Ventilator associated pneumonia (VAP) is the leading nosocomial infection in Intensive Care. It is associated with increased ICU and hospital stay, an increased use of antibiotics, and greater hospital costs. The recently launched Pneumonia Zero project (NZ) undoubtedly constitutes a challenge for professionals in the ICU, and has been designed to reduce the high incidence rates described. It is necessary to establish the true incidence, and whether the latter is influenced by the diagnostic method employed.
The lack of a reference standard for the microbiological diagnosis of VAP has generated controversy over the diagnostic algorithms to be used, with the distinction of two strategies: a noninvasive or clinical strategy based on upper respiratory tract cultures, and an invasive method based on the use of quantitative cultures of samples from the lower respiratory tract obtained by bronchoscopic techniques. Despite the recommendations of scientific societies, which do not justify the use of qualitative tracheal aspirates in the microbiological diagnosis of VAP, this method is still routinely used.
This study underscores the need to stop using qualitative tracheal aspirates as a routine diagnostic method for VAP, recommending the use of bronchoscopic techniques or quantitative tracheal aspirates.
La neumonía asociada a ventilación mecánica (NAVM) es la principal infección nosocomial acontecida en cuidados intensivos, se asocia a un aumento de la estancia en la unidad de cuidados intensivos (UCI) y hospitalaria, a un mayor consumo de antibióticos, y del coste hospitalario. El proyecto Neumonía Zero (NZ), recientemente iniciado, es sin duda un reto para los profesionales de las UCI dirigido a disminuir las altas tasas de incidencia descritas. Es necesario aclarar de qué incidencia real partimos y si el método diagnóstico utilizado influye en esta.
La falta de un patrón de referencia para el diagnóstico microbiológico de NAVM ha suscitado una controversia respecto a los algoritmos diagnósticos a seguir, distinguiéndose dos estrategias que coexisten: la «no invasiva» o «clínica», basada en cultivos de vías respiratorias altas y la «invasiva», fundamentada en el uso de cultivos cuantitativos de muestras obtenidas del tracto respiratorio inferior mediante técnicas broncoscópicas. A pesar de las recomendaciones de las sociedades científicas, que no justifican la utilización del aspirado traqueal cualitativo para el diagnóstico microbiológico de la NAVM, este sigue siendo un método habitualmente utilizado. El presente artículo incide en la necesidad de que el aspirado traqueal cualitativo deje de ser un método de diagnóstico rutinario para la NAVM recomendando el uso de técnicas broncoscópicas o el aspirado traqueal cuantitativo.
Nosocomial infections (NIs) are infections that develop in relation to healthcare, and are not a direct consequence of the background disease for which the patient is receiving treatment. Urinary tract infections associated to bladder catheterization, skin and soft tissue infections following surgical procedures, or mediastinitis after heart surgery, are examples of NIs.
Intensive Care Units (ICUs) represent a favorable scenario for the development of infections of this kind, since seriously ill patients are more susceptible to NIs. Invasive procedures are typically carried out in the ICU that adversely affect the local defense barriers of the body, and the patients admitted to these Units have often been previously exposed to antibiotics and are therefore susceptible to the development of bacterial resistances. In the Intensive Care setting, ventilator associated pneumonia (VAP) is the most prevalent infectious problem,1–3 ahead of catheter-related or urinary tract infections. Moreover, VAP is distinguished from the latter by its high associated mortality, particularly when caused by multiresistant organisms.4,5 Lastly, it must be underscored that VAP is associated with a longer stay in the ICU and in hospital,6,7 increased antibiotic use,8 and greater hospital costs.9
The recently launched Pneumonia Zero (PZ) project undoubtedly represents a challenge for ICU professionals. Following the satisfactory experience gained with the Bacteremia Zero (BZ) project, we now face a new battle against the main type of infection found in ICUs—though a series of aspects need to be clarified: What is the true starting incidence of the infection? Does the diagnostic technique used exert an influence upon the incidence? And in this context, what diagnostic method should be used to assess the efficacy of the adopted preventive measures?
The ENVIN-HELICS registry: What is the true starting incidence of the infection?The existence of a nosocomial infection vigilance system is undoubtedly the result of years of work on the part of the Infectious Diseases Work Group of the SEMICYUC (GTEI-SEMICYUC). The ENVIN-HELICS registry has become consolidated in recent years as one of the main ICU nosocomial infections registries. It has grown from an initial total of 1884 patients in its first year in 1994 to 16,950 cases in the last report corresponding to the year 2010. This undoubtedly reflects the concern among intensivists regarding the vigilance and control of NIs, and has contributed to assess and improve the quality of healthcare by establishing a map or profile of the true situation in our ICUs year by year, with the ultimate aim of incorporating preventive measures for improving the safety of critically ill patients.
