward. Fourteen percent of the remaining 43 patients (62.3%) who were moved to the hospital ward with the tracheotomy cannula subsequently died.
In relation to the complications of the patients during admission to the ICU, particular mention must be made of infectious processes. Specifically, the most frequent infections were of a respiratory nature, with ventilator-associated pneumonia (VAP) in 19.5% of the cases–mostly of early onset (within the first 5–7 days of admission)–followed by catheter-related infections (3.8%). On considering only TBI, the proportion of VAP was found to increase to 21.5%. The rest of the infections had a lesser incidence and corresponded to urinary infections, postoperative abdominal infections and central nervous system infections.
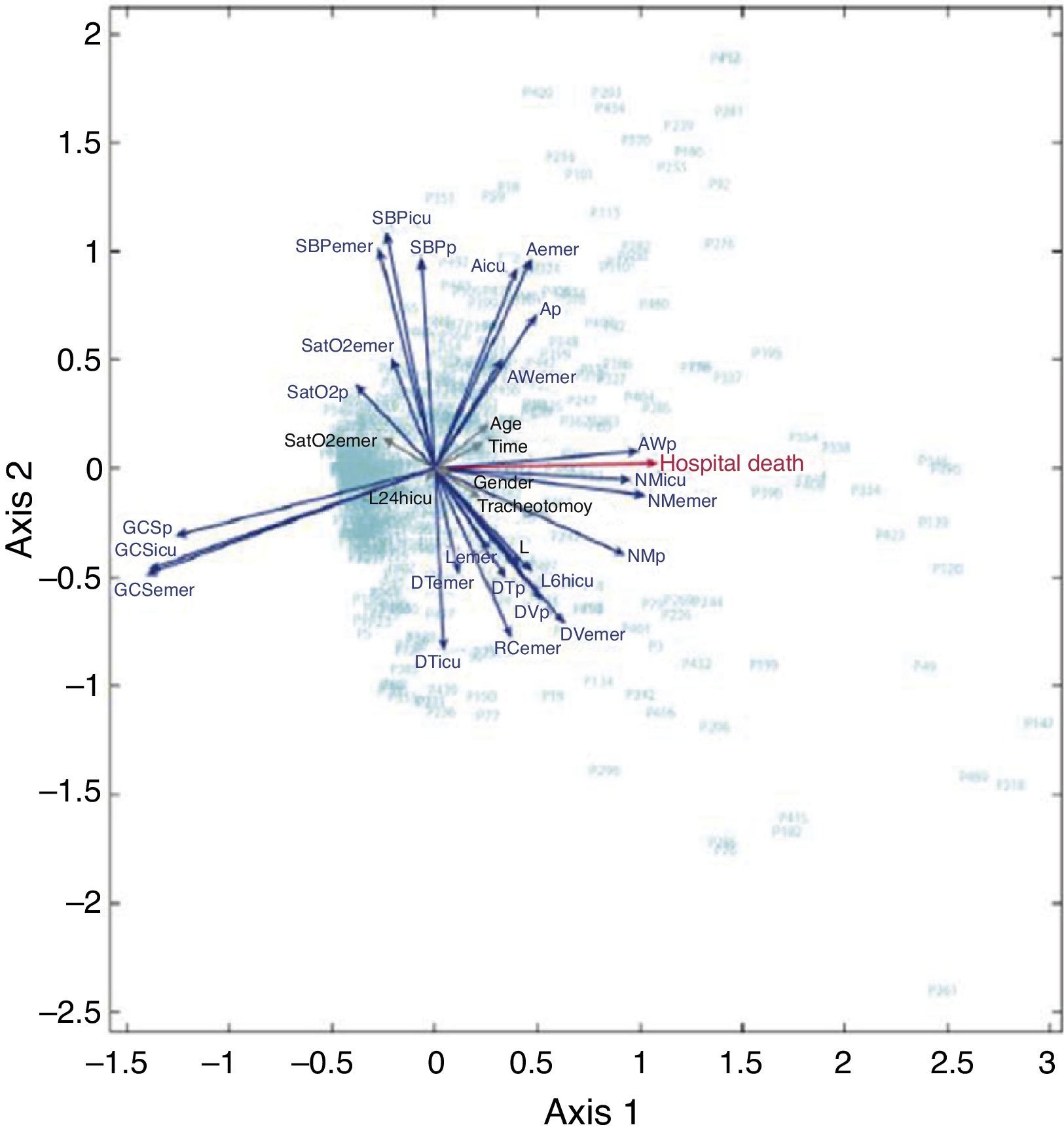
HJ-BiplotThe HJ Biplot statistical analysis using the MultBiplot program4 yielded a graphic representation (Fig. 2) of the different study variables. Through determination of the length and angulation between variables represented in vector form, we can determine the greater or lesser association between variables. On taking death as the reference variable, the vectors with a more acute angulation were seen to correspond to the variables anisocoria and the need for lung isolation by the pre-hospital care service. The GCS was positioned in the plot opposite to death in the ICU (forming an angle of 180° with death), i.e., the