To construct a risk prediction model and systematically analyze factors contributing to unplanned weaning during continuous renal replacement therapy (CRRT) in critically ill adult patients.
DesignCross-sectional, single center study.
SettingDialysis Center of Third-level hospital in China.
PatientsEight hundred and thirteen critically ill adults receiving CRRT after exclusions during May 2023 to Dec 2024.
InterventionsProspective collection of variables during hospital admission and follow-up.
Main variables of interestDemographics, clinical conditions, nursing parameters, vascular access, consumables, laboratory profiles, treatment prescriptions, and hemodynamic data.
ResultsIndependent predictors of unplanned weaning included anticoagulant type (nemastat mesylate, OR = 10.20, 95%CI 3.15–33.02), scheduled treatment time > 24 h (OR = 6.66, 95%CI 3.22–13.79), agitation status (OR = 2.76, 95%CI 1.27–6.02), peak venous pressure > 114 mmHg (OR = 3.58, 95%CI 1.84–6.93), peak transmembrane pressure > 172 mmHg (OR = 2.19, 95%CI 1.11–4.33), weight > 70 kg (OR = 2.13, 95%CI 1.13–4.01). The model demonstrated AUCs of 0.874 (training) and 0.730 (validation).
ConclusionsThis nomogram-based model integrates multidimensional risk factors and provides actionable insights for preventing unplanned CRRT weaning. Key clinical strategies include optimizing anticoagulation protocols and monitoring hemodynamic parameters. Further multicenter validation is warranted to improve generalizability.
Construir un modelo de predicción de riesgos y analizar sistemáticamente los factores que contribuyen al destete no planificado durante la terapia continua de reemplazo renal (CRRT) en pacientes adultos en estado crítico.
DiseñoEstudio transversal, unicéntrico.
EntornoCentro de diálisis de un hospital de tercer nivel en China.
Pacientes813 adultos en estado crítico que recibieron CRRT tras las exclusiones entre mayo de 2023 y diciembre de 2024.
IntervencionesRecopilación prospectiva de variables durante la hospitalización y el seguimiento.
Principales variables de interésDatos demográficos, condiciones clínicas, parámetros de enfermería, acceso vascular, consumibles, perfiles de laboratorio, prescripciones de tratamiento y datos hemodinámicos.
ResultadosLos predictores independientes de la retirada no planificada incluyeron el tipo de anticoagulante (mesilato de nemastat, OR = 10,20, IC del 95%: 3,15–33,02), tiempo de tratamiento programado > 24 h (OR = 6,66, IC del 95%: 3,22–13,79), estado de agitación (OR = 2,76, IC del 95%: 1,27–6,02), presión venosa máxima > 114 mmHg (OR = 3,58, IC del 95%: 1,84–6,93), presión transmembrana máxima > 172 mmHg (OR = 2,19, IC del 95%: 1,11–4,33), peso > 70 kg (OR = 2,13, IC del 95%: 1,13–4,01). El modelo mostró AUC de 0,874 (entrenamiento) y 0,730 (validación).
ConclusionesEste modelo basado en un nomograma integra factores de riesgo multidimensionales y proporciona información útil para prevenir el destete no planificado de la CRRT. Las estrategias clínicas clave incluyen la optimización de los protocolos de anticoagulación y la monitorización de los parámetros hemodinámicos. Se requiere una validación multicéntrica adicional para mejorar la generalización.
Continuous renal replacement therapy (CRRT) is a treatment method that replaces impaired renal function with extracorporeal blood purification therapy. It has been widely used in the treatment of critical patients.1,2 However, critical patients often experience unplanned weaning from CRRT due to coagulopathy, weakened immunity, and multi-organ dysfunction.3 Unplanned weaning affects 10%–39% of CRRT sessions, correlating with excess healthcare costs and increased mortality risk.4,5
Early identification of risk factors is key to effectively preventing unplanned weaning during CRRT in critical patients. Existing risk stratification tools predominantly focus on patient-centric biomarkers like haematocrit.6 There are also many studies focusing on treatment data such as anticoagulation protocols and haemodynamics.7,8 Furthermore, nursing experience has also emerged as a key predictor.8
However, the treatment of CRRT in critical patients is complex and requires the creation of comprehensive prediction tools from more perspectives. One study synthesised different prediction models for unplanned weaning of CRRT for comparison, and the results suggested that the prediction effect varied greatly between different models.9 Other researchers conducted meta-analyses and systematic reviews of multiple models for the unplanned weaning of CRRT in critical patients.10,11 Despite being able to synthesise predictors of unplanned weaning from multiple perspectives, the results obtained from meta-analyses need to be further validated in populations to determine their actual predictive effects.
