To identify risk factors for worsened quality of life (QoL) and activities of daily living (ADL) at 3 and 12 months after discharge from the Intensive Care Unit (ICU) in patients on mechanical ventilation (MV).
DesignA prospective, multicentric observational study was made.
SettingThree ICUs in Argentina.
PatientsThe study included a total of 84 out of 129 mainly clinical patients admitted between 2011–2012 and requiring over 24hours of MV.
InterventionsNo interventions were carried out.
VariablesQuality of life was assessed with the EQ-5D (version for Argentina), and ADL with the Barthel index.
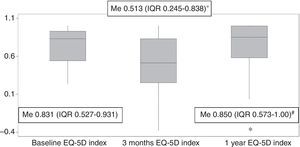
ResultsThe EQ-5D and Barthel scores were assessed upon admission to the ICU (baseline) and after three months and one year of follow-up. Comorbidities, delirium, ICU acquired weakness (ICUAW), and medication received were daily assessed during ICU stay. The baseline QoL of the global sample showed a median index of [0.831 (IQR25–75% 0.527–0.931)], versus [0.513 (IQR0.245–0.838)] after three months and [0.850 (IQR0.573–1.00)] after one year. Significant differences were observed compared with QoL in the Argentinean general population [mean 0.880 (CI 0.872–0.888), p<0.001; p<0.001; p0.002]. Individual analysis showed that 67% of the patients had worsened their QoL at three months, while 33% had recovered their QoL.
In the multivariate analysis, the variables found to be independent predictors of worsened QoL were a hospital stay ≥21 days [OR 12.57 (2.75–57.47)], age ≥50 years [OR 5.61 (1.27–24.83)], previous poor QoL [OR 0.11 (0.02–0.54)] and persistent ICUAW [OR 8.32 (1.22–56.74)]. Similar results were found for the worsening of ADL.
ConclusionsQuality of life is altered after critical illness, and its recovery is gradual over time. Age, length of hospital stay, previous QoL and persistent ICUAW seem to be risk factors for worsened QoL.
Identificar los factores de riesgo relacionados con el empeoramiento de la QOL y actividades de la vida diaria (AVD) a los 3 meses y al año del alta de la unidad de cuidados intensivos (ICU) en pacientes que recibieron ventilación mecánica (VM).
DiseñoProspectivo, observacional.
ÁmbitoTres UCI en Argentina.
PacientesSe incluyó a 84 de 129 pacientes, predominantemente clínicos, que habían sido ingresados en las UCI entre 2011 y 2012 con>24h de VM.
IntervencionesNinguna.
VariablesLa QOL fue evaluada a través del EQ-5D (versión argentina) y las AVD con el índice de Barthel.
ResultadosEl EQ-5D y el índice de Barthel se evaluaron al ingreso a ICU, a los 3 meses y al año de seguimiento. Las comorbilidades, el delirio, la debilidad adquirida en UCI y los fármacos recibidos fueron evaluados diariamente. La QOL basal de toda la muestra exhibió una mediana del índice (0,831 [IQR: 0,527-0,931]), a los 3 meses (0,513 [IQR: 0,245-0,838]) y al año (0,850 [IQR: 0,573-1]) y mostró una diferencia significativa con la QOL de la población general argentina (0,880 (0,872-0,888) p<0,001; p<0,001; p=0,002]. El análisis individual evidenció que el 67% de los pacientes había empeorado su QOL a los 3 meses mientras que el 33% la había recuperado.
En al análisis multivariado, las variables que probaron ser predictores independientes de empeoramiento de QOL fueron estadía hospitalaria≥21 días (OR: 12,57 [2,75-57,47]), edad≥50 años (OR: 5,61 [1,27-24,83]), baja QOL previa (OR: 0,11 [0,02-0,54]), y debilidad adquirida en UCI persistente (OR: 8,32 [1,22-56,74]). Resultados similares se observaron en el empeoramiento de AVD.
ConclusionesLa QOL está alterada tras la enfermedad crítica y su recuperación es gradual en el tiempo. La edad, estadía hospitalaria, QOL previa y debilidad adquirida en UCI persistente parecen ser factores de riesgo que tienden a empeorar la QOL.
