To evaluate patient post-intensive care syndrome (PICS-P) and caregiver burden 3 months after discharge from the Intensive Care Unit (ICU) and determine the impact of different components of PICS-P upon caregiver burden.
DesignA prospective observational study was conducted over 26 months (January 2013–February 2015).
SettingMedical-surgical ICU and follow-up consultation in Portugal.
Patients or participantsPatients discharged after a minimum of 2 days in the ICU. Caregiver inclusion criteria: not paid, written and spoken Portuguese, and agreement to participate in the study.
Main variables of interestIn ICU: Patient gender, age, severity of illness (SAPS II) and length of ICU stay. At 3 months caregiver burden, physical (reduced mobility, weakness acquired in the ICU) and psychological components of PICS (anxiety, depression, post-traumatic stress disorder).
ResultsA total of 168 caregivers completed the survey (response rate of 69%). A low degree of overburden was reported by 34.5% of caregivers, while 15.5% showed moderate to high levels of overburden.
Patient anxiety and depression 3 months after ICU discharge significantly influenced the presence of caregiver burden (p=0.030 vs p=0.008).
When physical components of PICS-P were evaluated, no influence on caregiver burden was observed. Patient demographics, severity of illness and length of stay also failed to influence caregiver burden.
ConclusionsThe presence of psychological components of PICS-P 3 months after ICU seems to have a negative impact upon caregiver burden. On the other hand, physical problems showed no important impact upon caregiver overburden.
Caracterizar el síndrome poscuidados intensivos de los pacientes (PICS-P) y la sobrecarga de los cuidadores a los 3 meses del alta de la Unidad de Cuidados Intensivos (UCI). Averiguar cómo la sobrecarga es influida por los diferentes componentes del PICS-P.
DiseñoEstudio prospectivo observacional de 26 meses (enero de 2013-febrero de 2015).
ÁmbitoUCI médico-quirúrgica y consulta de seguimiento en Portugal.
Pacientes o participantesPacientes dados de alta después de 2 o más días en la UCI. Criterios de inclusión de los cuidadores: no cobrar, leer y hablar portugués y aceptar participar en el estudio.
Principales variables de interésEn la UCI: género, edad, gravedad de la enfermedad (SAPS II) y estancia en la UCI. A los 3 meses: sobrecarga del cuidador; componentes físicos (reducción de la movilidad, debilidad adquirida en la UCI) y psíquicos (ansiedad, depresión, síndrome de estrés postraumático) del PICS-P.
ResultadosUn total de 168 cuidadores respondieron al cuestionario de sobrecarga (tasa de respuesta del 69%). El nivel de sobrecarga era bajo en el 34,5% de los casos y moderado a alto en el 15,5%. A los 3 meses, la presencia de ansiedad y depresión en los pacientes influyó de forma significativa en la sobrecarga de los cuidadores (p=0,030 y p=0,008, respectivamente). No se encontró ninguna influencia de los componentes físicos del PICS-P, la edad, el género, el SAPS II o la estancia en UCI sobre la sobrecarga.
ConclusionesLa presencia de componentes psicológicos de PICS-P a los tres meses parece influir de forma negativa en el nivel de sobrecarga de los cuidadores. Los problemas físicos parecen no tener impacto sobre dicha sobrecarga.
Nowadays an increasing number of patients survive critical illness after the tremendous advances in medical science and healthcare. Although survival is clearly an important and crucial outcome, the clinical condition after survival is also fundamental. Post Intensive Care Syndrome (PICS) is a multidimensional problem experienced after an Intensive Care Unit (ICU) stay, which can persist for several years.1 PICS is described both for the patient (PICS-P) and their family (PICS-F).1–4,6,7
PICS-P includes non-physical components like anxiety, depression, post-traumatic stress disorder and cognitive impairment and physical problems like ICU acquired weakness, mobility impairment, glottis dysfunction, pain or pulmonary function impairment.2 The real prevalence of PICS among ICU survivors is still unknown, with some studies reporting an incidence as high as 73% at hospital discharge and 46% one year after ICU.3,4
The National Institute for Health and Care Excellence published guidelines for managing rehabilitation after critical care and have proposed a care pathway for these patients.5 In a first stage, at ICU admission patients at risk should be identified. Risk factors for PICS-P are based both on patient background and acute illness features. Previous mobility, respiratory or cognitive impairments, long expected ICU stay, physical or neurological injury, acute physical impairment and severe respiratory failure are risk factors for physical PICS components. On the other hand, risk factors for psychological PICS are previous psychiatric disorder, dementia or story at ICU of nightmares, intrusive memories, anxiety, recurrent panic attacks and refusing to talk about the disease. On a second stage, PICS components should be identified before ICU discharge and rehabilitation should be started as soon as possible. After discharge, a follow-up team should accompany the patient during ward based-care focused on rehabilitation goals and a revaluation should be made before discharge to home or community. In a fourth stage, the patient should be revaluated 2 to 3 months after critical care.5
Although most of the studies done after ICU care are focused in the patient despite the recognition that they are not the only ones affected by ICU stay. Caregivers play a crucial role in patients’ recovery and they face themselves many stressors like fearfulness, disruption of family dynamics, financial pressure and work overload, all of which can contribute to caregiver burden. In the light of this knowledge PICS has also been recognized for caregivers, particularly families (PICS-F).6,7 Extensive burdens are described for families following the patient's ICU admission, related mostly with psychosocial issues, quality of life, lifestyle, employment and financial status.8
Even though there is an increasing awareness of the importance of psychological impairments and burden is common in caregivers, more studies are needed to relate patient status after discharge (PICS-P) and PICS-F in a way that will allow the ICU teams to intervene and prevent or treat it.