The “cultural” change of understanding that NIs are not simply the price to pay for admission to Intensive Care, as an unavoidable risk or problem inherent to medical care, has become manifest in the BZ project. It has been shown that the adoption of a series of measures not only contributes to reduce the incidence of these infections, but moreover has given rise to increased awareness of the importance of clinical safety—establishing concrete objectives, identifying errors or inadequate practices, and defining plans for improvement. The launching in 2011 of the PZ project represents a further challenge that is fully justified and constitutes an ethical obligation destined to improve healthcare in search of excellence.
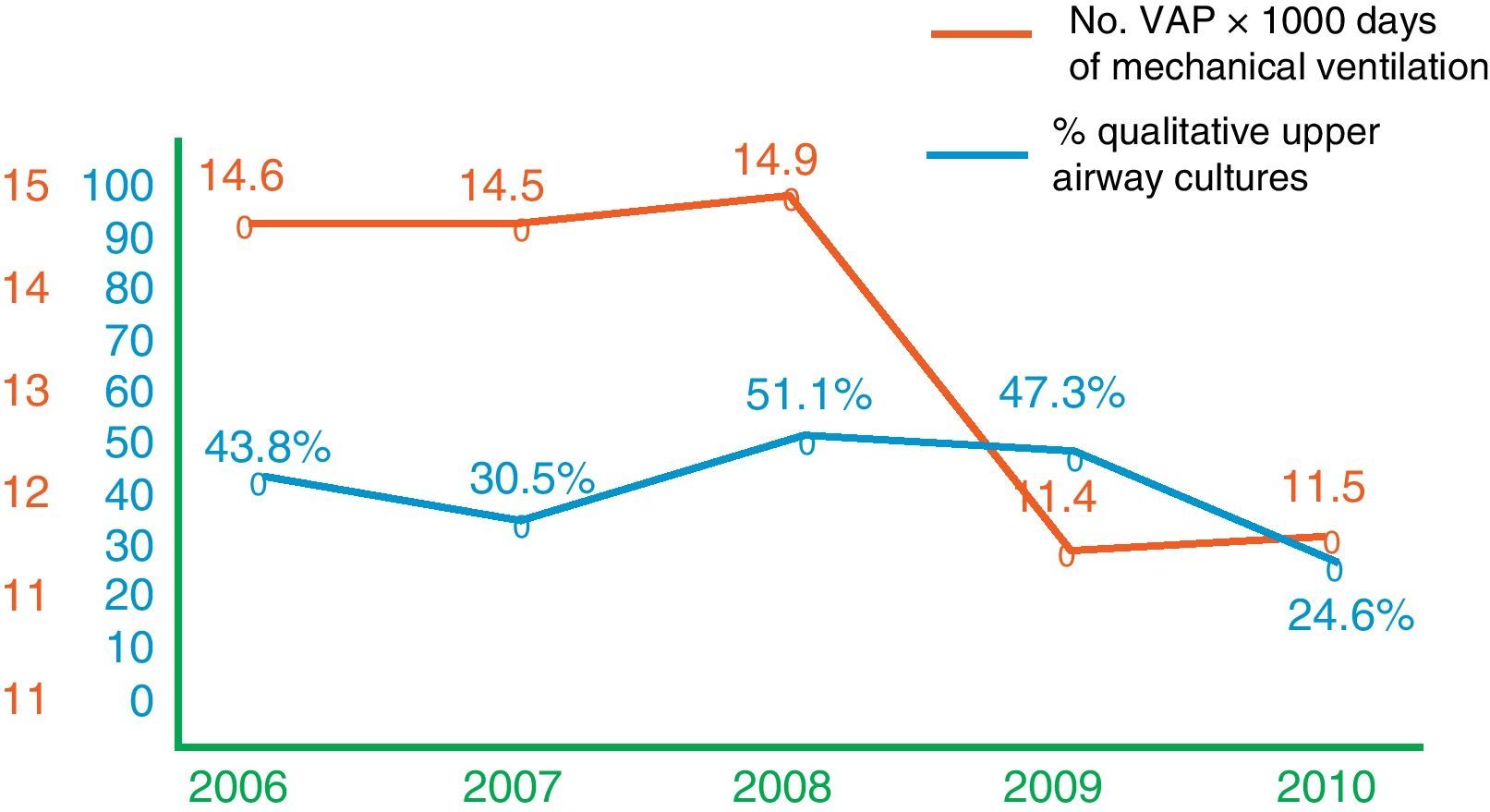
On examining the last few years (Fig. 1), we see that after the decrease in the incidence of VAP recorded in the year 2009, the figures have remained stable. However, the procedures used for the microbiological diagnosis of VAP have varied. In this sense, in the year in which the highest incidence of NIs was recorded, qualitative cultures of upper airway samples were the most frequently used diagnostic technique (51.1%).