Twenty eight percent of the patients who are admitted to ICU (intensive care unit=ICU) with mechanical ventilation requirement (mechanical ventilation=MV) die during their stay at intensive care unit.1 Survivors experienced deterioration in their QOL (quality of life=QOL) and functionality due to physical, psychological and neurocognitive dysfunctions, which in many cases, remain after 5 years of hospital discharge.2,3 These disorders cause that about 50% of patients are unable to return to their previous activities after a year of having been discharged from hospital4; only 13% return to their regular jobs and most of them retire after 5 years.5 Psychological disorders also affect the relatives of the patients admitted to ICU and last over post ICU period.6 In turn, an economic impact is generated, which although heterogeneously studied, is certainly relevant in the post ICU scenario.7 However, studies on selected populations in which QOL return to pre-admission values after 6–9 months have been published.8
There are few published data about QOL after critical illness in Argentina9,10 but they seem to be similar to those in developed countries.11,12 Different risk factors for QOL worsening after intensive care unit therapy that varies according to the studied population such as age, prolonged MV,13 length of hospital stay (length of hospital stay=LHS),14 and diagnostic category4,15 have been described in literature. It is interesting to know risk factors related to quality of life worsening in order to prevent those modifiable ones and early recognize non-modifiable ones to develop an early treatment and an adequate family counseling. For this purpose, we developed a study whose primary objective is to identify risk factors associated with quality of life worsening in the medium and short term in patients receiving invasive mechanical ventilation in Intensive Care Unit more than 24h. We hypothesize that previous QOL, duration of mechanical ventilation, delirium and weakness associated with intensive care (ICU acquired weakness=ICUAW) could be risk factors of quality of life worsening after being discharged from intensive care unit.
MethodsStudy design, patients and settingMulticentric, observational study which included all the adult patients (≥18 years) admitted consecutively to ICU of Clinica Olivos, Sanatorio Anchorena and Clinica Bazterrica, between April 2011 and January 2012, who required MV for more than 24h. The area where the study was conducted was 3 monovalent intensive care units that have intensive care physicians 24hours a day, respiratory therapist, 12hours a day and a nurse every two patients. It should be noted that these institutions receive patients only from the private health system (prepaid health system). The patients readmitted to the ICU were not been considered as new patients, but they were included in the study protocol and all data was analyzed together with data collected in the previous hospitalization.
Patients who received MV for more than 24hours in a previous health center at admission, patients with do not resuscitate (DNR) before or after receiving MV, patients with previous cognitive impairment or unconsciousness (with diagnosis recorded in medical record or family interview) were excluded, and also those patients who did not sign the informed consent, pregnant women and patients with neoplastic or degenerative disease with life expectancy less than a year.
ProceduresEvery day, respiratory therapists were in charge of recollecting the following data. Demographic variables in eligible patients were evaluated: cause of admission to ICU, reason for MV requirement,1 severity of illness at admission (APACHEII score), comorbidities (Charlson index), sedation (Richmond agitation-sedation scale, RASS16), weaning process,17 daily doses of sedatives, analgesics and neuromuscular blockers (NMB), ICUAW (Medical Research Council scale, MRC18: cutoff point 48), delirium (CAM-ICU Spanish version19) and site at discharged from hospitalization: home (with or without home care), or chronic care centers (long term acute care hospital=LTACH).
QOL was assessed by EQ-5D questionnaire, a simple and generic instrument validated in Argentina and valued in Argentinian general population (general population=GP).20 This is a self-administered questionnaire, although phone evaluation has also been recommended21,22 and reliability for measurement by close relatives has been proven (indirectly).23 An index (from 0 to 1) and a (visual analogic scale=VAS) visual analog scale that assesses the overall health status of the patient is obtained from the questionnaire. A complete description of the questionnaire is shown in the electronic supplement. It was delivered to the patient (or family cohabiting in case the patient was unable to complete it) once the informed consent was signed; the results of this first evaluation were referred to four weeks prior to admission. All patients who were able to communicate countersigned the questionnaire later. Three months and one year after being discharged from ICU, the same questionnaire was reassessed by phone to the patient or family cohabitant (proxy), preferably, the same family member who performed it at admission to ICU, in case the patient cannot refer it. The proxy is defined as the person in daily contact with the patient before admission to the ICU. Since our study includes a small number of patients and was not supported by any pharmaceutical/medical firm, the use of the questionnaire was free of charge. Functional status was assessed by independence in activities of daily life (activities of daily living=ADL) not only basic ones, but also instrumental ones that determine people's autonomy. We have used Barthel index since it is one of the most popular generic measures, studied and spread worldwide, assigning different scores according to the level of independence regarding basic activities of daily life. This test has been validated in Argentina24 and for phone use. All Phone calls were made by the first author. A detailed description of the characteristics of ICUs and procedures performed during the study can be found in the electronic supplement.
