To study the agreement between the level of satisfaction of patients and their families referred to the care and attention received during admission to the ICU.
DesignA prospective, 5-month observational and descriptive study was carried out.
SettingICU of Marqués de Valdecilla University Hospital, Santander (Spain).
SubjectsAdult patients with an ICU stay longer than 24h, who were discharged to the ward during the period of the study, and their relatives.
InterventionInstrument: FS-ICU 34 for assessing family satisfaction, and an adaptation of the FS-ICU 34 for patients. The Cohen kappa index was calculated to assess agreement between answers.
ResultsAn analysis was made of the questionnaires from one same family unit, obtaining 148 pairs of surveys (296 questionnaires). The kappa index ranged between 0.278 and 0.558, which is indicative of mild to moderate agreement.
ConclusionsThe families of patients admitted to the ICU cannot be regarded as good proxies, at least for competent patients. In such cases, we must refer to these patients in order to obtain first hand information on their feelings, perceptions and experiences during admission to the ICU. Only when patients are unable to actively participate in the care process should their relatives be consulted.
Estudiar la concordancia entre los grados de satisfacción de los pacientes y sus familiares (ambos pertenecientes a un mismo núcleo familiar) en cuanto a los cuidados y atenciones proporcionados durante su estancia en la UCI.
DiseñoEstudio transversal, observacional, descriptivo y prospectivo durante 5 meses.
ÁmbitoUCI del Hospital Universitario Marqués de Valdecilla de Santander.
SujetosPacientes mayores de 18 años con estancia mayor de 24h que fueron dados de alta de la UCI durante el período de estudio y familiares de dichos pacientes.
IntervenciónInstrumento: cuestionario FS-ICU 34 para evaluar la satisfacción de los familiares de pacientes ingresados en la UCI y adaptación de dicho cuestionario para el paciente. Se determina el grado de concordancia mediante el índice de kappa ponderado para muestras pareadas.
ResultadosSe analizaron todos los cuestionarios procedentes de un mismo núcleo familiar, obteniéndose un total de 148 pares de cuestionarios (296 encuestas). Se obtuvieron índices kappa que oscilaron entre 0,278 y 0,558, lo que indica grados de concordancia entre débiles y moderados.
ConclusionesLos familiares de los pacientes ingresados en la UCI no pueden ser considerados unos representantes adecuados, al menos para el subgrupo de pacientes competentes. En estos casos debemos acudir a esos pacientes para conocer de primera mano sus sentimientos, percepciones y vivencias durante su estancia en la UCI. Solo cuando los pacientes no están en condiciones de participar activamente en el proceso asistencial debemos acudir a sus familias.
Intensive Care Units (ICUs) have become places where high scientific-technical quality medical care is provided. However, as a result of the characteristics inherent to these Units, such care must also be accompanied by special attention and treatment of the patients and their families.1
In the year 2001, the Institute of Medicine published an article entitled: “Crossing the quality chasm”, which defended the concept of “Medicine focused on the patient”, in contraposition to “Medicine focused on the supplier or on the disease”, which up until then had characterized the physician-patient relationship. The article established a series of recommendations referred to treatment and the decision-making process, based on and adapted to the preferences and opinions of the patients.2
Posteriorly, a number of studies have shown Medicine focused on the patient to be associated to improved clinical outcomes.3,4 In this regard, it is in the ICU where this concept acquires particular relevance, since participation of the patients and their families exerts a profound influence upon the decision-making process and on the ultimate prognosis.5 In the context of the critical patient, we therefore can speak of “Medicine focused on the tandem patient/family”.
Often as a consequence of the disease or because of the seriousness of the clinical condition, patients admitted to the ICU may not be able to actively participate in the care process. Consequently, in this scenario we usually resort to their families. Traditionally, the patient relatives have been viewed as hypothetical “mediators” or “representatives” of the patients as regards care and decision making within the ICU – particularly when the patients themselves are unable to state an opinion or decide about their illness. In this respect, few studies have attempted to gain first hand knowledge of the opinion of the patients in the setting of the ICU.6,7
In recent years, a number of instruments have been developed with the aim of measuring the level of satisfaction of the relatives of patients admitted to the ICU.8–13
However, assessment of the level of satisfaction of the patient admitted to the ICU has not been as well developed as in the case of the relatives.14–17 The main reasons for this seem obvious: the seriousness of the patient condition, which often makes communication impossible; the variety of intensive treatments involved; altered levels of consciousness; and the fact that the mentioned complexity of the situation often causes patients to be unable to make decisions concerning their personal condition. This is the principal reason why the assessment of user satisfaction in the ICU has focused mainly on the patient relatives.