GCS score was inversely related to death (lesser scores being associated to increased mortality). In turn, the persistence over time of lactate levels of >4mmol/l was associated to mortality, as represented by a more acute angulation of lactate >4mmol/l after 6h of admission to the ICU (L6hicu) versus lactate upon admission to the ICU (L) or lactate concentration in emergency care (Lemer). Some variables appear coded in less intense color, indicating that they are more poorly represented in the plot, though tending to be associated to mortality in the ICU, such as patient age, pre-hospital care time, and the need for tracheotomy.
HJ-Biplot multivariate analysis of the variables related to in-hospital mortality. Ap: pre-hospital anisocoria; Aicu: anisocoria in ICU; Aemer: anisocoria in emergency care; RCemer: red cell concentrates in emergency care; DTp: pre-hospital thoracic drainage; DTicu: thoracic drainage in ICU; DTemer: thoracic drainage in emergency care; DVp: pre-hospital vasoactive drugs; DVemer: vasoactive drugs in emergency care; GCSp: pre-hospital GCS; GCSemer: GCS in emergency care; GCSicu: GCS in ICU; L: lactate upon admission to ICU; L24hicu: lactate after 24h in ICU; L6hicu: lactate after 6h in ICU; Lemer: lactate in emergency care; NMp: pre-hospital non-reactive mydriasis; NMicu: non-reactive mydriasis in ICU; NMemer: non-reactive mydriasis in emergency care; SatO2p: pre-hospital SatO2; SatO2emer: SatO2 in emergency care; SBPp: pre-hospital systolic BP; SBPicu: systolic BP in ICU; SBPemer: systolic BP in emergency care; Time: time to arrival in hospital; AWp: pre-hospital airway; AWemer: airway in emergency care.
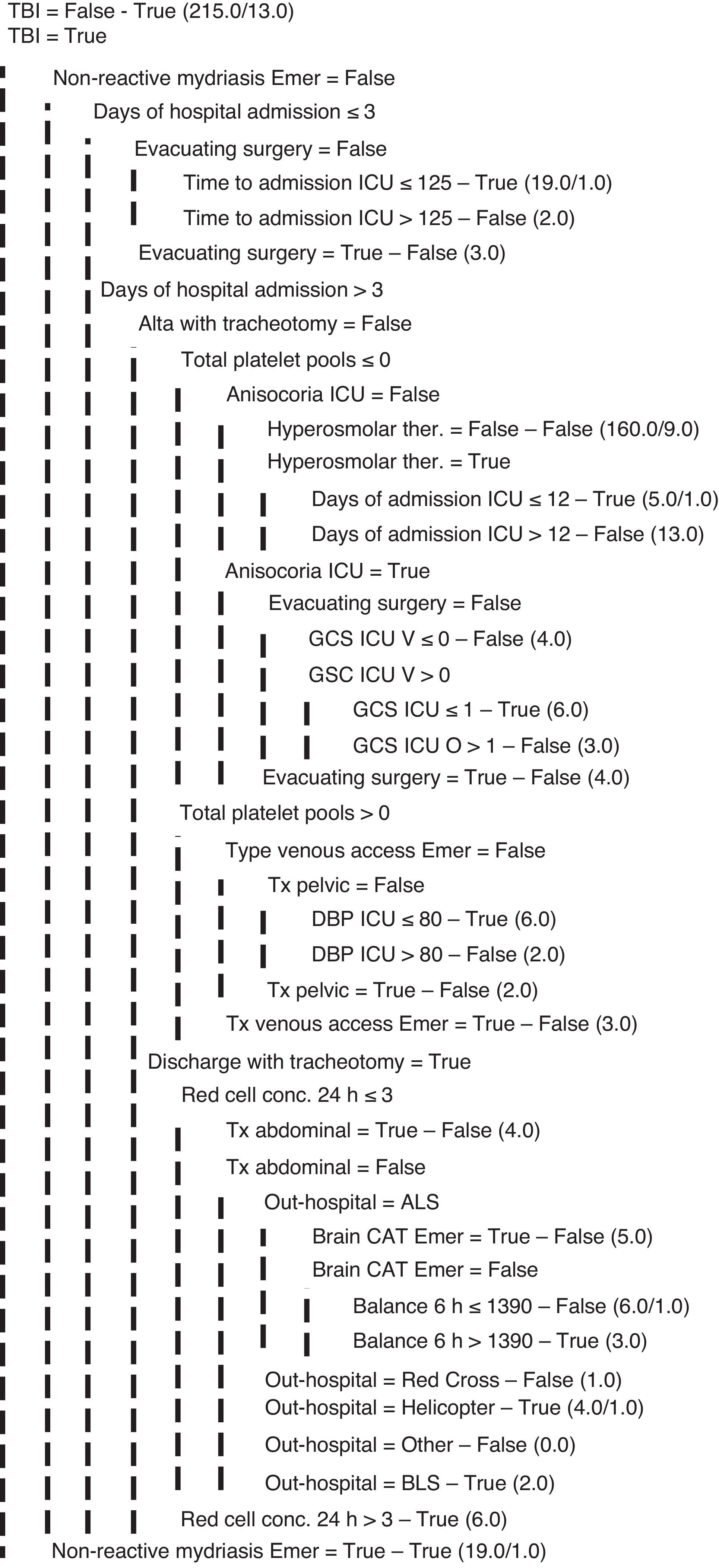
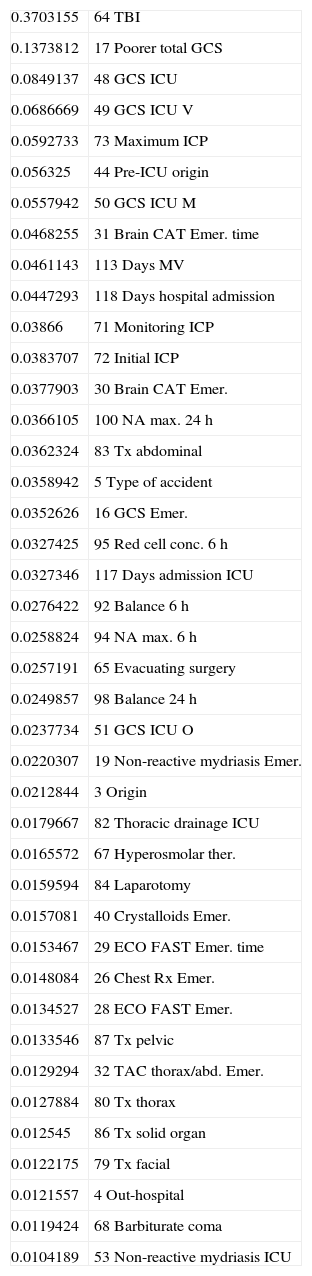
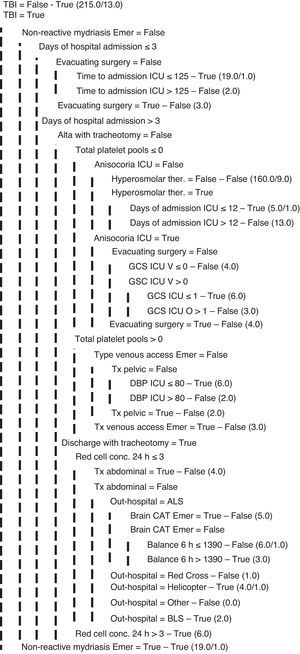
Lastly, on applying data mining algorithms,5,6 the characteristics with the greatest repercussion in terms of mortality were found to be TBI and its associated variables, such as the GCS score (fundamentally referred to its motor component), or maximum ICP (Table 6). Following these variables, we also identified the need for vasoactive drugs at the start of patient care, the transfusion of red cell concentrates, lactate >4mmol/l after 24h of stay in the ICU, patient age, and the days on mechanical ventilation. Posteriorly, different classification algorithms were applied to construct decision trees such as the J48 pruned tree for death, among others, with a view to develop outcome predictor models. As can be seen in Fig. 3, the most determinant elements in terms of mortality were the TBI-related variables, followed by other parameters such as the days of admission, patient age or the days on mechanical ventilation. Of all the applied algorithms, that exhibiting the greatest precision in the global patients was the Adaboost multi-classifier with J48 as base classifier (92%).