The ongoing debate: the clinical versus invasive strategyOver a decade ago, Niederman et al.10 and Chastre et al.11 started a debate on the microbiological diagnosis of VAP that persists to this day.12,13 This lack of a reference standard for the microbiological diagnosis of VAP has given rise to controversy regarding which diagnostic algorithms to use. In this context, there are two coexisting strategies: “noninvasive” or “clinical”, based on the culture of upper airway samples,14 and “invasive”, based on the use of quantitative cultures of lower respiratory tract samples usually obtained by bronchoscopy.15–17 The two randomized clinical trials that have compared these strategies, with the inclusion of many patients and an important impact upon the scientific community, have yielded conflicting results.14,18 Although the objectives of both studies appeared to be similar, there were major differences in their design that can explain the observed lack of agreement. In the study published by Fagon et al.,14 treatment was guided by the results of gram staining. Accordingly, if germ isolation proved negative and there were no signs of sepsis, treatment was suspended. In the other study,18 treatment was started with broad-spectrum antibiotics in all patients, regardless of whether they were at risk of infection caused by multiresistant organisms or not. Another important difference between the two studies was the patient population involved, since the Canadian trial18 excluded individuals with immune deficiencies, chronic diseases, treatment with carbapenem or quinolones, and colonization by microorganisms resistant to antibiotic treatment. The profile of these excluded individuals, representing over one-third of all the patients in the study, coincides with the profile of most subjects admitted to the ICU with clinically suspected VAP, and this is possibly the patient subpopulation that would benefit most from the invasive strategy—though no study has confirmed this to date.
Although some authorities have suggested an end to the debate, it seems logical to consider that a sample obtained from the lower respiratory tract with guidance toward the affected zone offers greater quality than a tracheal sample. In any case, and although it may seem overly ambitious, we can debate whether one strategy or the other truly has impact upon mortality or not. In this context, although the clinical strategy has not been shown to be inferior to the invasive strategy in relation to the patient prognosis, it has not been able to improve upon the established advantages of the bronchoscopic techniques: greater confidence on the part of the clinician, rational antibiotic use (which can contribute to avoid the development of bacterial resistances), and the importance of a negative reading obtained from a quality respiratory sample in redirecting the search for other infectious foci—particularly in patients without previous antibiotic treatment.
“ZERO” qualitative tracheal aspirateAccording to the ENVIN-HELICS registry, up until the year 2009 qualitative tracheal aspiration was the microbiological technique most widely used to diagnose VAP in Spanish ICUs (47.3% of the cases registered that year). This is probably attributable to the fact that tracheal aspiration is rapid, simple and causes few complications. In coincidence with these observations, a study on the diagnosis of VAP in Andalusia found qualitative tracheal aspiration to be the most frequently used technique (42.8%).19 The analysis carried out by the pneumonia work group of the European Society of Intensive Care Medicine (EU-VAP/CAP Study Group) in 2009, involving over 20 ICUs in 9 countries and the evaluation of 2436 patients with 827 cases of pneumonia, likewise found qualitative tracheal aspiration to be the microbiological diagnostic method used in 46.2% of the cases.20
A number of factors can explain this situation, which has persisted for years. Firstly, the lack of a reference standard has given rise to great clinical variability in dealing with the diagnosis of VAP. Such variability can be minimized through training programs, emphasizing the fact that qualitative tracheal aspiration is not recommended, regardless of the debate referred to the use of invasive or noninvasive techniques. In this sense, for example, if we compare the mortality figures with those of other infectious diseases found in the ICU, such as severe acute meningitis, it is surprising that despite the similarities between these processes, the attitude toward the microbiological samples differs: cerebrospinal fluid is rapidly processed and immediate information is requested from the microbiologist, while the approach tends to be more contemplative in the case of a tracheal aspirate or bronchoalveolar lavage. We feel that a more active attitude is needed here; coordination between the clinician (the intensivist in this case) and the microbiologist is essential, with a view to insisting on the need for quantitative processing of the sample. The decrease recorded in Spain regarding qualitative aspirate utilization in the registry corresponding to 2010 is promising, and reflects greater adherence to the recommendations of the main scientific societies. Independently of the recommendation of the American Thoracic Society (ATS),4 which points to a reduction in mortality after 14 days with the “invasive” diagnostic strategy versus the “clinical” strategy, supported by grade I evidence, and based on the multicenter clinical trial published by Fagon et al.,14 it is important to underscore the recommendations of both the ATS and the SEMICYUC4,21 referred to the use of qualitative tracheal aspiration. With grade II evidence, it is recommended that lower respiratory tract samples should be obtained in all patients with clinically suspected VAP, and that these samples may be tracheal aspirate, bronchoalveolar lavage (BAL) or protected bronchial brush. Based on the maximum evidence (grade I), both the ATS and the Spanish Society of Intensive Care Medicine advise against the routine use of qualitative tracheal aspiration for the microbiological diagnosis of VAP.4,21 The main argument in this sense is that such samples are unlikely to allow differentiation between colonization and infection, since the airways of most patients on mechanical ventilation are colonized by potentially pathogenic microorganisms, and we may be risking the over-diagnosis of cases of pneumonia which in fact correspond to tracheal colonization or tracheobronchitis.