From this perspective, it is necessary for health professionals to know, understand and assume the point of view of the patients in order to increase their satisfaction and the quality of the care provided. Within the intervention lines established by the Strategic Plan of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC), it was considered of interest to develop tools capable of contributing to continuous quality improvement. This gave rise to the document “Quality indicators in the critical patient”, where satisfaction measured by means of a questionnaire addressing perceived quality at discharge from the Department of Intensive Care Medicine (DICM) was defined as a relevant indicator.18
Our group carried out a study evaluating satisfaction in the ICU among both the relatives of surviving patients and the relatives of patients that died, and constituted a pioneering effort in measuring the level of satisfaction among the ICU-discharged patients themselves.19
The present study intends to take a step further by determining whether the relatives can be regarded as good proxies of the patients regarding experiences and decision making, as has traditionally been assumed.
Patients and methodsThe present cross-sectional, prospective, descriptive observational study was carried out during a 5-month period in 2011 in Marqués de Valdecilla University Hospital (Santander, Spain)—a third level hospital serving as reference center in this region of Spain.
The study included competent patients over 18 years of age discharged from the ICU after a stay in the Unit of over 24h, and who agreed to participate in the project, and their direct relatives.
A relative was taken to be a person with close family, social or emotional ties to the patient. This consequently included not only blood relatives but also people close to the patient. Only one relative per patient was considered, with inclusion after agreeing to participate in the study.
The DICM has a total of 30 ICU beds distributed into two Medical-Surgical Units and one Maternal-Children's Unit. The staff in turn is composed of physicians, nurses, nursing assistants and attendants, as well as external staff ascribed to the ICU (e.g., administrative staff).
The patients admitted to the ICU can be medical, surgical (general surgery, neurosurgery, thoracic surgery, specialties), polytrauma cases, or liver, pancreas–kidney and lung transplant patients. Pediatric patients and cardiological or post-heart surgery patients are not included.
Measurement instrumentOf all the instruments described in the literature for measuring family satisfaction, we decided to use the Family Satisfaction in the Intensive Care Unit (FS-ICU 34) questionnaire in its Spanish language version, with some concrete modifications such as the inclusion of questions referred to the work of the nursing assistants and attendants grouped under “other ICU staff”, in order to adjust the instrument to the concrete needs of our setting.
In an attempt to incorporate the key elements of a good ICU humanization plan, we moreover included questions regarding the management of symptoms and perceptions, rating of the work and attention received by the different professionals, the ICU environment (noise, illumination, intimacy and comfort), assessment of visits and the work done by the Extended Intensive Care Service.20
During patient admission, we identified the corresponding relative and assessed patient competence or not for inclusion in the study. At least 24h after discharge from the Unit, and once in the hospital ward, an intensivist delivered the questionnaires to the patient and family, and retrieved them a few days later.
In order to measure the satisfaction of the patients, we adapted the items of the dimension referred to care of the FS-ICU 34 family questionnaire. Questions relating to demographic data were included. The rest of the study questionnaire followed a structure parallel to the family questionnaire, including the sections referred to care received, nursing staff, medical staff, other ICU staff, the wish for religious or psychological support, the ICU environment (noise, illumination, intimacy and comfort), the assessment of visits, and a global evaluation of the care and work carried out by the Extended Intensive Care Service. Lastly, an open-format question addressing comments or suggestions was included.
Exclusion criteriaThe exclusion criteria varied slightly according to the target population involved (i.e., patients or relatives).
Patients interviewed: We excluded patients under 18 years of age; those discharge with a Glasgow coma score of under 15; patients with an ICU stay of less than 24h; patients in which consensus-based limitation of therapeutic effort was decided; patients who died in the first 24h of stay in the hospital ward following discharge from the ICU; individuals discharged home within the first 24h of admission to the hospital ward; patients moved from the ICU to another hospital center; and individuals who for some reason were unable to read or understand Spanish.
Relatives interviewed: We excluded individuals under 18 years of age; the relatives of patients who died in the first 24h of stay in the hospital ward following discharge from the ICU; the relatives of patients discharged home within the first 24h of admission to the hospital ward; the relatives of patients moved from the ICU to another hospital center; and individuals who for some reason were unable to read or understand Spanish.