Ethics considerationsThis study was approved by the Ethics Committee of the three Institutions in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments and also recommended and approved Informed Consent used.
Statistical analysisContinuous variables are expressed as median and interquartile range (interquartile range (IQR)) represented by the 25–75 percentile or mean and standard deviation (SD), and categorical variables, as absolute value and percentage. For data analysis, parametric (t test, ANOVA) and nonparametric (Mann Whitney) tests, according to the frequency distribution of continuous variables were used, and Chi square, for categorical variables. Wilcoxon signed rank test was used to compare repeated measurements (EQ-5D and VAS). Logistic regression was performed, the entry criteria for multivariate analysis was p=0.10. A p value less than or equal to 0.05 were considered significant.
This is a prospective cohort study, but the main analysis corresponds to a design of cases and case–control study (nested).
Paired samples are studied; therefore, risk factors will be analyzed based on a conditional logistic regression model. According to this criterion, the sample size was calculated according to the classic recommendation of Freeman (n=10×(K+1). It is estimated that the inclusion of 110 patients will require six months of recruitment. To classify quality of life prior to admission as “good” or “poor”, the study of quality of life in healthy people of Argentina's population was used. It was considered “poor quality of life on admission” when baseline EQ-5D index value was less than lower the confidence interval (CI=confidence interval), and “good” when the index value was equal to or higher. It was considered worsening quality of life when the value of the EQ-5D index at 3 months was less than the lower limit of the confidence interval of the baseline index. The same criterion was used to categorize the QOL one year after discharging from ICU.
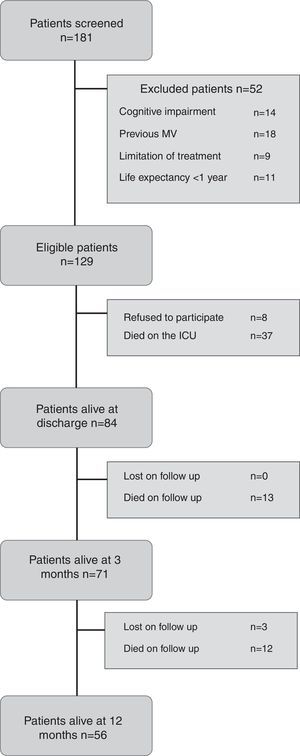
ResultsSample characteristicsIn the mentioned period, 181 patients receiving MV for more than 24hours were admitted at 3 ICUs (Fig. 1); 52 patients were excluded. Of the 129 eligible patients, eight of them refused to sign the consent, 37 died in ICU, and 84 patients who were discharged from the ICU, formed the study sample. At 3 months of follow-up, 13 patients had died (5 of them in the hospital), 71 were alive but only 70 could be evaluated. After one year of follow-up, 12 more patients had deceased (total of 25; 30%), 56 were alive (55 were tested) and 3 were lost at follow up.
