To assess the impact of gender upon the prognosis and medical care in a regional acute ST-elevation myocardial infarction management network.
DesignAn observational study was made of consecutive patients entered in a prospective database.
ScopeThe Catalan acute ST-elevation myocardial infarction management network.
PatientsPatients treated between January 2010 and December 2011.
InterventionsPrimary angioplasty, thrombolysis or conservative management.
Variables of interestTime intervals, proportion and type of reperfusion, overall mortality, and in-hospital complication and overall mortality at 30 days and one year were compared in relation to gender.
ResultsOf the 5831 patients attended by the myocardial infarction network, 4380 had a diagnosis of acute ST-elevation myocardial infarction, and 961 (21.9%) were women. Women were older (69.8±13.4 vs. 60.6±12.8 years; p<.001), had a higher prevalence of diabetes (27.1 vs. 18.1%, p<.001), Killip class>I (24.9 vs. 17.3%; p<.001) and no reperfusion (8.8 vs. 5.2%; p<.001) versus men. In addition, women had greater delays in medical care (first medical contact-to-balloon: 132 vs. 122min; p<.001, and symptoms onset-to-balloon: 236 vs. 210min; p<.001). Women presented higher percentages of overall in-hospital complications (20.6 vs. 17.4%; p=.031), in-hospital mortality (4.8 vs. 2.6%; p=.001), 30-day mortality (9.1 vs. 4.5%; p<.001) and one-year mortality (14.0 vs. 8.3%; p<.001) versus men. Nevertheless, after multivariate adjustment, no gender differences in 30-day and one-year mortality were observed.
ConclusionsDespite a higher risk profile and poorer medical management, women present similar 30-day and one-year outcomes as their male counterparts in the context of the myocardial infarction management network.
Evaluar el impacto del género sobre el pronóstico y el manejo en una red regional de atención al infarto agudo de miocardio con elevación del segmento ST.
DiseñoEstudio observacional sobre una base de pacientes consecutivos recogida prospectivamente.
ÁmbitoRed catalana de atención al infarto agudo de miocardio con elevación del segmento ST.
PacientesPacientes atendidos entre enero de 2010 y diciembre de 2011.
IntervencionesAngioplastia primaria, fibrinólisis o manejo conservador.
Variables de interésSe compararon, según el género, intervalos de tiempo, proporción y tipo de reperfusión, mortalidad global y complicaciones intrahospitalarias y mortalidad global a 30 días y un año.
ResultadosDe 5.831 pacientes atendidos, 4.380 tenían diagnóstico de infarto agudo de miocardio con elevación del segmento ST, siendo 961 (21,9%) de ellos mujeres. Estas tenían mayor edad (69,8±13,4 frente a 60,6±12,8 años, p<0,001), mayor prevalencia de diabetes (27,1 frente a 18,1%, p<0,001), Killip>I (24,9 frente a 17,3%, p<0,001) y ausencia de reperfusión (8,8 frente a 5,2%, p<0,001) que los hombres. Además, las mujeres presentaban mayores retrasos en la atención (primer contacto médico-balón: 132 frente a 122min, p<0,001; inicio de síntomas-balón: 236 frente a 210min, p<0,001), más complicaciones intrahospitalarias (20,6 frente a 17,4%, p=0,031) y mortalidad intrahospitalaria, a 30 días y un año (4,8 frente a 2,6%, p=0,001; 9,1 frente a 4,5%, p<0,001; 14,0 frente a 8,3%, p<0,001). Sin embargo, tras el análisis multivariado no hubo diferencias en mortalidad a 30 días y un año.
ConclusionesA pesar del peor perfil de riesgo y el peor tratamiento recibido, las mujeres presentaron similares resultados a 30 días y un año que sus homólogos masculinos atendidos por una red de atención al infarto.