Questionnaires returned without answering were also regarded as excluded cases (patients or relatives, as applicable).
Ethical particularsThe study project was evaluated and approved by the local Clinical Research Ethics Committee.
Statistical analysisContinuous variables were expressed as the mean±standard deviation (SD).
Conversion of the format of the questionnaire answers (Likert scale) to a 1–100 numerical scale (where 0=worst result and 100=best result) proved necessary in order to apply the required statistical calculations. The authors, in both the original version of the instrument (FS-ICU 34) and in its shorter version (FS-ICU 24), recommend such conversion to allow more concrete processing of the results.
The Wilcoxon test for paired samples was used to compare the answers of the patients and relatives pertaining to the same family unit, since the data exhibited a non-normal distribution. In turn, the weighted kappa index (κ) for paired samples was used to measure the degree of agreement between the answers of both groups, since more than two categories on an ordinal scale were involved.
The kappa index ranges between 0 and 1, distributed as follows: κ≤0.20: poor agreement; 0.21≥κ≤0.40: weak agreement; 0.41≥κ≤0.60: moderate agreement; 0.61≥κ≤0.80: good agreement; 0.81≥κ≤1.00: excellent agreement.
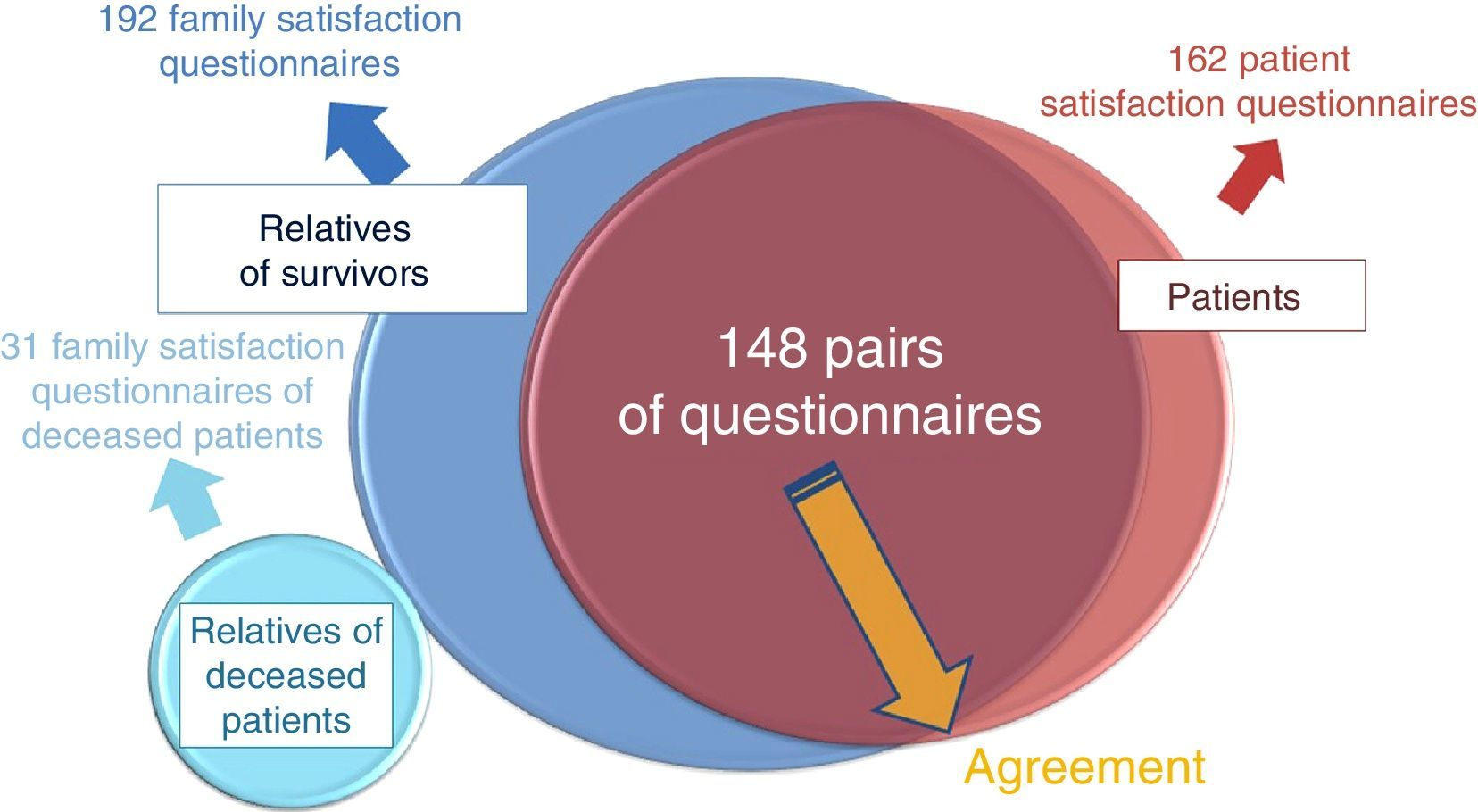
ResultsA total of 538 patients were admitted to the ICU during the study period. Following application of the different exclusion criteria, a total of 148 pairs of questionnaires (patient and relative) were collected—each corresponding to one same family unit (Fig. 1).