The characteristics of the patients who entered the study are listed in Table 1. The level of education of the patients was 22.6% primary education, 47.6% secondary education and 29.8% college education; 75% of patients were active from the labor point of view (65.5% employee or independent, household activities 6%, student 3.6%) while 25% were retired. Most patients were referred by hospital emergency (60%), while the rest came from the hospitalization area (33%) or another institution (7%). The drugs most used to achieve sedo-analgesia were midazolam in 85% of patients and fentanyl in 88%, although to a much lesser extent, they were also used: remifentanyl in 15%, dexmedetomidine in 17%, lorazepam in 17% and propofol in 13%. The NMB were only used in 8 patients and for short periods of time. Of all the patients using dexmedetomidine (n=14), over 70% used it during NIV (noninvasive ventilation=NIV) after extubation (n=10). The presence of delirium was observed in 57 patients (72%) (5 of them were in a coma, therefore they could not be evaluated) during their stay in ICU; the median duration was [3 days (IQR25–75% 2–6)]; except for 7 patients, all were free of delirium at discharge from ICU. All patients received early mobilization and were evaluated according to their functional achievements; 71% managed to sit on the edge of the bed, 51% did so in a chair and 33% stood up before being discharged from ICU. The ICUAW measured by the MRC score in the wake of the MV was observed in 50 patients (59%); 30 of them (36%) continued with a score <48 at discharge from ICU. The median baseline QOL (corresponding to four weeks prior to admission) showed an index of [0.831 (0.527–0.931 IQR25–75%)], VAS [70 (50–80 IQR25–75%)] and Barthel [100 points (95–100 IQR25–75%)], that is, most of our patients had a good quality of life and functionality before admission to ICU but less than the GP by age (mean 0.880 CI (0.872–0.888) p<0.001). Patients who survived (n=79) were discharged to their homes (n=36), or their homes with home care (n=20) or LTACH (n=22); 1 patient was lost at follow-up.
Characteristics of the sample.
| Variables | Patients alive at discharge n=84 |
|---|---|
| Age (years) – mean (SD) | 59.6 (17.6) |
| Male Sex – No. (%) | 45 (53.6) |
| APACHE II – median (IQR) | 17 (10–25) |
| Charlson – median (IQR) | 3 (1–5) |
| Reason for admission ICU (%) | |
| Medical | 81 |
| Surgical | 12 |
| Trauma | 5 |
| Trauma with TBI | 2 |
| Reason for MV (%) | |
| ARF | 65.5 |
| Coma | 25 |
| Acute exacerbation | 8.3 |
| Neuromuscular disease | 1.2 |
| Mechanical Ventilation days – median (IQR) | 5 (3–8) |
| Weaning process (%) | |
| Simple | 75 |
| Difficult | 14.3 |
| Prolonged | 10.7 |
| Length of ICU stay (days) – median (IQR) | 13 (8–22) |
| Length of Hospital stay (days) – median (IQR) | 24.5 (14–38) |
| Tracheotomy No. (%) | 11 (13) |
Characteristics of patients that survived to ICU and were included on the study. MV: mechanical ventilation. IQR: interquartile range. ARF: acute respiratory failure. TBI: traumatic brain injury. Reason for MV[Acute Respiratory Failure (Postoperative Pneumonia, Congestive Heart Failure, Sepsis, Trauma, ARDS, Aspiration, Cardiac arrest, Other cause), Coma, Acute exacerbation of chronic disease (COPD, Asthma, chronic respiratory disease not COPD) Neuromuscular disease].
At 3 months of follow-up, 70 patients were included in the analysis. The interview was direct in 62% of cases and 38% through relatives (proxies). After being discharged from ICU, 57% of patients received functional rehabilitation from 1 to 3 months, while only 29% received psychological treatment. Although 20% had to be readmitted for a median time of 8 days (1–50), none required MV. After a year of follow up, 55 interviews were included, 73.6% directly and the rest, through relatives (proxies).
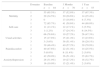
The results of the EQ-5D index are shown in Table 2. The 73% (n=51) could not perform activities of daily life as they did before admission to ICU (study, work, household activities, etc.) and 53%, after one year of follow up.
Results EQ-5D questionnaire.
| Domains | Baseline n=84 | 3 Months n=70 | 1 Year n=55 | |
|---|---|---|---|---|
| Mobility | 1 | 55 (65.5%) | 37 (52.8%) | 37 (67.3%) |
| 2 | 29 (34.5%) | 20 (28.6%) | 14 (25.4%) | |
| 3 | 0 | 13 (18.6%) | 4 (7.3%) | |
| Self-care | 1 | 72 (85.7%) | 41 (58.6%) | 44 (80.0%) |
| 2 | 11 (13.1%) | 12 (17.1%) | 3 (5.5%) | |
| 3 | 1 (1.2%) | 17 (24.3%) | 8 (14.5%) | |
| Usual activities | 1 | 66 (78.6%) | 19 (27.2%) | 26 (47.3%) |
| 2 | 15 (17.8%) | 15 (21.4%) | 13 (23.6%) | |
| 3 | 3 (3.6%) | 36 (51.4%) | 16 (29.1%) | |
| Pain/disconfort | 1 | 39 (46.4%) | 40 (57.2%) | 39 (70.9%) |
| 2 | 40 (47.6%) | 22 (31.4%) | 14 (25.5%) | |
| 3 | 5 (6.0%) | 8 (11.4%) | 2 (3.6%) | |
| Anxiety/depression | 1 | 42 (50.0%) | 36 (51.4%) | 35 (63.7%) |
| 2 | 26 (31.0%) | 19 (27.2%) | 18 (32.7%) | |
| 3 | 16 (19.0%) | 15 (21.4%) | 2 (3.6%) |
Results of EQ-5D questionnaire at baseline, 3 months and 1 year of follow-up. Note that usual activities are the most impaired domain during follow up period.
