We present the case of a 28-year-old woman with no relevant past medical history who visited the ER with a 1-week history fever of 39 °C after coming back from a trip to the Azores. Since symptom onset, she started developing an ulcerative lesion with an erythematous halo around the periphery on her back, which progressed to a necrotic scab. Despite initial treatment with cefadroxil and antipyretics, she continued to have a high fever along with abdominal pain. Upon arrival at the ER, a generally painful abdomen and hypotension were noted. Emergency lab tests revealed acute renal failure (creatinine levels of 1.83 mg/dL), lymphopenia (100), thrombocytopenia (140,000), elevated transaminases with aspartate aminotransferase (AST) 125 U/L and alanine aminotransferase (ALT) 93 U/L, and an increase in C-reactive protein (CRP) 385 mg/L. An abdominal ultrasound revealed the presence of hepatosplenomegaly as the only finding. Microbiological screening was initiated, including viral and bacterial serologies, Plasmodium antigen testing, and cultures from the wound exudate and blood; the patient was admitted to the intensive care unit (ICU) for monitoring and further evaluation.
The initial course of the disease was unfavorable, with high fever, abdominal pain, and progressive respiratory deterioration, requiring high-flow nasal oxygen therapy. Chest X-ray at admission revealed interstitial infiltrates with basal consolidations. Empirical coverage with ceftriaxone, cloxacillin, and doxycycline was initiated while awaiting results and observing the patient’s progression. A few hours after admission, the patient started developing overt respiratory failure requiring urgent orotracheal intubation, with hypoxemia refractory to alveolar recruitment maneuvers, and progressive hemodynamic instability in refractory vasoplegic shock treated with norepinephrine, vasopressin, and corticosteroids; metabolic acidosis with hyperlactatemia and oliguria. In the presence of multiple organ dysfunction (Sequential Organ Failure Assessment score, SOFA 12), empirical coverage was expanded to include linezolid and meropenem in addition to doxycycline, and continuous renal replacement therapy—hemodiafiltration—was initiated with regional citrate anticoagulation. Aferwards, the Microbiology Department informed us of the isolation of Chromobacterium violaceum in blood cultures, leading to the addition of levofloxacin after reviewing the literature, given the resistance profile of this microorganism.
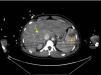
Gradually, the patient stabilized both from a respiratory and hemodynamic perspective, allowing for her transfer for further evaluation using computed tomography (CT), which revealed multiple pulmonary abscesses (Fig. 1), 2 liver abscesses, and splenic infarction (Fig. 2)1; no findings were noted in the brain.
Twenty-four hours after admission, an antibiogram of Chromobacterium violaceum was obtained, showing sensitivity to carbapenems and quinolones. The same pathogen was isolated in wound exudate and in tracheal aspirate. Plasma levels of meropenem were monitored. Both trough and 50% administration levels fell within the therapeutic range for a minimum inhibitory concentration (MIC) of 0.12.
The clinical course over the following days was favorable, with vasopressor support being withdrawn, and successful extubation; in fact, the patient no longer required oxygen therapy, and renal failure resolved at the time of her ICU discharge. She was, then, transferred to the general ward 12 days later.
Although Chromobacterium violaceum-related infections in humans are rare, they are reported to have mortality rates of up to 65%. This is an atypical facultative anaerobic Gram-negative bacillus, an uncommon pathogen with <300 cases reported in the literature. Classically, it has been considered endemic to tropical and subtropical regions; infection by this bacterium typically occurs after exposure of wounds to contaminated water or soil.2
It typically presents with skin or soft tissue infections that can be associated with pulmonary and liver abscesses, meningitis, osteomyelitis, endocarditis, and can rapidly progress to multiple organ dysfunction with high lethality.3,4
Although the optimal antimicrobial treatment and its duration are not well established, management can be challenging since this microorganism is known for its resistance to many routine antimicrobials such as penicillins and cephalosporins.5 It is generally susceptible to fluoroquinolones, chloramphenicol, tetracycline, trimethoprim/sulfamethoxazole, carbapenems, and aminoglycosides.
In conclusion, in the management of sepsis caused by Chromobacterium violaceum, clinical suspicion, early diagnosis, and prompt and appropriate treatment are key to ensuring patient survival. These are unusual infections that require a high index of suspicion, especially if the patient has a history of outdoor activities such as contact with stagnant water, rivers, lakes, or wounds and/or lesions that could serve as the entry point.6