Therefore, the present study provides a comprehensive analysis of various potential risk factors for unplanned weaning during CRRT in adult critical patients. This study aims to provide clinically actionable insights for preventing unplanned weaning while CRRT.
Patients and methodsStudy designThis cross-sectional study enrolled 1039 CRRT patients from the Dialysis Center of the First Affiliated Hospital of Xi'an Jiaotong University from May 2023 to May 2024. The inclusion criteria were: (1) age ≥ 18 years; (2) Critically ill patients receiving CRRT; (3) availability of complete blood count and coagulation profile within 24 h pre-dialysis. Exclusion criteria included: (1) emergency weaning due to life-threatening hypotension or resuscitation; (2) patient intolerance requiring early weaning; (3) non-medical discontinuation (e.g., examination requests, treatment withdrawal, death, power outage); (4) scheduled circuit/filter changes every 6−8 h; (5) incomplete clinical records.
Treatment modelThe treatment regimen for patients is determined by clinicians and nurses based on the patient's condition, and this study does not interfere with their treatment plan. Within the context of the Intensive Care Unit (ICU), CRRT treatment is administered by nurses specialising in critical care to patients classified as critically ill. Patients classified as critically ill and not receiving treatment within the ICU, for example those presenting to the emergency department, are administered CRRT treatment by nurses employed in the haemodialysis department.
Ethical approvalThe study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University (Approval No. XJTU1AF2025LSYY-546). Written informed consent was obtained from all participants, with explicit disclosure of data usage for research purposes.
Data collectionData were systematically collected encompassing eight domains: demographics, disease and conditions, nursing parameters, vascular access, consumable material, laboratory profiles, treatment prescription, and hemodynamic monitoring. A comprehensive list of variables within each domain is provided in Supplementary File A1.
Quality assuranceStandardized data collection forms were utilized to ensure consistency across three trained investigators.
Key variable definitionsUnplanned hemodialysis cessationAdapted from Fei's criteria,12 unplanned weaning during CRRT was defined as premature discontinuation before achieving either ultrafiltration goals or scheduled treatment duration. Thresholds for mandatory termination included: Sustained pressure alarms, including transmembrane pressure, arterial pressure, venous pressure, and waste pressure; Refractory hypotension; Alarms such as poor blood flow cannot be eliminated after adjustment.
Agitation statusAgitation is assessed using the Richmond Agitation-Sedation Scale (RASS) score.13 A RASS score of 2 or higher is defined as agitation.
Physical restraintThe present study employed the Motor Activity Assessment Scale (MAAS) as a tool to evaluate patients' suitability for restraint.14 In instances where the MAAS score ≥ 5, physical restraint was implemented on patients subsequent to the procurement of informed consent. The primary purpose of physical restraint was to protect patient safety and ensure the smooth implementation of clinical treatment.
Statistical analysisAll statistical analyses were conducted using R software (version 4.1.2; R Foundation for Statistical Computing). The dataset was randomly divided into training and validation sets at a 1:1 ratio using stratified sampling to ensure balanced representation of outcomes. Continuous variables were assessed for normality using Kolmogorov-Smirnov tests, reported as mean ± SD (normal) or median[IQR] (non-normal). Group comparisons employed Welch's t-test (normal) or Mann-Whitney U test (non-normal). Categorical variables were analyzed by Pearson χ² or Fisher's exact tests.
Continuous variables were converted into dichotomous variables by referring to the normal clinical range or the maximum Youden index. Potential risk factors for unplanned hemodialysis cessation were initially screened through univariate logistic regression (significance threshold: P < .10). Variables meeting this criterion underwent further selection via LASSO regression with 10-fold cross-validation to address multicollinearity and optimize feature selection. The final multivariable logistic model was refined using the Akaike Information Criterion (AIC) to balance model complexity and predictive performance.15 Model validation included receiver operating characteristic (ROC) curve analysis with area under the curve (AUC) calculations, calibration curve assessment, and internal validation. All hypothesis tests employed two-tailed analyses with significance set at P < .05.