1: no problems, 2: some/moderate problems and 3: severe/extreme problems.
The EQ-5D index at 3 months was [0.513 median (0.245–0.838 IQR25–75%)] much lower than the Argentina GP by age (p<0.001). When compared baseline index [0.831 median (0.612–0.931 IQR25–75%)] with index at 3 months, a significant difference p<0.001 was observed. The EQ-5D index after a year was [0.850 median (0.573–1.00 IQR25–75%)] and differed significantly from GP (p=0.0021) and the index at 3 months (p<0.001) but it was similar to baseline index (p0.857) (Fig. 2). EQ-5D VAS value at 3 months had a median of [70 (IQR25–75%) 55–80] similar to the value on admission (p=0.808); after a year was [80 (IQR70–90)] and showed a significant difference between the results at 3 months (p0.011) and on admission to ICU (p0.012). The Barthel Score was [median 97.5 (53.7–100 IQR25–75%)] at 3 months, significantly less than on admission (p<0.001). After one year, Barthel median was [100 (IQR90–100)], significantly higher than the value at 3 months (p0.006), but still lower than the value reported on admission (p0.014). Another way of presenting the results is in relation to independence in ADL (Table 3). It should be pointed out that at 3 months and at one year of follow up, 51% and 32% of patients had some degree of dependence compared to 27% of them recorded on admission.
Barthel Index.
| Baseline Barthel n=84 | Barthel 3 months n=70 | Barthel 1 year n=55 | |
|---|---|---|---|
| Barthel Index – median (IQR) | 100 (95–100) | 97 (53.7–100)* | 100 (90–100)#,& |
| Independence on ADL – No. (%) | 61 (72.6%) | 34 (48.6%) | 37 (67.2%) |
| Dependence on ADL – No. (%) | 23 (27.4%) | 36 (51.4%) | 18 (32.8%) |
Barthel Index results at baseline, 3 months and 1 year follow-up.
The EQ-5D baseline index of each patient and the index that showed the same patient at 3 months after being discharged were compared. Of the 70 patients who survived at 3 months, 47 (67.1%) showed deterioration in quality of life score with respect to the one on admission [median baseline index 0.883 (0.651–0.931 IQR25–75%)] and at 3 months [median 0419 (0.05–0.453 IQR25–75%)]; however 23 patients (32.9%) were included into the confidence interval of baseline index [baseline index 0.651 (0.480–0.883 IQR25–75%)] and at 3 months [median 1.0 (IQR25–75 0.831–1.0%)]. According to these results, we can distinguish two subgroups and compare variables. In univariate analysis LHS, stay in ICU, age, days in delirium, previous QOL, persistent ICUAW and site after being discharged were significant factors (Table 4). Other variables such as gender, severity of illness on admission (APACHEII), presence of comorbidities (Charlson score), cause of MV, days of MV or reason for admission had no significance. Post ICU rehabilitation (patients discharged with home care or to LTACH) was prescribed according to medical decision. Most of these patients were dependent on DLA. We hypothesize that rehabilitation was finally indicated to more severe patients at discharge from hospital; that may be the reason why it showed an increase on the OR for worsening QOL (Table 4).