Gain in attributes in relation to mortality or poor neurological outcome based on data mining techniques.
| 0.3703155 | 64 TBI |
| 0.1373812 | 17 Poorer total GCS |
| 0.0849137 | 48 GCS ICU |
| 0.0686669 | 49 GCS ICU V |
| 0.0592733 | 73 Maximum ICP |
| 0.056325 | 44 Pre-ICU origin |
| 0.0557942 | 50 GCS ICU M |
| 0.0468255 | 31 Brain CAT Emer. time |
| 0.0461143 | 113 Days MV |
| 0.0447293 | 118 Days hospital admission |
| 0.03866 | 71 Monitoring ICP |
| 0.0383707 | 72 Initial ICP |
| 0.0377903 | 30 Brain CAT Emer. |
| 0.0366105 | 100 NA max. 24h |
| 0.0362324 | 83 Tx abdominal |
| 0.0358942 | 5 Type of accident |
| 0.0352626 | 16 GCS Emer. |
| 0.0327425 | 95 Red cell conc. 6h |
| 0.0327346 | 117 Days admission ICU |
| 0.0276422 | 92 Balance 6h |
| 0.0258824 | 94 NA max. 6h |
| 0.0257191 | 65 Evacuating surgery |
| 0.0249857 | 98 Balance 24h |
| 0.0237734 | 51 GCS ICU O |
| 0.0220307 | 19 Non-reactive mydriasis Emer. |
| 0.0212844 | 3 Origin |
| 0.0179667 | 82 Thoracic drainage ICU |
| 0.0165572 | 67 Hyperosmolar ther. |
| 0.0159594 | 84 Laparotomy |
| 0.0157081 | 40 Crystalloids Emer. |
| 0.0153467 | 29 ECO FAST Emer. time |
| 0.0148084 | 26 Chest Rx Emer. |
| 0.0134527 | 28 ECO FAST Emer. |
| 0.0133546 | 87 Tx pelvic |
| 0.0129294 | 32 TAC thorax/abd. Emer. |
| 0.0127884 | 80 Tx thorax |
| 0.012545 | 86 Tx solid organ |
| 0.0122175 | 79 Tx facial |
| 0.0121557 | 4 Out-hospital |
| 0.0119424 | 68 Barbiturate coma |
| 0.0104189 | 53 Non-reactive mydriasis ICU |
As has been evidenced by many studies, one of the factors most closely related to mortality in severe trauma patients is the presence of TBI. The prognosis of such patients can be determined from the pupillary alterations and GCS score,7–9 both of which were identified by the statistical tests used in our study. In order to improve the prognosis of patients with TBI, the Brain Trauma Foundation guidelines establish a series of initial management principles based on scientific evidence.10,11 Regarding therapeutic maneuvering in the general management of polytraumatized patients, adherence to the recommendations of the Advanced Trauma Life Support (ATLS) program results in lowered mortality, as affirmed by van Olden et al. in 2004,12 though Pfeifer et al. in 2009,13 in a study on the evolution of such mortality over 30 years, concluded that the mentioned decrease is attributable to a reduction in deaths due to bleeding, while deaths due to TBI or multiorgan failure remain stable. This affirmation was based on a systematic review of different studies, with no type of meta-analysis, reflecting a mortality rate in the reviewed studies of between 9 and 49.8%. Our own data are at the lower limit of this range.