ST-segment elevation acute myocardial infarction (STEMI) is one of the greatest public health problems in society today.1,2 Traditionally, women with STEMI have been considered to have a poorer prognosis than men with the same disorder,3 probably because they receive less optimum management (fewer hospital admissions, a lesser percentage of medical treatments recommended by the clinical practice guides, and a lesser percentage of primary angioplasty [PA]),4 with a greater delay in applying reperfusion therapies.5 However, recent studies, after adjusting for confounding factors, have identified no gender-related differences in terms of the treatment and prognosis of the disease.6,7
The benefits derived from reperfusion therapy in STEMI are conditioned to time.8 Primary angioplasty, performed within the recommended time window, can reduce the mortality and reinfarction risk compared with fibrinolysis.9 Likewise, moving STEMI patients from hospitals where PA is not available 24h a day, 7 days a week (24/7), to centers with PA 24/7 has been shown to be a feasible and safe strategy.10 For this reason, PA is regarded as the treatment of choice in STEMI, provided it is performed by an experienced operator within 120min after first medical contact (FMC).1
The implantation of STEMI management networks has contributed to expand reperfusion therapy, fundamentally involving PA, and thus has helped to generalize optimum treatment for each patient according to the time window recommended by the clinical practice guides.11 However, only limited information is available on the impact of patient gender in STEMI cases attended by networks specifically designed to the effect.4,12 The present study was designed to analyze the impact of gender in terms of the medical care received and upon patient mortality (in-hospital, after 30 days and at one year) in a population attended by a regional STEMI management network.
Material and methodsStudy population, STEMI management network and the Codi Infart registryThe present multicentric observational study is fundamented upon a prospective database of consecutive STEMI patients attended by the Catalan STEMI management network (the Codi Infart registry) from January 2010 to December 2011.
The Autonomous Community of Catalonia is located in North-Eastern Spain and has a population of approximately 7.5 million inhabitants. A STEMI management network was implanted in Catalonia in June 2009.13,14 The network divided Catalonia into reference areas for the 10 pre-existing hospitals with the capacity to perform PA, with the aim of affording the reperfusion therapy best suited to each individual patient. The Codi Infart comprised 5 basic elements: (1) The ambulances of the Medical Emergencies Service (Servei d’Emergencies Mèdiques [SEM]), staffed by physician/s or nurse/s capable of diagnosing the symptoms, interpreting the electrocardiogram (ECG) tracings and of administering fibrinolytic therapy; (2) The SEM coordination center which decided the reperfusion strategy and coordinated the logistics among ambulances, district hospitals and hospitals with the capacity to perform PA; (3) The 10 hospitals with the capacity to perform PA (5 of which had 24/7 availability); (4) The Intensive Care Units (ICUs) or Coronary Units of all the hospitals participating in the project, and which received the patients after undergoing reperfusion treatment; and (5) The inclusion of all the patients attended by the network in a mandatory prospective registry (the Codi Infart registry).
Briefly, the protocol specified that when a medical professional diagnosed STEMI on the basis of clinical criteria and the ECG tracing in the context of FMC, the network was to be activated and the strategy would be chosen according to the clinical practice guides.1 All patients with STEMI directly admitted to a center with the capacity to perform PA underwent PA, while those patients initially attended in hospitals without PA, in primary care centers or directly by the SEM were moved to centers where PA was available, according to the risk profile involved and if the time to PA was expected to be less than 120min. If the time to PA was expected to be longer than 120min, fibrinolytic therapy was provided if compatible with the clinical condition of the patient, and only in the case of failed fibrinolysis was the patient transferred for rescue angioplasty. Secondary prevention in turn was prescribed according to common medical practice in each center.1,2,14
The Codi Infart registry is implemented according to the principles of the Declaration of Helsinki, and complies with all the legal requirements. All the centers were encouraged to keep the registry, and all the patients attended by the network were required to be included in it. Demographic and clinical data were collected, together with information on the procedure, the time intervals, and the in-hospital complications, with telephone follow-up after 30 days. Mortality due to all causes after one year was documented by crossing the data of each patient with the database of the Spanish National Statistics Institute (Instituto Nacional de Estadística [INE]) (death certificates).