Univariate model for QOL worsening. Logistic Regression EQ-5D.
| Variable | p | OR |
|---|---|---|
| Age ≥ 50 years | 0.015 | 3.87 (1.30–11.56) |
| LHS ≥ 21 days | <0.001 | 12.42 (3.57–43.25) |
| ICUAW at discharge | 0.027 | 4.52 (1.18–17.37) |
| Poor baseline QOL | 0.036 | 0.31 (0.10–0.93) |
| Discharge home with home care or LTACH | 0.001 | 13.57 (3.59–52.58) |
| Days with delirium | 0.037 | 1.34 (1.02–1.77) |
| More than 1 day with ICUAW | 0.010 | 4.46 (1.42–14.01) |
| LOS on the ICU | 0.004 | 1.14 (1.04–1.25) |
Univariate model of risk factors for QOL worsening at three months after discharge from ICU.
LHS: length of hospital stay, ICUAW: ICU acquired weakness, LTACH: long term acute care hospital, LOS: length of stay.
In the multivariate model (Table 5) it was observed that the variables that proved to be independent predictors of deterioration of quality of life were: LHS≥21 days, age≥50, previous poor quality of life and persistent ICUAW. The same individual analysis can be performed taking into account the results at one year after discharge. When comparing individual differences between baseline index and the index after a year we found that 41.8% (n=23) continued with worsening QOL [median baseline index 0.883 (IQR0.742–1.0)] and median after a year [0.559 (IQR0.229–0.770)], while the rest (58.2%) had recovered their previous QOL [median baseline index 0.692 (IQR0.486–0.931) and median at one year 1.0 (IQR1.0–1.0)]. The only two predictor of worsening QOL after a year were LHS≥21 days [OR12.55 (3.08–51.24)] and previous poor QOL [OR0.23 (0.06–0.90)].
Multiple regression model for QOL worsening. Logistic Regression EQ-5D.
| Variable | p | OR |
|---|---|---|
| Age ≥ 50 years | 0.023 | 5.61 (1.27–24.83) |
| LHS ≥ 21 days | 0.001 | 12.57 (2.75–57.47) |
| ICUAW at discharge | 0.030 | 8.32 (1.22–56.74) |
| Poor baseline QOL | 0.007 | 0.11 (0.02–0.54) |
Multiple regression model of risk factors for QOL worsening at three months after discharge from ICU.
LHS: length of hospital stay, ICUAW: ICU acquired weakness.
If we analyze the results of Barthel index individually, in the same way we did with the score of quality of life (Barthel on admission – Barthel at discharge) we found that 44.3% of patients worsened their dependence on Basic activities of daily life at 3 months after discharge, while 55.7% had no changes. Risk factors for worsening Barthel score at 3 months after discharge can be observed in Table 6 and they are similar to those described for worsening of QOL. One year after discharge, 15 patients (27%) had a lower value relative to Barthel score regarding admission, while 40 (72.7%) had regained independence in ADL. The only predictor of worsening Barthel score after a year was LHS≥21 days [OR10.83 (2.15–54.70)].
Multiple regression model for ADL worsening. Logistic Regression Barthel Index.
| Variable | p | OR |
|---|---|---|
| LHS ≥ 21 days | <0.001 | 16.28 (4.07–65.06) |
| ICUAW at discharge | 0.010 | 7.01 (1.57–31.37) |
| Poor baseline QOL | 0.041 | 0.24 (0.06–0.95) |
Multiple regression model of risk factors for Barthel index (ADL) worsening at three months after discharge from ICU.
LHS: length of hospital stay, ICUAW: ICU acquired weakness, ADL: activities of daily living.
The findings of this study focus on the description of risk factors related to the worsening quality of life after a critical illness on medical population; still some risk factors are non-modifiable, such as age, previous QOL or derivation site to be discharged, and other partially modifiable such as hospital stay and persistent ICUAW,25 that need to be prevented or at least taken into account for appropriate treatment and family counseling. In turn, this study reinforces the need for an individual assessment of patients for performing a correct analysis of the results related to QOL, as some of them recover after a period of time and others suffer from effects that persist over time. The deterioration of the QOL after critical illness has been described in several studies3,4,8,26; however, many researchers conducted a comprehensive assessment of patients, so study results are confusing. In our study, QOL at 3 months worsened globally, but 33% of patients recovered it in that period. A similar analysis can be performed with results obtained after a year; the overall results of the sample reflect a recovery in QOL while in the individual analysis, 42% had a poorer QOL than they had at ICU admission. These results are similar to those described by Iribarren-Diarasarri27 at 6 months of follow up. They found an overall decrease in QOL, however 20% improved QOL and in another 20%, QOL remained unchanged. Therefore, according to these findings, the recovery time varies depending on the population studied.14,15,27–30
There is an enormous difficulty in defining clinical worsening or “poor” quality of life. A value corresponding to the minimum clinically significant difference (DMCS) in this group of patients has not been found in literature. DMCS values for the published EQ-5D differ widely (0.04–0.12) depending on the disease, the country where the studies conducted and the period of time established for measuring the variable.31–35 According to the aforementioned it is that we consider appropriate to define “worsening” of the QOL when the EQ-5D index of each patient at the 3rd month was below the lower CI of his/her own baseline index.