A total of 148 patients were finally interviewed—this representing 27.5% of the total patients admitted to the ICU during the study period (n=538; 103 deaths, 13 subjects under 18 years of age, 31 non-competent patients, 48 subjects in the ICU<24h, 14 with limitation of therapeutic effort in the ward, 8 deaths in the ward, 28 discharges to the hospital ward within less than 24h, 41 transfers to another hospital, 10 cases presenting cultural differences, 20 non-answered questionnaires, 60 system losses, 14 patient questionnaires not accompanied by the corresponding family questionnaire).
The age mean was 53.14±13.89 years. Ninety-five responders were males (64.1%), and 104 lived outside the city (70.2%). The mean APACHE II score was 14.16±6.98.
Family characteristicsThe age mean of the interviewed relatives was 46.23±11.62 years. A total of 103 were females (69.59%). The most frequent kinship corresponded to wives (n=40, 27.02%), followed by daughters (n=31, 20.94%). Over one-half of the relatives (n=85, 57.43%) had no previous experience of the ICU. Most lived with the patient in the same home, and over 70% saw the patient more than once a week. A total of 120 of the interviewed families lived in the province (75.67%).
The levels of satisfaction in both groups were rated as “very good”: global satisfaction with the care received being 84.96±11.91 points for the patients and 82.90±12.63 for the relatives.
Comparison of resultsMost of those interviewed considered the care received to be “very good” (the level of satisfaction according to the relatives being 79.6±12.6 points, versus 82.4±11.9 among the patients).
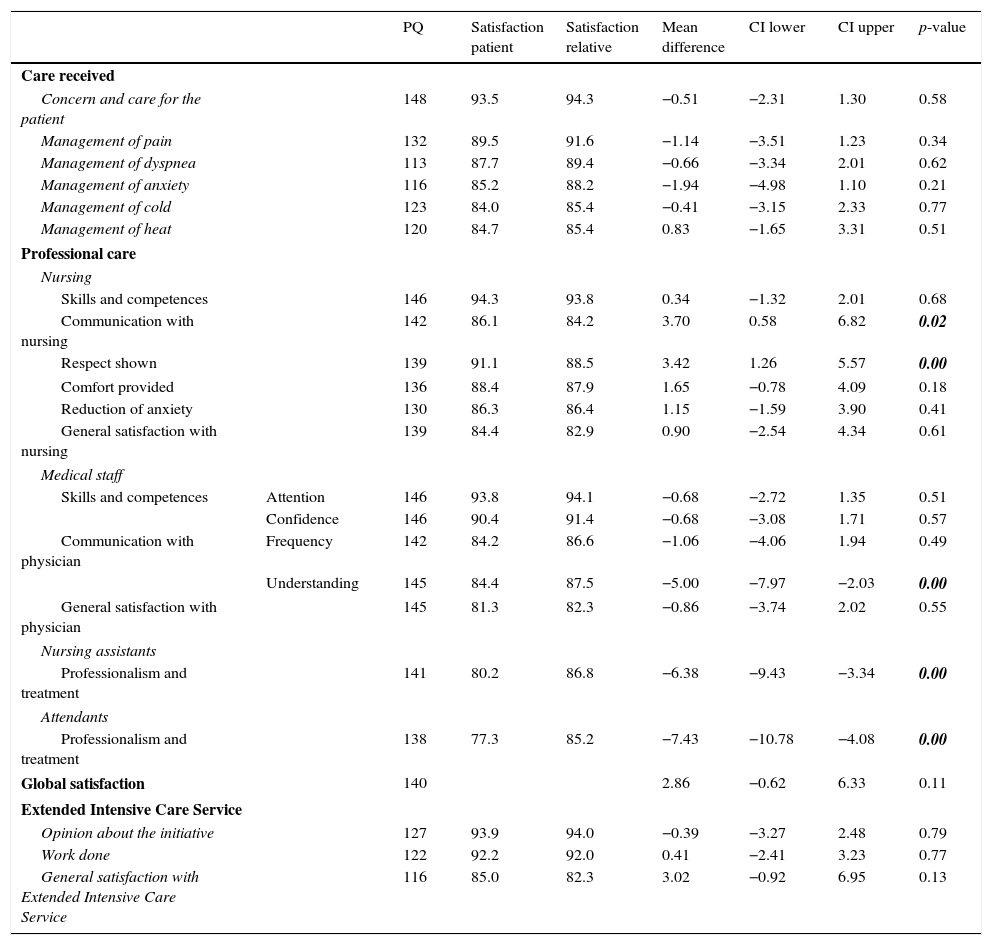
On comparing the results between patients and relatives (within one same family unit/paired samples), the levels of satisfaction were very high in both groups, and significant differences (p<0.05) were only observed in relation to 5 items: two referred to the nursing staff (communication and respect shown: 86.1±18.4 vs 84.2±19.3, respectively, and 91.1±13.3 vs 88.5±14.2), one referred to the medical staff (understanding of the medical explanations: 84.4±18.9 vs 87.5±18.5) and two referred to other staff (attendants: 77.3±21.9 vs 85.2±15.5; nursing assistants: 80.2±21.7 vs 86.8±15.8) (Table 1).
Comparison of means for paired samples (of the same family unit) between the answers of the patients and their relatives.
| PQ | Satisfaction patient | Satisfaction relative | Mean difference | CI lower | CI upper | p-value | ||
|---|---|---|---|---|---|---|---|---|
| Care received | ||||||||