Study variablesIn line with the purpose of the study, all the variables were analyzed according to gender. The primary endpoint was mortality due to all causes as determined after one year. The secondary clinical endpoints included: mortality due to all causes in-hospital and after 30 days, and in-hospital complications, defined as the combination of ventricular fibrillation, ventricular tachycardia, asystolia, complete atrioventricular block, atrial fibrillation, cardiogenic shock or the need for mechanical ventilation, and each of the individual components considered separately. Cardiogenic shock was defined as the need for intravenous inotropic drugs and/or intra-aortic balloon counterpulsation in order to keep the systolic blood pressure (SBP) >90mmHg.1 Other secondary endpoints related to medical treatment were also evaluated, such as the type of reperfusion therapy provided, and the following management intervals: symptoms onset-FMC, FMC-diagnostic ECG, diagnostic ECG-balloon, FMC-balloon, and symptoms onset-balloon (total ischemia time).15 First medical contact in turn was defined as the first contact with the healthcare system, where the patient was attended by a physician or nurse on an in-hospital or pre-hospital basis, and with the capacity to activate the STEMI management network.15
All the events were assigned by the Catalan Health Department (Servei Català de la Salut: CatSalut; Departament de Salut, Generalitat de Catalunya). As commented above, all study variables were analyzed according to gender.
Statistical analysisThe normal distribution of continuous variables was assessed based on the Kolmogorov–Smirnov test. Those variables found to present a normal distribution were expressed as the mean (standard deviation [SD]), while those lacking a normal distribution were expressed as the mean (interquartile range [IQR])–comparisons being made using the Student's t-test or Mann–Whitney U test as applicable. Categorical variables in turn were expressed as number (percentage) and were compared using the chi-squared test.
Cox proportional hazards regression models were developed to evaluate the association between gender (exposure variable) and overall mortality after 30 days and one year. We performed an exploratory univariate analysis, and the covariables with clinical justification or p<0.10 were entered in the Cox regression models. The following variables were included in the models: gender, age, diabetes mellitus, previous myocardial infarction, previous angioplasty, previous coronary bypass surgery, diagnostic ECG, location of myocardial infarction, Killip class upon admission, place of FMC, time intervals, and treatment received.
The results were reported as hazard ratios (HR) with the corresponding 95% confidence interval (95%CI). All p-values were two-tailed, and statistical significance was considered for p<0.05. The SPSS® version 20.0 statistical package (SPSS Inc., Chicago, IL, USA) was used throughout.
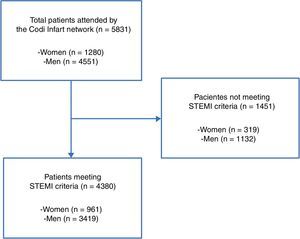
ResultsA total of 5831 patients with suspected STEMI were activated within the Codi Infart network between January 2010 and December 2011. The final analysis involved 4380 patients (75.1%). The flow chart is shown in Fig. 1.
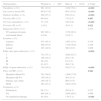
Clinical characteristics and reperfusion strategiesOf the 4380 patients analyzed, 961 (21.9%) were females and 3419 (78.1%) were males. The baseline characteristics of both groups are shown in Table 1. The women were comparatively older (69.8±13.4 vs. 60.6±12.8 years, respectively; p<0.001), with a greater prevalence of diabetes mellitus (27.1 vs. 18.1%; p<0.001) and a greater prevalence of Killip class >I upon admission (24.9 vs. 17.3%; p<0.001). Furthermore, the female group showed a lesser prevalence of previous myocardial infarction (6.9 vs. 9.7%; p=0.007), previous angioplasty (3.9 vs. 6.9%; p<0.001) and previous coronary bypass procedures (0.3 vs. 1.1%; p=0.022) compared with the male group. The place of FMC also differed significantly between the two groups. In turn, it should be mentioned that the female group comprised a greater percentage of non-reperfused patients compared with the male group (8.8 vs. 5.2%; p<0.001).