ResultsStudy population characteristicsFrom the initial cohort of 1039 CRRT patients, 813 met inclusion criteria after excluding 226 cases with incomplete data. The flowchart of the research subject dataset is shown in Supplementary files Fig. A1.
The overall cohort had a median age of 57 years (IQR 39–68). No significant difference in age was observed between participants with and without unplanned hemodialysis cessation. Significant disparities were observed in etiology of CRRT, body weight and multiple clinical parameters between patients with and without unplanned dialysis termination, including comorbidities, vascular access, and laboratory profiles. Detailed comparisons across demographics and clinical domains are presented in Supplementary files Table A1.
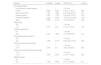
Significant disparities were observed in terms of nursing experience, consumable materials, treatment protocols, and haemodynamic monitoring parameters between patients with and without unplanned dialysis termination. Detailed comparisons of these parameters are systematically presented in Table 1.
Demographics and clinical domains of participants.
| Variable | Planned dialysis termination | Unplanned dialysis termination | P-value |
|---|---|---|---|
| N = 618 | N = 195 | ||
| Nursing parameters | |||
| Shift schedule | .402 | ||
| Day shift | 289(46.76%) | 88(45.13%) | |
| Evening shift | 171(27.67%) | 48(24.62%) | |
| Night shift | 158(25.57%) | 59(30.26%) | |
| Nursing experience (Years) | .003 | ||
| <3 | 93(15.05%) | 39(20%) | |
| 3–5 | 63(10.19%) | 34(17.44%) | |
| 6–10 | 224(36.25%) | 68(34.87%) | |
| >10 | 238(38.51%) | 54(27.69%) | |
| Education level | .582 | ||
| College and below | 5(0.81%) | 0(0%) | |
| Bachelor | 608(98.38%) | 193(98.97%) | |
| Master and above | 5(0.81%) | 2(1.03%) | |
| Professional title | <.001 | ||
| Nurse | 88(14.24%) | 44(22.56%) | |
| Nurse practitioner | 205(33.17%) | 78(40%) | |
| Charge nurse | 325(52.59%) | 73(37.44%) | |
| Hemodialysis specialization tenure (Years) | <.001 | ||
| Median (Q1, Q3) | 8.00 (3.00, 10.00) | 4.00 (2.00, 8.00) | |
| Certification in blood purification nursing | 313(50.65%) | 81(41.54%) | .026 |
| CRRT emergency simulation training | 435(70.39%) | 152(77.95%) | .04 |
| Concurrent patient load | .823 | ||
| 1 | 323(52.27%) | 97(49.74%) | |
| 2 | 236(38.19%) | 84(43.08%) | |
| ≥3 | 59(9.54%) | 14(7.18%) | |
| Consumable materials | |||
| Dialyzer membrane material | <.001 | ||
| AN69 | 540(87.38%) | 147(75.38%) | |
| Polysulfone membrane | 78(12.62%) | 48(24.62%) | |
| Treatment prescription | |||
| Modality | <.001 | ||
| CVVH | 112(18.12%) | 64(32.82%) | |
| CVVHDF | 506(81.88%) | 131(67.18%) | |
| Scheduled treatment time (h) | 12.00 (8.00, 24.00) | 48.00 (24.00, 72.00) | <.001 |
| Heparin dose in priming saline (units/1000 mL) | 6,250.00 (6,250.00, 6,250.00) | 6,250.00 (6,250.00, 6,500.00) | .419 |
| Vein chamber level | .814 | ||
| 1/4 | 1 (0.2%) | 0 (0%) | |
| 1/2 | 54 (8.7%) | 19 (9.7%) | |
| 3/4 | 557 (90%) | 173 (89%) | |
| Full | 6 (1.0%) | 3 (1.5%) | |