The determination of lactate concentration has been introduced in recent years for the assessment of shock.14–16 Despite controversy about the usefulness of lactate in assessing the clinical situation of a patient and the success of resuscitation, many studies speak in favor of the determination of this parameter. In relation to this point, Blow in 199917 indicated that patients in whom the lactate levels could not be reduced or normalized within the first 24h experienced greater mortality. This is why this crucial first day is referred to as the “silver day”. With a view to minimizing this problem, therapeutic maneuvering is indicated, e.g., early surgery or intensive resuscitation, along with other management measures that could be encompassed within what is known as “damage control”.18
The patient population in our setting is older than in other studies found in the literature.19,20 This is mainly due to aging of the population in the region of Castilla y León, and particularly in the province of Salamanca. No major differences were observed as regards the causes of trauma with respect to other studies, except for a small increase in the number of falls–this fundamentally being explained by the larger presence of individuals over 65 years of age in our series. The mortality rate in our study is consistent with the figures published elsewhere (11–15%).19–22
Reducing the patient care and transfer times until definitive admission to the ICU is important for improving survival. As has been reflected in a study comparing the outcomes of trauma in the urban versus the rural setting,23,24 differences in the time of transfer to hospital are associated to increased mortality, without differences in terms of the ultimate outcome between the two groups once the patients reach the hospital. Some studies have considered separate groups corresponding to urban care and rural care. In our series the distinction was referred to times of transfer to hospital, with the documentation of a tendency toward greater mortality in the case of longer transfer times. Those patients who present some severity criterion upon admission to emergency care stand to benefit from early assessment by an experienced trauma team, as has been evidenced by a number of authors; our efforts therefore should focus on greater protocolization based on already established recommendations that have been shown to be effective.25–28 Such protocolization exerts a decisive influence in reducing the times to definitive patient care.
The development of registries in Intensive Care Medicine contributes to improve the care of patients requiring admission to the ICU mainly through knowledge of the characteristics and therapeutic maneuvers depending on the type of disease condition involved. Polytraumatized patients constitute an important group of individuals requiring admission to the ICU; in our setting they represent 15.6% of all emergency admissions and 7.6% of the total admissions to the ICU. In recent years, both national and European trauma registries have been developed.20,29 In Spain, a new national polytrauma registry is under development,30 and the present study offers a possible reference for establishing comparisons.
The limitations of this study may be the fact that it is a single-center initiative involving a retrospective review, with the inclusion of patients who were referred to the Salamanca Hospital Complex from other provinces. Nevertheless, we identified and eliminated the possible confounding factors, and recorded no statistically significant differences in mortality according to the origin of the studied variables.
In conclusion, the use of less common statistical techniques such as data mining or MultBiplot allowed identification of the variables with the greatest influence upon mortality among polytraumatized patients–the results being consistent with those produced by classical statistical methods. In our study, the variables related to the presence of TBI were seen to be important, though lactate concentration was also important in terms of patient prognosis. In effect, this parameter is relevant both for assessing the hemodynamic situation of polytraumatized patients and as an endpoint for monitoring the efficacy of the adopted resuscitation measures. In turn, the present study points to the need for correct protocolization in order to shorten the patient care times–which exert a decisive influence upon patient prognosis and mortality–and the need for registries which can be used to define possible measures and opportunities for improving patient care.
Financial supportThere has been no partial or full financial support of this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Robledo J, Martín-González F, Moreno-García M, Sánchez-Barba M, Sánchez-Hernández F. Factores pronósticos relacionados con la mortalidad del paciente con trauma grave: desde la atención prehospitalaria hasta la Unidad de Cuidados Intensivos. Med Intensiva. 2015;39:412–421.