Patient baseline clinical characteristics and management.
| Characteristics | Women (n=961) | Men (n=3419) | p-Value |
|---|---|---|---|
| Population, n (%) | 961 (21.9) | 3419 (78.1) | <0.001 |
| Age (years), mean (SD) | 69.8 (13.4) | 60.6 (12.8) | <0.001 |
| Diabetes mellitus, n (%) | 260 (27.1) | 620 (18.1) | <0.001 |
| Previous MI, n (%) | 66 (6.9) | 331 (9.7) | 0.007 |
| Previous angioplasty, n (%) | 37 (3.9) | 236 (6.9) | <0.001 |
| Previous CB, n (%) | 3 (0.3) | 39 (1.1) | 0.022 |
| Diagnostic ECG, n (%) | 0.578 | ||
| ST-segment elevation | 883 (99.1) | 3179 (99.3) | |
| Left bundle block | 9 (0.9) | 24 (0.7) | |
| Location, n (%) | |||
| Anterior | 435 (45.3) | 1487 (43.5) | 0.339 |
| Inferior | 460 (47.9) | 1738 (50.8) | 0.108 |
| Lateral | 105 (10.9) | 360 (10.5) | 0.809 |
| Killip class upon admission, n (%) | <0.001 | ||
| I | 722 (75.1) | 2826 (82.7) | |
| II | 100 (10.4) | 261 (7.6) | |
| III | 46 (4.8) | 63 (1.8) | |
| IV | 93 (9.7) | 269 (7.9) | |
| Killip >I upon admission, n (%) | 239 (24.9) | 593 (17.3) | <0.001 |
| Place of FMC, n (%) | 0.042 | ||
| Hospital without PA | 383 (39.9) | 1266 (37.0) | |
| Hospital with PA | 156 (16.2) | 483 (14.1) | |
| Primary care center | 160 (16.7) | 666 (19.5) | |
| SEM | 262 (27.3) | 1004 (29.4) | |
| Treatment, n (%) | |||
| Fibrinolysis | 68 (7.1) | 285 (8.3) | 0.227 |
| PA | 808 (84.1) | 2956 (86.5) | 0.066 |
| No reperfusion therapy | 85 (8.8) | 178 (5.2) | <0.001 |
PA: primary angioplasty; SD: standard deviation; ECG: electrocardiogram; CB: coronary bypass; MI: myocardial infarction; FMC: first medical contact.
The highlighted data are statistically significant.
In comparison with the male population, the women that underwent PA showed greater delays in the following management time intervals: symptoms onset-FMC (90 vs. 74min; p<0.001), FMC-diagnostic ECG (26 vs. 22min; p<0.003), diagnostic ECG-balloon (83 vs. 80min, p=0.020), FMC-balloon (132 vs. 122min; p<0.001) and symptoms onset-balloon (total ischemia time) (236 vs. 210min; p<0.001).
The comparative data referred to the mentioned time intervals are shown in Table 2.
Medical management intervals in patients subjected to primary angioplasty.
| Medical management intervals (min), mean [IQR] | Women (n=808) | Men (n=2956) | p-Value |
|---|---|---|---|
| Population, n (%) | 808 (21.5) | 2956 (78.5) | <0.001 |
| Symptoms onset-FMC | 90 [42–180] | 74 [35–162] | <0.001 |
| FMC-diagnostic ECG | 26 [12–51] | 22 [12–45] | 0.003 |
| Diagnostic ECG-balloon | 83 [62–115] | 80 [60–110] | 0.020 |
| FMC-balloon | 132 [99–183] | 122 [92–170] | <0.001 |
| Symptoms onset-balloon (total ischemia time) | 236 [169–360] | 210 [150–315] | <0.001 |
ECG: electrocardiogram; FMC: first medical contact; IQR: interquartile range.
The highlighted data are statistically significant.