| Arteries chamber level | .008 | ||
| 1/2 | 16 (2.6%) | 9 (4.6%) | |
| 3/4 | 166 (27%) | 73 (37%) | |
| Full | 15 (2.4%) | 6 (3.1%) | |
| Not Involving | 421 (68%) | 107 (55%) | |
| Anticoagulant type | <.001 | ||
| Low molecular weight heparin | 260 (42%) | 40 (21%) | |
| Citrate | 242 (39%) | 103 (53%) | |
| Saline timed flush | 16 (2.6%) | 8 (4.1%) | |
| Normal heparin | 14 (2.3%) | 12 (6.2%) | |
| Nemastat mesylate | 55 (8.9%) | 20 (10%) | |
| Other | 31 (5.0%) | 12 (6.2%) | |
| Circuit reversal events | 62 (10%) | 33 (17%) | .013 |
| Blood product administration | 102 (17%) | 47 (24%) | .022 |
| Lipid emulsion administration | 69 (11%) | 44 (23%) | <.001 |
| Hemodynamic monitoring | |||
| Ultrafiltration mean rate (mL/h) | <.001 | ||
| Median (Q1, Q3) | 300.00 (200.00, 450.00) | 200.00 (100.00, 400.00) | |
| Ultrafiltration Peak rate (mL/h) | .003 | ||
| Median (Q1, Q3) | 400.00 (250.00, 500.00) | 350.00 (200.00, 500.00) | |
| Front Replacement fluid flow rate (mL/h) | <.001 | ||
| Median (Q1, Q3) | 0.00 (0.00, 1,000.00) | 0.00 (0.00, 1,000.00) | |
| Rear Replacement fluid flow rate (mL/h) | .025 | ||
| Median (Q1, Q3) | 1,000.00 (1,000.00, 1,000.00) | 1,000.00 (1,000.00, 1,000.00) | |
| Sodium bicarbonate infusion rate (mL/h) | <.001 | ||
| Median (Q1, Q3) | 0.00 (0.00, 80.00) | 0.00 (0.00, 110.00) | |
| Blood flow rate (mL/min) | 160.00 (150.00, 200.00) | 150.00 (120.00, 180.00) | <.001 |
| Peak transmembrane pressure (mmHg) | <.001 | ||
| Median (Q1, Q3) | 125.00 (98.00, 160.00) | 180.00 (120.00, 305.00) | |
| Peak venous pressure (mmHg) | <.001 | ||
| Median (Q1, Q3) | 80.00 (58.00, 104.00) | 115.00 (79.00, 200.00) | |
| Filtration fraction | 0.21 (0.16, 0.29) | 0.28 (0.18, 0.36) | <.001 |
| Grade ≥ 2 filter clotting | 98 (16%) | 89 (46%) | <.001 |
| Blood pump stoppage | 86 (14%) | 59 (30%) | <.001 |
CRRT: continuous renal replacement therapy; CVVH: Continuous Venovenous Hemofiltration; CVVHDF: Continuous Venovenous Hemodiafiltration.
The final analytical sample was randomly divided into training (n = 420) and validation (n = 393) sets. The baseline characteristic of two datasets was in Supplementary files Table A2.
Variable selection processIn the training cohort (n = 420), univariate logistic regression identified 40 variables with P < .10. A list of univariate logistic regression results is provided in Supplementary File Table A3. LASSO regression with 10-fold cross-validation (λ = 0.022) refined the feature set to 14 core predictors (Supplementary files Fig. A2).
Final multivariable modelAccording to the AIC principle, the lower AIC means the better model. The AIC-optimized model demonstrated key predictors: anticoagulant type (nemastat mesylate, OR = 10.20, 95%CI 3.15–33.02), scheduled treatment time > 24 h (OR = 6.66, 95%CI 3.22–13.79).
Other predictors: agitation status (OR = 2.76, 95%CI 1.27–6.02), peak venous pressure > 114 mmHg (OR = 3.58, 95%CI 1.84–6.93), peak transmembrane pressure > 172 mmHg (OR = 2.19, 95%CI 1.11–4.33), weight > 70 kg (OR = 2.13, 95%CI 1.13–4.01).
Full model of multivariable logistic regression is shown in Table 2.