| Concern and care for the patient | 148 | 93.5 | 94.3 | −0.51 | −2.31 | 1.30 | 0.58 | |
| Management of pain | 132 | 89.5 | 91.6 | −1.14 | −3.51 | 1.23 | 0.34 | |
| Management of dyspnea | 113 | 87.7 | 89.4 | −0.66 | −3.34 | 2.01 | 0.62 | |
| Management of anxiety | 116 | 85.2 | 88.2 | −1.94 | −4.98 | 1.10 | 0.21 | |
| Management of cold | 123 | 84.0 | 85.4 | −0.41 | −3.15 | 2.33 | 0.77 | |
| Management of heat | 120 | 84.7 | 85.4 | 0.83 | −1.65 | 3.31 | 0.51 | |
| Professional care | ||||||||
| Nursing | ||||||||
| Skills and competences | 146 | 94.3 | 93.8 | 0.34 | −1.32 | 2.01 | 0.68 | |
| Communication with nursing | 142 | 86.1 | 84.2 | 3.70 | 0.58 | 6.82 | 0.02 | |
| Respect shown | 139 | 91.1 | 88.5 | 3.42 | 1.26 | 5.57 | 0.00 | |
| Comfort provided | 136 | 88.4 | 87.9 | 1.65 | −0.78 | 4.09 | 0.18 | |
| Reduction of anxiety | 130 | 86.3 | 86.4 | 1.15 | −1.59 | 3.90 | 0.41 | |
| General satisfaction with nursing | 139 | 84.4 | 82.9 | 0.90 | −2.54 | 4.34 | 0.61 | |
| Medical staff | ||||||||
| Skills and competences | Attention | 146 | 93.8 | 94.1 | −0.68 | −2.72 | 1.35 | 0.51 |
| Confidence | 146 | 90.4 | 91.4 | −0.68 | −3.08 | 1.71 | 0.57 | |
| Communication with physician | Frequency | 142 | 84.2 | 86.6 | −1.06 | −4.06 | 1.94 | 0.49 |
| Understanding | 145 | 84.4 | 87.5 | −5.00 | −7.97 | −2.03 | 0.00 | |
| General satisfaction with physician | 145 | 81.3 | 82.3 | −0.86 | −3.74 | 2.02 | 0.55 | |
| Nursing assistants | ||||||||
| Professionalism and treatment | 141 | 80.2 | 86.8 | −6.38 | −9.43 | −3.34 | 0.00 | |
| Attendants | ||||||||
| Professionalism and treatment | 138 | 77.3 | 85.2 | −7.43 | −10.78 | −4.08 | 0.00 | |
| Global satisfaction | 140 | 2.86 | −0.62 | 6.33 | 0.11 | |||
| Extended Intensive Care Service | ||||||||
| Opinion about the initiative | 127 | 93.9 | 94.0 | −0.39 | −3.27 | 2.48 | 0.79 | |
| Work done | 122 | 92.2 | 92.0 | 0.41 | −2.41 | 3.23 | 0.77 | |
| General satisfaction with Extended Intensive Care Service | 116 | 85.0 | 82.3 | 3.02 | −0.92 | 6.95 | 0.13 | |
Column one examines the pairs of questionnaires (PQ) analyzed; columns two and three refer to the levels of satisfaction of the patients and their relatives; column four shows the differences between means (with negative values when the patient mean is smaller than the mean corresponding to the relative); columns five and six show the 95% confidence intervals (CI) (lower and upper limits); and the last column represents the p-value (level of significance p<0.05). Those values reaching statistical significance appear in italics and boldface.