The data comparing the clinical events between the groups are shown in Table 3. Overall, women presented a greater percentage of in-hospital complications (22.2 vs. 19.0%; p=0.031). In particular, the female group showed a greater presence of atrioventricular block (6.1 vs. 3.7%; p=0.001), atrial fibrillation (3.4 vs. 2.2%; p=0.032) and cardiogenic shock (9.7 vs. 7.9%; p<0.001) than the male group. Furthermore, women had a greater overall in-hospital mortality rate (4.8 vs. 2.6%; p=0.001), overall 30-day mortality rate (9.1 vs. 4.5%; p<0.001) and overall one-year mortality rate (14.0 vs. 8.3%; p<0.001).
Clinical events.
| Women (n=961) | Men (n=3419) | p-Value | |
|---|---|---|---|
| Population, n (%) | 961 (21.9) | 3419 (78.1) | <0.001 |
| In-hospital complications | 198 (20.6) | 594 (17.4) | 0.031 |
| Ventricular fibrillation | 26 (2.7) | 106 (3.1) | 0.594 |
| Ventricular tachycardia | 27 (2.8) | 81 (2.4) | 0.412 |
| Asystolia | 18 (1.9) | 44 (1.3) | 0.215 |
| Complete atrioventricular block | 59 (6.1) | 126 (3.7) | 0.001 |
| Atrial fibrillation | 33 (3.4) | 74 (2.2) | 0.032 |
| Cardiogenic shock | 93 (9.7) | 269 (7.9) | <0.001 |
| Mechanical ventilation | 46 (4.8) | 141 (4.1) | 0.367 |
| Overall mortality | |||
| In-hospital mortality | 46 (4.8) | 89 (2.6) | 0.001 |
| Mortality after 30 days | 87 (9.1) | 154 (4.5) | <0.001 |
| Mortality after one year | 135 (14.0) | 285 (8.3) | <0.001 |
The highlighted data are statistically significant.
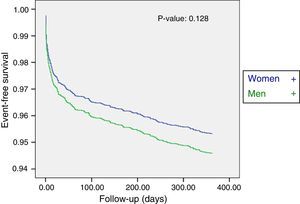
However, following multivariate adjustment of the data, no gender differences were observed in the overall 30-day mortality rate (hazard ratio [HR] adjusted to 30 days [95%CI]: 1.25 [0.94–1.65]; p=0.123; HR adjusted to one year [95%CI]: 0.88 [0.69–1.07]; p=0.128). The Cox regression curve for mortality due to all causes after one year is shown in Fig. 2.
DiscussionThe main conclusions of our study were: (1) women with STEMI had a comparatively worse risk profile and a greater proportion of in-hospital complications and overall mortality; (2) women received less reperfusion treatment and suffered longer delays in medical assistance compared with men; and (3) after adjusting for confounding factors, women and men showed similar rates referred to mortality due to all causes after both 30 days and one year of follow-up.
STEMI management network and gender gap in medical careThe implementation of strategies designed to facilitate STEMI patient access to the medical care system has been shown to reduce delays in percutaneous coronary intervention,16,17 lessen the mortality rate,18 and lower the global hospital costs.19
Despite the improvements in medical care resulting from introduction of the STEMI management networks, the gender gap in patient management is seen to persist. Indeed, in our study women suffered greater delays and underwent a lesser proportion of revascularization procedures than men. Previous studies have shown that women suffer greater delays in medical assistance, as evidenced by longer door-balloon times and longer total ischemia times.20–23 By allowing ECG recordings in the home, out-hospital activation of hemodynamic systems and direct patient transfer to the Hemodynamics Unit via the SEM, the STEMI management networks have been associated to lesser delays in medical care and lower mortality rates.24,25
Following implantation of the Codi Infart network, the female population still shows longer management intervals and lesser reperfusion rates than the male population. This gender gap in time intervals and reperfusion therapy could be explained by gender differences in the clinical presentation and physiopathology of STEMI. Such differences should be considered when evaluating and treating women with suspected of confirmed STEMI, since this is a population characterized by great diagnostic and therapeutic complexity.26
The comparatively older age and greater prevalence of diabetes mellitus among the women in our study is associated to a greater presence of atypical symptoms that can lead to patient delays in contacting the medical care system (patient delay), as well as to errors in the clinical assessment of STEMI which in turn result in delays once the patients have already entered the system (system delay).1,20–23 These differences were evidenced by the fact that women showed greater delays in all the evaluated time intervals compared with the male group.