Results of the full model of multivariable logistic regression.
| Variable | Estimate | Statistic | OR (95% CI) | P-value |
|---|---|---|---|---|
| Anticoagulant type | ||||
| Low molecular weight heparin | – | – | 1.00 (ref) | – |
| Citrate | 0.832 | 2.234 | 2.30 (1.11,4.77) | .025 |
| Saline timed flush | 1.434 | 1.692 | 4.20 (0.80,22.10) | .091 |
| Normal heparin | 1.081 | 1.376 | 2.95 (0.63,13.73) | .169 |
| Nemastat mesylate | 2.322 | 3.873 | 10.20 (3.15,33.02) | <.001 |
| Other | 0.086 | 0.123 | 1.09 (0.28,4.27) | .902 |
| Weight (kg) | ||||
| ≤70 | – | – | 1.00 (ref) | – |
| >70 | 0.757 | 2.35 | 2.13 (1.13,4.01) | .019 |
| Catheter dysfunction | ||||
| No | – | – | 1.00 (ref) | – |
| Yes | 0.612 | 1.633 | 1.84 (0.89,3.84) | .103 |
| Scheduled treatment time (H) | ||||
| ≤24 | – | – | 1.00 (ref) | – |
| >24 | 1.896 | 5.105 | 6.66 (3.22,13.79) | .000 |
| Peak venous pressure (mmHg) | ||||
| ≤114 | – | – | 1.00 (ref) | – |
| >114 | 1.274 | 3.77 | 3.58 (1.84,6.93) | .000 |
| Peak transmembrane pressure (mmHg) | ||||
| ≤172 | – | – | 1.00 (ref) | – |
| >172 | 0.784 | 2.256 | 2.19 (1.11,4.33) | .024 |
| Agitation status | ||||
| No | – | – | 1.00 (ref) | – |
| Yes | 1.015 | 2.552 | 2.76 (1.27,6.02) | .011 |
To determine the accuracy of the models, we plotted the ROC curve of the model in training set and test set (Fig. 1). The results suggested that the AUC of the model was 0.874 in the training data, with with 74.34% sensitivity and 88.60% specificity (Table 3). The AUC of the nomogram in test data was 0.730, with 70.73% sensitivity and 72.99% specificity.
In addition, calibration curves were drawn that showed good agreement between the observed and predicted probabilities (Fig. 2).
Nomogram construction and validationFactors that were significant in multivariable regression were used to develop the nomogram to evaluate the risk of unplanned weaning (Fig. 3).
DiscussionThis study developed and validated a multivariable prediction model for unplanned CRRT weaning in critic patients through systematic analysis of multidimensional clinical parameters. Our nomogram demonstrated robust discriminative capacity (AUC 0.874) and clinical interpretability, identifying 7 independent predictors spanning anticoagulation strategies, weight, catheter dysfunction, scheduled treatment time, peak venous pressure, peak transmembrane pressure, and agitation status. These findings extend current risk stratification paradigms.
The risk prediction model has clearly identified the anticoagulation type as an independent risk factor for unplanned CRRT weaning. A salient finding from our study is that nemastat mesylate was associated with the highest risk, followed by citrate. Conversely, low molecular weight heparin demonstrated the most favourable profile in our cohort.
The efficacy of citrate anticoagulation in prolonging filter lifespan when compared with heparin-based regimens has been demonstrated by a high-quality randomized control trial.8 However, no statistically significant difference was observed between the two anticoagulation regimens in outcomes such as duration of kidney replacement therapy and 90-day all-cause mortality.8 A meta-analysis incorporating 38 randomized control trials reached conclusions that are consistent with those of the present study. The citrate group was found to extend filter lifespan, but no statistically significant difference was observed in all-cause mortality outcomes when compared to the heparin anticoagulation regimen.16
However, it should be noted that the duration of the filter and clinical outcome measures, such as all-cause mortality, differ from the endpoint of unplanned weaning in this study. In comparison with the filter lifespan, unplanned weaning is a more clinically comprehensive endpoint influenced by a greater number of patient-specific factors. With regard to patient clinical outcomes, unplanned weaning may be less influenced by patient-specific factors and more by the CRRT treatment protocol. It can be hypothesized that the stability and predictable pharmacokinetics of low molecular weight heparin in severely ill patients may contribute to a reduced risk of unplanned treatment interruption. The findings of this study indicate that the selection of anticoagulant therapy should be tailored to the individual patient, shifting the emphasis from the survival of the filter to a more comprehensive assessment of the patient's overall clinical stability.