The first two items referred to the nursing staff received higher scores on the part of the patients than from their relatives. In contrast, understanding of the medical explanations and the attention and professionalism of the nursing assistants and attendants received comparatively poorer scores from the patients.
On comparing these same results between patients and relatives per different subgroups (sex of the patient, sex of the relative, ICU room involved, APACHE II score, residency in the city versus in the province), we identified a number of variables, such as the work of the nursing assistants and attendants, that maintained the same differences in all the mentioned subgroups, with poorer scores given by the patients in all cases. The explanations given by the medical staff were generally also poorer rated by the patients in all the subgroups.
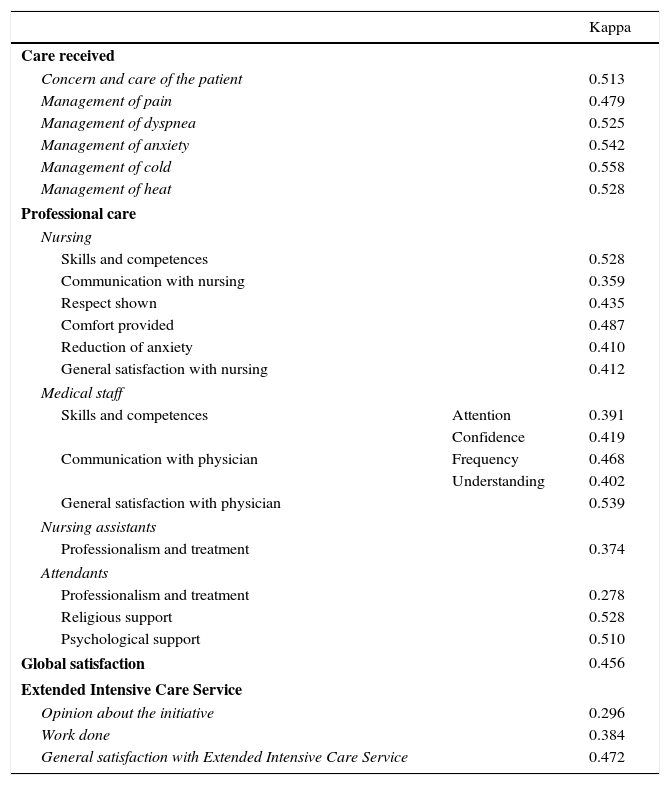
Level of agreement of the answersThe kappa index was used to determine the level of agreement between the patients and their relatives. Agreement proved to be moderate, with κ values between 0.278 and 0.558 (Table 2).
Kappa values between the patients and their relatives.
| Kappa | ||
|---|---|---|
| Care received | ||
| Concern and care of the patient | 0.513 | |
| Management of pain | 0.479 | |
| Management of dyspnea | 0.525 | |
| Management of anxiety | 0.542 | |
| Management of cold | 0.558 | |
| Management of heat | 0.528 | |
| Professional care | ||
| Nursing | ||
| Skills and competences | 0.528 | |
| Communication with nursing | 0.359 | |
| Respect shown | 0.435 | |
| Comfort provided | 0.487 | |
| Reduction of anxiety | 0.410 | |
| General satisfaction with nursing | 0.412 | |
| Medical staff | ||
| Skills and competences | Attention | 0.391 |
| Confidence | 0.419 | |
| Communication with physician | Frequency | 0.468 |
| Understanding | 0.402 | |
| General satisfaction with physician | 0.539 | |
| Nursing assistants | ||
| Professionalism and treatment | 0.374 | |
| Attendants | ||
| Professionalism and treatment | 0.278 | |
| Religious support | 0.528 | |
| Psychological support | 0.510 | |
| Global satisfaction | 0.456 | |
| Extended Intensive Care Service | ||
| Opinion about the initiative | 0.296 | |
| Work done | 0.384 | |
| General satisfaction with Extended Intensive Care Service | 0.472 | |
None of the kappa values exceeded the threshold of 0.6 indicative of good agreement.