Bronchoscopic methods represented 23.3% in the European study,20 and did not exceed 10% in the ENVIN-HELICS registry of 2010. Probably the non-availability of fibrobronchoscopy in some ICUs, the lack of experienced personnel and the need for prior training are some of the reasons for such limited utilization—though the technique is actually simple, with few complications, and can be performed at the patient bedside.22
Influence of the microbiological diagnostic method upon incidenceOn analyzing the incidence of VAP, the published results are seen to be very heterogeneous. This is probably due to the existing clinical variability, conditioned by the different patient populations and isolated pathogens in each study, the different types of ICUs involved, and the mentioned lack of consensus regarding the microbiological diagnosis. The interval found in the literature varies greatly from 5% or 9% using invasive diagnostic methods23,24 to 41% or 67% when based on clinical criteria.25,26 In 53 patients with clinically suspected pneumonia, Morris et al.27 analyzed the influence of qualitative and quantitative aspiration, and bronchoalveolar lavage, upon the incidence of the disorder—important differences being detected depending on whether sample processing in the laboratory was qualitative or quantitative.
Final considerationsThe possibility of error in diagnosing VAP is not without a price for both the patient and the healthcare system. The risk of overdiagnosing pneumonias which in fact constitute colonization implies unnecessary antibiotic use—with the consequent drug cost increments,28 an increased risk of antibiotic toxicity, and the appearance of bacterial resistances.
There is no doubt that quantitative sample processing offers clinicians a greater degree of confidence in relation to patient management. However, we must abandon the concept of “positive culture” and “negative culture” and request sample quantification. The described cutoff points accepted by the scientific community lack a validating reference standard; as a result, they must not be viewed isolatedly but in a clinical context—taking into account previous antibiotic treatment, days on mechanical ventilation, the microorganism, the sample obtained, the medical history, and the immune condition of the patient.
The described variability in the diagnostic management of VAP implies differences in the assignment of resources, and therefore the possibility that the offered diagnosis and treatment may be suboptimal, depending on the setting involved. Consensus on the diagnostic algorithm is therefore needed, assuming the disagreement between those who defend the clinical strategy and those who prefer the invasive approach—but accepting the fact that both strategies can coexist, provided they coincide on the need for recommending quantitative respiratory sample cultures. Quantitative tracheal aspiration is a reasonable alternative that has been shown to offer sensitivity and specificity performances similar to those of the bronchoscopic techniques.29 The clinical trials that have compared the two strategies have concluded that there are no differences between them in terms of prognosis and mortality, though antibiotic use is effectively greater with the invasive strategy.30 In relation to the last issue raised in “Introduction” section, it is necessary to clarify that the efficacy of the preventive measures cannot be comparable among hospitals as long as the diagnostic approach remains variable. In the current scenario, the incidence of VAP cannot be used as a comparative measure among different ICUs, or as a prognostic quality predictor in critical patients subjected to ventilation,31,32 in the way of days on mechanical ventilation, stay in the ICU, or mortality. It is to be expected that the incidence of microbiologically confirmed VAP in hospitals that exclusively use endoscopic techniques is lower than in those centers that do not use these procedures. It therefore seems prudent to propose a differentiated measure of the rates according to whether use is made of one technique or other, in order to avoid transference bias and afford a true measure of the effect of the preventive actions taken.
The title to this article emphasizes the need to eliminate qualitative tracheal aspiration as a routine diagnostic method in VAP—limiting its use to those ICUs in which quantitative diagnostic procedures are not possible.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Estella A, Álvarez-Lerma F. ¿Debemos mejorar el diagnóstico de la neumonía asociada a ventilación mecánica? Med Intensiva. 2011;35:578–82.