In this study, there was an increased risk of unplanned weaning with the nemastat mesylate anticoagulation regimens compared with the low molecular weight heparin anticoagulation regimen. The utilisation of nemastat mesylate is predominantly observed in Asian regions, and extant studies suggest that the concurrent use of nemastat mesylate and citrate does not exert an effect on CRRT treatment outcomes.7 Nevertheless, there have been reports in the literature that the use of nemastat mesylate may pose certain issues with regard to AN69 membrane adsorption. Consequently, the utilisation of nemastat mesylate may necessitate heightened caution, yet it also demands additional evidence to substantiate its implementation.17
Obstruction of the dialyzer or filtration membrane causes an elevation of transmembrane pressure. Higher peak transmembrane pressure results in a relative decrease in the permeability and capacity of the superior pore within the hollow fiber filament membrane, and further extracorporeal coagulation. Therefore, a progressive increase in transmembrane pressure is an important warning for unplanned CRRT weaning. However, the results of this study suggest that when the point measurement of transmural pressure exceeds 172 mmHg, caution should be exercised regarding the occurrence of unplanned CRRT weaning.
Another factor that influences unplanned weaning events is agitation (OR = 2.76), a factor that has been validated in other studies.11 Agitation, caused by impaired patient consciousness, may result in compromised CRRT lines, which increases the risk of accidental disconnections.
The results of this study showed that the peak venous pressure and weight of patients were the factors leading to unplanned weaning during CRRT. In a previous meta-analysis,18 the results showed abnormalities in blood pressure was associated with higher risk of unplanned weaning during CRRT. And excess weight also means potentially poorer vascular function and circulatory load.
The contribution of nursing staff to the effectiveness of CRRT is a pivotal factor in the overall management of the procedure. The centre has enhanced the calibre of nursing personnel operations in CRRT by implementing diverse training programmes. The present study found no nursing factors with the potential to impact CRRT outcomes. Consequently, further investigation is necessary to ascertain the extent to which nursing factors influence the outcomes of CRRT.
Strength and limitationOur systematic factor analysis addresses three critical gaps in existing literature -operational variables, nursing workflow integration, and treatment effects. Our study culminated in a clinically usable nomogram. The nomogram's 74.34% sensitivity at 88.60% specificity suggests utility: high-risk patients (nomogram score > 80th percentile) may benefit from intensified anticoagulation monitoring. What’s more, the model could inform development of automated early-warning systems, particularly for centers with limited CRRT nursing expertise.
While our model demonstrated internal validity, two limitations merit consideration. The present study is confined to a single-center observational study. The single-center design limits generalizability to centers. Static laboratory measures may inadequately capture rapid physiological changes. Future research should prioritize Multicenter validation across diverse anticoagulation protocols.
ConclusionsIn summary, agitation status, peak transmembrane pressure, weight, peak venous pressure, scheduled treatment time, catheter malfunction, and anticoagulant type are risk factors for unplanned weaning of CRRT in critical patients. We have accordingly developed a nomogram with good performance and expect to provide clinical enhancement of CRRT.
CRediT authorship contribution statementXiaomin Liu: formal analysis, writing the original draft, funding acquisition.
Julin Gao: Conceptualisation, methodology, project administration.
Minling Li, Rui Wu, Jiajia Ma, Cunyi Shen, Xiaohong Yang: investigation, data collection.
Meng Wei, Limin Wei, Lei Chen: data entry, data verification.
Qiaoning Wei, Hao He: initial analysis.
All authors reviewed, revised, and approved the final version of the manuscript and agreed to the submission of this manuscript.
Declaration of Generative AI and AI-assisted technologies in the writing processNon-use of any form of AI.
FundingThis work is supported by theKey R&D Plans of Shaanxi Province [2025SF-YBXM-051] and [2025SF-YBXM-375] and The First Affiliated Hospital of Xi'an Jiaotong University [2024-HL-14].
No potential conflict of interest was reported by the authors.
None.