The aspects related to the care received by the patient showed moderate agreement, with values between 0.479 and 0.558.
The aspects evaluating the professional care received by the nursing staff and physicians likewise showed weak to moderate agreement—the lowest values corresponding to the communication process.
The lowest level of agreement between patients and relatives was referred to the work of the nursing assistants and attendants.
We also explored the possible existence of differences in agreement according to certain characteristics of the interviewed individuals: sex of the patient, ICU room involved, APACHE II score, sex of the relative, or place of residency. There were no significant differences referred to these characteristics, with the sole exception of the APACHE II score. In effect, the kappa index was almost always greater when the patient APACHE II score was below the median score (i.e., when the patients were less seriously ill).
DiscussionSatisfaction in the ICU has become a very important issue over the last decade, considering that the patients and their families constitute the cornerstone of attention and treatment in the context of critical care. Our group has been working for several years in this field, seeking to know the opinions of these patients and their relatives with a view to improving the quality of our DIMC.19,21
The fundamental aim of this study was to know the direct opinion of the patients that have been admitted to the ICU, and which because of their clinical characteristics were able to answer a questionnaire designed to evaluate their stay in the Unit, compare their answers with those of their relatives, and determine whether the latter can be regarded as adequate proxies of the patients, as has traditionally been assumed.
The levels of satisfaction were high in both interviewed groups. On comparing the answers, we observed significant differences in relation to 5 items. In this regard, the explanations given by the physicians received poorer scores from the patients than from their relatives. This probably reflects usual practice in the ICU, where the medical staff typically spends more time informing the family than the actual patient – perhaps forgetting that the ICU patient might be able to state an opinion and of course receive information.22 In this regard, in the European CoBaTrICE (Competency-Based Training in Intensive Care Medicine) questionnaire, the patients demanded “clarity of the explanations”, defined as “explaining the medical terms in such a way that they are easy to understand”.23
The literature describes several factors that influence the satisfaction of the patients and their relatives in the ICU, with communication in the broadest sense of the word being a key factor. Indeed, information is one of the most highly valued items for the relatives and patients in the DICM.24–28
While the communication and respect received from the nursing staff was associated to high levels of satisfaction in both groups, the scores were higher among the patients than in the case of the relatives. This supports the recommendations of Escudero et al., according to which “the professional must understand, deal with and assertively redirect inadequate emotional reactions while also showing understanding and empathy. The ties between the family and the nursing staff are characterized by greater confidence and the transmission of doubts and concerns. In this regard the information should be divided: nurses should talk about general patient care and the apparatuses used, while the physician should address the diagnosis, treatment and prognosis”.29
The nursing assistants and attendants obtained somewhat lower scores in both interviewed groups. This is difficult to interpret, because such staff members are not comparable to those of other studies, as they are specific of the Spanish healthcare system. The aspects evaluated in relation to these professionals were referred to professionalism and the attention given. It is important to mention that this is one of the items where significant differences were observed between the scores given by the patients and their relatives—the former expressing comparatively lower levels of satisfaction. It is also one of the items showing the poorest agreement between the patients and relatives. The explanation for this could be that these professionals pertain to the ICU and are involved in activities that tend to cause greater patient discomfort (e.g., patient mobilization in the presence of pain, feeding without an appetite, personal hygiene when such measures cause discomfort for the patient, etc.). As a result, these professionals receive poorer scores.