Most of the risk factors described in our study have already been mentioned in other studies. The age factor and prolonged hospital stay were described in similar populations4,14,28,36; still, the cutoff point values vary considerably. Previous quality of life and its relationship with long-term results have been partially studied. Wehler30 and Vazquez Mata37 found similar results to those recorded by us. Patients whose precondition was damaged could recover and improve their previous status. Persisting ICUAW was also described by other authors and associated with poor functional results until five years after discharge from ICU.3 Fletcher38 could demonstrate consistent neurophysiological evidence of partial muscle denervation (neurophysiologic evidence of chronic partial denervation of muscle) with prior polyneuropathy in more than 90% of patients with prolonged stay after 5 years of discharge. These patients had severe disability and physical function was badly affected. Fan39 observed that the objective weakness at discharge of ICU was associated with their severe physical dysfunction and poor QOL that persisted after two years of discharge.
The self-perception of health status assessed through the EQ-5D VAS score showed no significant differences when compared it on admission with health status at three months. This finding was also described by Badia and coll.15 and could be related to the fact that the EQ-5D index explores specific areas while the VAS is only a general impression of the state of health. Another possible explanation is that some patients reported a better state of health and some others, a worse state of health, and on average, no differences were observed.
Our study has limitations. We could not reach the number of patients needed for our analysis despite prolonged recruitment period and having a low percentage of loss at follow up (3.5%). This could have changed the results. We also could not find any difference in relation to the diagnostic category because our sample was quite homogeneous and we had a very low percentage of patients with trauma who use to experience a substantial deterioration in QOL at discharge from ICU.4,15,29 Another limitation was the telephone interview, although performed only by the first author and with a questionnaire validated for this purpose, we do not know if personal interviews would have showed different results.
ConclusionsThe quality of life of patients receiving MV in ICU is altered after critical illness and recovery is gradual over time, finding a group of patients suffering from the sequels for a longer period. Age, ICU stay and persisting ICUAW seem to be factors that tend to worsen the quality of life; while suffering a poor quality of life prior to admission appears to be a protective factor of QOL worsening. Then, follow up seems to be recommended after critical illness, especially in the presence of risk factors.
Multicenter study of three Intensive Care Units ArgentinaUnidad de Terapia Intensiva, Clínica Olivos SMG, Buenos Aires, Argentina.
Unidad de Terapia Intensiva, Sanatorio Anchorena, CABA, Argentina.
Unidad de Terapia Intensiva, Clínica Bazterrica, CABA, Argentina.
Conflict of interestThe authors declare no conflicts of interest and have not received any financial support from commercial or scientific bodies.
I would like to express my gratitude to the following partners who participated in the studio: Depaoli Silvana1, RT; Jarque Agustina1, RT; Morena Andrea1, RT; Armelino Javier1, RT; Barcena Leandro4, RT; Foster Carolina1, RT; Palmieri Analia1, RT; Leoz Andres2, RT; D‘Annunzio Pablo2, RT; Rienzi Valeria2, RT; Heidenreich Marisol2, RT; Leiva Valeria2, RT; Quiroga Corina2, RT.
1 Unidad de Terapia Intensiva, Clínica Olivos SMG, Buenos Aires, Argentina.
2 Unidad de Terapia Intensiva, Sanatorio Anchorena, CABA, Argentina.
3 Servicio de Neumonologia, Hospital Ramos Mejía, CABA, Argentina
4 Unidad de Terapia Intensiva, Clínica Bazterrica, CABA, Argentina.