It also should be commented that although PA is currently the preferred reperfusion strategy in STEMI, particularly in women, because PA is able to reduce bleeding complications in females to a greater extent than in males,9,27–29 the gender difference in reperfusion therapy persists in our network – as reflected by the greater percentage of women that did not receive therapy versus their male counterparts (8.8 vs. 5.2%; p<0.001). The data obtained in our study are unable to offer an in-depth explanation for this difference, though it could be mediated in part by gender-related physiopathological variations in STEMI such as the greater incidence of spontaneous coronary dissection and coronary spasm in the female population.1,26,27
STEMI management network and outcome in womenThe studies carried out in the thrombolysis era, such as the GUSTO IIB trial,28 have shown women to experience a greater proportion of in-hospital complications and mortality after 30 days compared with men. The mentioned study also demonstrated an interaction between mortality and the female gender following the multivariate adjustment analysis.28 These data were subsequently confirmed by other registries during the 1990s and opening years of the XXI century in Spain.29,30
The studies published following the generalized adoption of PA in routine clinical practice6,7,27,31 also showed women to suffer greater in-hospital mortality than men. This could be explained by the differences in reperfusion rate and the worse risk profile of the women with STEMI in those studies.
Following their multivariate analysis, Lawesson et al.32 found the one-year mortality rate to be 8% lower in women than in men. This was the first study in the context of STEMI to show women to suffer greater in-hospital mortality but lesser long-term mortality than men. Our study did not identify differences in the overall mortality rate after 30 days and one year between the two genders after adjusting for the confounding factors. The results obtained indicate that the implantation of STEMI management networks has contributed to equalize the middle- and long-term prognosis in males and females, and suggest that if both genders could receive reperfusion therapy and medical management intervals in the same way, the long-term prognosis could be even better in women than in men.
Study limitationsA first limitation of this study is the fact that it is a retrospective analysis of subgroups from a prospective database of the Servei Català de la Salut (CatSalut). Nevertheless, it is the largest Spanish study to date on the role of patient gender in patients attended by a specific STEMI management network. A second limitation is that the outcome after one year was only assessed on the basis of mortality due to all causes and other prognostic assessment parameters such as cardiac mortality, myocardial infarction or the need for further revascularization. A third limitation is the fact that a non-negligible percentage of patients did not receive reperfusion therapy and, as commented above, we do not have concrete data capable of explaining this observation – since the collection of such information was not contemplated when the registry was designed. A fourth limitations is the fact that the data are referred to the Catalan population, representing a Mediterranean area, and therefore cannot be fully extrapolated to other geographical settings. Lastly, we do not have information on the extent of coronary disease (e.g., the number of diseased vessels) or on the drug treatment or interventional cardiological management provided in the course of patient follow-up, and which could also influence the extrapolation of our results.
ConclusionsThe female population attended by our regional STEMI management network had a worse risk profile, received less reperfusion therapy and showed greater delays in medical management than the male population. However, following the multivariate adjustment analysis, the clinical outcomes after 30 days and one year in the female population were seen to be similar to those of their male counterparts.
Financial supportNone.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández-Rodríguez D, Regueiro A, Cevallos J, Bosch X, Freixa X, Trilla M, et al. Brecha de género en los cuidados médicos en las redes de atención al infarto agudo de miocardio con elevación del segmento ST: hallazgos de la red catalana Codi Infart. Med Intensiva. 2017;41:70–77.