A steadily increasing number of patients survive their stay in the Intensive Care Unit (ICU), and a significant percentage become chronic cases. Patient post-intensive care syndrome (PICS-P) is a recently described condition that affects an important number of patients (30–50%). It encompasses the physical (mainly respiratory and neuromuscular), cognitive (memory and attention) and psychological sequelae (depression, anxiety, stress and/or posttraumatic stress syndrome) at discharge from the ICU, and which have a negative impact upon patient quality of life.1
This syndrome also affects the family of the patient (PICS-F). In effect, the patient relatives constitute a vulnerable and often forgotten group of individuals that nevertheless suffer negative physical, psychological and social effects that worsen their quality of life.2
The relatives of critical patients often suffer anxiety (70%), depression (35%) and posttraumatic stress (35%) that can persist for years. In a recent study, 16% of the relatives had not reduced their level of depression one year after patient discharge.3 Furthermore, they suffer physical symptoms such as fatigue and behavioral alterations that pose a risk for health, such as sleep disturbances, insufficient rest, lack of physical exercise, disrupted eating habits, and a lack of adherence to medical treatment. The burden of caring for a postcritical patient moreover affects personal aspects such as life plans and social and professional relationships, and favors the generation of family conflicts.4
The concept of person-centered medicine recognizes the needs not only of the patient but also of the family during critical illness.
Although several factors have been related to PICS-F,5 few studies have specifically addressed this syndrome to date. The study published by Torres et al.6 in the journal Medicina Intensiva was carried out in a Portuguese medical-surgical ICU and offers relevant information in this regard. The authors evaluated the impact of the different components of PICS-P upon caregiver burden. Among the 186 relatives interviewed, the burden was found to be low in 34.5% of the cases and moderate-high in 15.5%. The main finding of the study was that the presence of psychological components of PICS-P (anxiety and depression) three months after discharge from the ICU had a negative impact upon caregiver burden. Neither the patient physical sequelae nor other variables studied (age, gender, SAPS II score or ICU stay) had a significant impact upon caregiver burden. Among the limitations of the study, the authors mentioned its single center design, and the fact that the sample size may have been too small to allow extrapolation of the results. Likewise, the lack of anonymity might have influenced sincerity in answering, and certain family-related variables considered in other studies were not examined. Lastly, the 31% of cases lost to follow-up could have altered the results.
Despite the interest and contributions of the study, which are particularly relevant in demonstrating the need to include the family in critical patient care and to offer them support over time, important gaps remain when it comes to defining the best strategy for dealing with these syndromes. Furthermore, validated tools are needed to allow homogeneous comparison of the results obtained.
The strategies designed to detect and prevent PICS require a structured and multidisciplinary approach implemented early after admission of the critical patient. The measures adopted must allow us to detect risk factors for the appearance of sequelae not only in the patient but also in the family. Many initiatives and recommendations have been defined to reduce the appearance of PICS-P in all its dimensions, and they are gradually being incorporated to the ICU as daily objectives. However, few strategies have demonstrated scientific evidence in reducing the negative impact of admission to the ICU upon the family, and even fewer Units have systematically incorporated such strategies to daily care.
The concept of “ICU Liberation”7 constitutes a quality improvement initiative based on implementation of the ABCDEF series of measures, with high scientific evidence, and which when globally applied has been found to improve the outcomes and reduce the appearance of PICS. The control of pain, adequate sedation, the management of delirium, keeping the patients awake and under spontaneous breathing, early mobilization, and implication and participation of the family have been shown to lessen the impact not only in terms of patient survival but also as regards the sequelae for both the patients and their relatives at discharge from the ICU. The incorporation of these measures to clinical practice requires a change in culture and philosophy, adopting an integral approach to the patient and family in all dimensions, and ensuring optimum teamwork on the part of all the professionals implicated in critical patient care. If we really want to improve the outcomes, we must be able to recognize these needs. The success of some initiatives8 should help overcome reluctance to change, adopting an open view allowing the gradual but effective reduction of avoidable damage associated to critical patient care.