We analyzed the agreement between the answers of the patients and their relatives, and found that the latter are not good proxies of the patients regarding the situations experienced in the ICU—specifically of those patients who are able to answer the questionnaire. The only study addressing this issue to date has been published by Stricker et al.15. These authors carried out a prospective, multicenter observational study involving 235 patients and 266 relatives. The questionnaires were distributed after discharge from the ICU, and the instrument used was the FS-ICU 34 questionnaire in its German language version for the relatives, and an adaptation of that questionnaire in short form and focused on those aspects with a direct bearing upon medical care (e.g., treatment of pain, dyspnea or agitation) for the patients. Both groups showed high levels of satisfaction (with mean scores above 80), with discretely higher scores in the patient group (84.2±16.9 vs 82.2±17.2). On examining the agreement between the answers of the patients and their relatives, the authors obtained kappa indices of between 0.24 and 0.4, i.e., lower than in our own study, though these indices were nevertheless regarded as indicating “moderate agreement”. In addition, the authors compared agreement between the patients and different groups of relatives, and in this regard observed greater agreement when the relatives were the partners or spouses of the patients. The authors concluded that relatives may be regarded as good proxies of the patients. However, κ values of under 0.6 cannot be taken to represent good agreement.30 Consequently, the results obtained by Stricker et al., with κ values below this limit for all the items, are not indicative of good agreement. Unfortunately, the opinions of the subgroup of patients that could not be interviewed (i.e., theoretically the most seriously ill individuals) are not known. As a result, the relatives in this case must be regarded as the only possible proxies as far as care and decision making are concerned, since these at least in theory are the people who know the patients best.
Puntillo et al.16 analyzed the agreement between 245 patients and 243 relatives, 103 nurses and 92 physicians regarding the perception of certain symptoms on the part of the patients, comparing the levels of intensity or discomfort caused by such symptoms in the patients or their relatives. The results yielded correlation coefficients of sufficient magnitude to justify taking the relatives into account when assessing the symptoms of those patients admitted to the ICU who are unable to communicate. Much lower correlation coefficients were obtained in the case of the physicians or nurses. However, the authors concluded that further studies are needed to establish how to measure or rate the perception of certain symptoms among patients that are unable to express themselves during admission to the ICU. In our study, it is important to note that agreement was greater when the patients were less seriously ill. This could be a result of the discussion of feelings and experiences between the patients and their relatives, causing them to show greater agreement in response to questions addressing the care provided. The fact that agreement was poorer in the more seriously ill patients raises an important doubt in relation to the key issue of the study: If agreement between the patients and relatives is poorer when the patients are more seriously ill, is it really acceptable to regard the relatives as adequate proxies or surrogates of the patients?
Until further studies are able to contribute additional information in this regard, the relatives of the more seriously ill patients will continue to be taken as adequate proxies for the assessment of symptoms and in decision making. However, the most relevant conclusion is that whenever possible, patients admitted to the ICU should be asked and evaluated, since they undoubtedly can offer more reliable information about their personal perception during admission to the ICU.
In the context of the current tendency to work to consolidate the structure, organization and functioning of the ICU with a view to improving comfort and ensuring humanization of the care provided,29 dedicating more time and effort to listening to our patients seems a clear option that can help the ICU to become more personalized and comfortable, and capable of offering high human and scientific-technical quality.
ConclusionsThe present study shows that competent patients admitted to the DICM can actively participate in the care process, thus making it feasible to measure their level of satisfaction—this aspect having received little attention in the literature to date.
The FS-ICU 34 questionnaire with minor modifications has been shown to be a valid instrument for assessing the satisfaction of patients discharged from the ICU, and could be used in Spain in other Units of similar characteristics.
As has been reported in the literature, the levels of satisfaction with the care received in the ICU are very high. In our study this has been confirmed for both the patients and their relatives, with no great differences between the two groups in terms of global values.
However, the level of agreement between the patients and their relatives was not found to be as high as theoretically presumed. For this reason, competent patients admitted to the ICU should be asked and considered, since they undoubtedly can offer more reliable information about their personal perception during admission to the ICU.
In the case of patients that are not in a condition to actively participate in the care process, we must resort to the relatives as proxies, since these theoretically are the people who known the patient best and can offer a more reliable impression of his or her feelings, experiences and perceptions.
Financial supportThe project described in this article forms part of a research project of the Marqués de Valdecilla Foundation (“Ayudas para Proyectos de Investigación”, published in the Cantabria Official Government Bulletin on 8 October 2010, reference API 11/15), conducted during the years 2011–2012.
The source of financial support has not participated in the design of the study, data collection, analysis or interpretation of the results, drafting of the manuscript, or in the decision to submit it for publication.
AuthorshipThe signing authors have collaborated in the project described in the article and have read the final manuscript prepared for publication.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Holanda Peña MS, Marina Talledo N, Ots Ruiz E, Lanza Gómez JM, Ruiz Ruiz A, García Miguelez A, et al. Satisfacción en la Unidad de Cuidados Intensivos (UCI): la opinión del paciente como piedra angular. 2017;41:78–85.