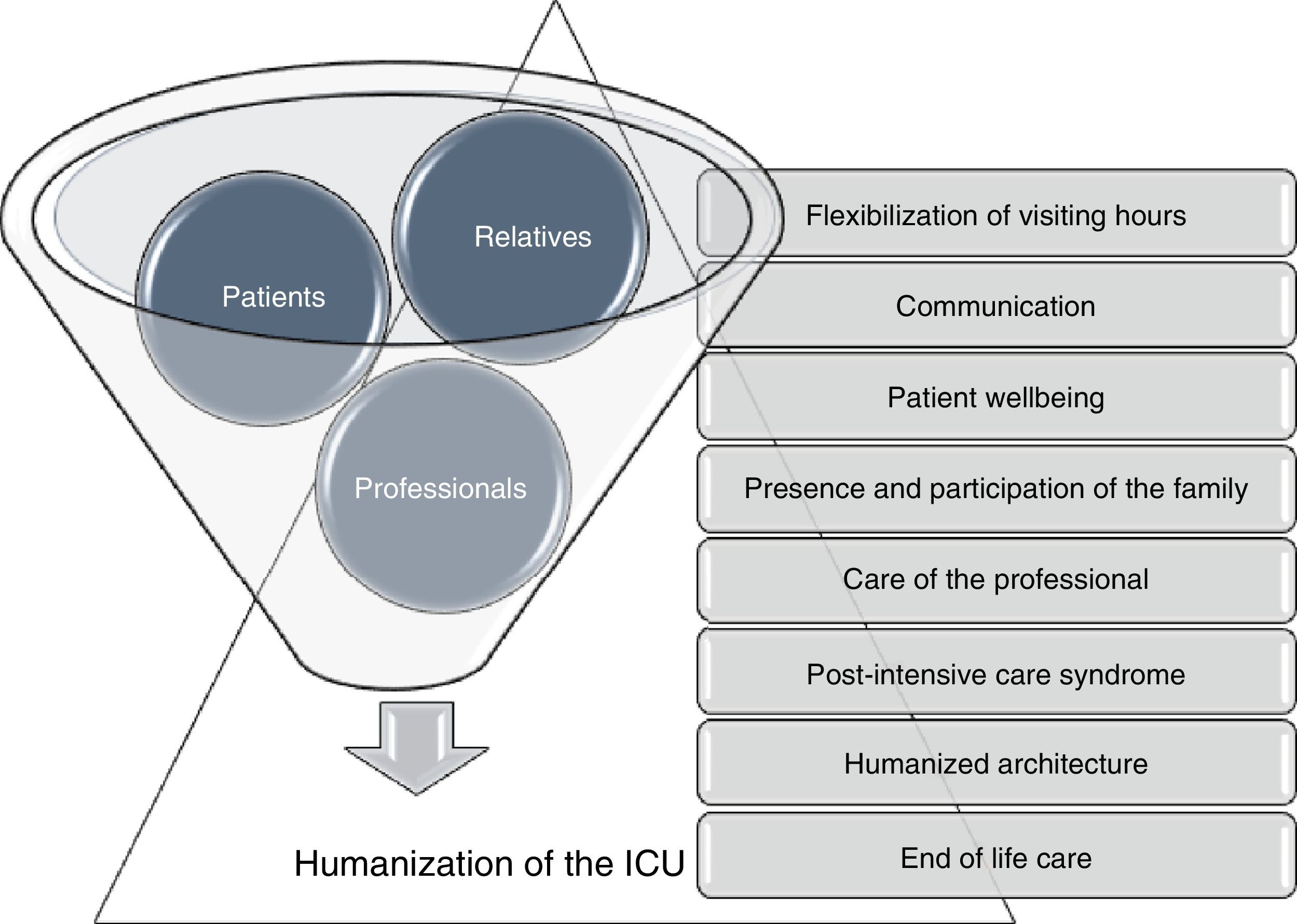
The humanization of intensive care, which recently has gained relevance as a consequence of different projects such as the HU-CI initiative,9 favors specific actions destined to reduce this syndrome through the strategic lines included in the Humanization Plan for ICUs in the Community of Madrid (Spain) (Fig. 1). The creation of monitoring units following ICU discharge will facilitate the continuity of management of the process and evaluation of the impact of these interventions. Intensive Care Units should consider expanding their range of services, offering this resource on a multidisciplinary basis with the aim of reintegrating the patients and their families to society after the critical episode, with the minimum physical, cognitive and psychological sequelae possible.10
Dirección General de Coordinación de la Atención al Ciudadano y Humanización de la Asistencia Sanitaria. Plan de Humanización de la Asistencia Sanitaria 2016–2019. Líneas estratégicas del Plan de Humanización de las Unidades de Cuidados Intensivos (UCI) de la Comunidad de Madrid. Available from: General Board of Citizen Care Coordination and Healthcare Humanization (Dirección General de Coordinación de la Atención al Ciudadano y Humanización de la Asistencia Sanitaria). Healthcare Humanization Plan 2016–2019. Strategic Lines of the Humanization Plan for Intensive Care Units (ICUs) in the Community of Madrid. Accessible at: http://www.madrid.org/bvirtual/BVCM017902.pdf.
The relatives and caregivers of patients that survive their ICU stay constitute a crucial element of support for these individuals, and moreover absorb an important economical cost for the health system. We therefore can and must make sure that these people are not forgotten.
Please cite this article as: Martín Delgado MC, García de Lorenzo y Mateos A. Sobrevivir a las unidades de cuidados intensivos mirando a través de los ojos de la familia. Med Intensiva. 2017;41:451–453.