This study aims to determine the incidence of patient's post-intensive care syndrome (PICS-P) and caregiver's burden 3 months after Intensive Care Unit (ICU) discharge and determine the impact of different components of PICS-P on caregiver's burden.
Patients and methodsA prospective study was conducted over a 26-month period, between January 2013 and February 2015 in a mixed surgical-medical adult ICU and the Follow-up Clinic.
HospitalHospital Pedro Hispano has an open model, mixed surgical-medical intensive care unit with 8 beds and approximately 300 admissions per year. The ICU outreach team has different components with a Medical Emergency Team and a Follow-up Team. The Follow-up Team is responsible for the assessment of patients during all hospital stay after ICU, in particularly at three moments: first week, 1 month after ICU or at the hospital discharge and 3 months after discharge from ICU in a Follow-up Clinic. A nurse and a physician make up the Follow-up Team.
Patients assessment and patient's post-intensive care syndromeAll surviving patients who stayed at ICU for at least two days were included along with their family. Patient characteristics, severity of illness (measured with SAPS II at first 24h)9 and length of ICU stay were collected. Risk for PICS was assessed at admission based on described risk factors and patients with at least one risk factor were considered as at risk. All patients, both considered as at risk or not, were assessed for PICS at different moments namely at ICU discharge, at their first week in ward, at 1 month after or hospital discharge and at 3 months after discharge. Three months after ICU stay patients were invited to attend the Follow-up Clinic for revaluation and PICS assessment. In all moments patients were evaluated for both physical and non-physical PICS.
Physical components (mobility impairment, ICU-acquired weakness) were clinically evaluated and the “Medical Research Council Scale for Muscle Strength” was used.10 A score ≤4 was considered for a decreased muscle strength and if present in at least two muscular groups was coded as ICU acquired weakness. As for the psychological components (anxiety, depression, post-traumatic stress disorder), the questionnaires “Hospital Anxiety and Depression Scale” (HADS)11 and “Post-Traumatic Stress Syndrome 14 Questions Inventory” (PTSS-14)12 were applied. For Anxiety and Depression subscales, a HADS >10 was considered positive to the mood disorder and a HADS between 8 and 10 as being suggestive of the presence of the respective state (the authors used the number ten as cut-off decision). A PTSS ≥49 was considered positive to post-traumatic stress disorder risk. Before 3 months’ assessment, questionnaires were sent by mail in advance. In all moments patients received the questionnaires in advance and were able to answer then alone and quietly. For the purpose of this study only data on PICS-P at 3 months after ICU discharge was analyzed, independently how much time passed over the date of hospital discharge.
Caregivers assessment and caregiver's burdenCaregiver was defined as the individual who provided the majority of support for the patient. No cohabitation or legal relation with the patient was required. Caregiver eligibility criteria included: being a non-paid caregiver, able to read and speak Portuguese and accept to participate in the study.
Caregivers were invited to the Patients’ Follow-up Clinic to assess burden 3 months after the patient discharge and were evaluated in the same day as the patient. Family burden was assessed using the “Zarit Burden Interview” which is a self-response questionnaire designed to expose the issues experienced by caregivers.13–16 Caregivers were asked to respond to a series of 22 questions about the impact of the patients’ disabilities on their life. For each item, caregivers indicate how often they felt that specific burden (never=0, rarely=1, sometimes=2, quite frequently=3, or nearly always=4). Higher scores indicate greater caregiver distress. As previously described by Zarit, caregivers were classified as without overburden if the Zarit result was less than or equal to 21, with low overburden if they reach a score between 22 and 40, or with high overburden if they have a score of at least 41.17 The questionnaire was sent in advance by mail to all caregivers which allowed them to answered it quietly and lonely at home and then bring it to the Follow-up Clinic. Caregiver's burden was assessed only at 3 months after patient's ICU discharge.
Ethical aspectsIt was a purely observational study without any implication in patients or caregivers’ treatment. All questionnaires, both for patients and caregivers, were preceded by an introduction where it was explained the purpose of the questionnaire and that it would be used in a scientific observational study. Informed consent was waved. Patients and caregivers voluntarily answered the questionnaires and confidentiality was maintained. This study has been assessed and approved by the Institutional Ethics Committee.
Statistical analysisThe relationship between caregiver's burden and the presence of different components of patient's PICS, patient characteristics, severity of illness and length of ICU stay were also analyzed. Categorical variables were described through absolute (n) and relative (%) frequencies, and continuous variables were described as mean and standard deviation, median, percentiles, and minimum and maximum when appropriate. Hypotheses were tested regarding the distribution of continuous variables with non-normal distribution by using the non-parametric Mann–Whitney and Kruskal–Wallis tests, depending on the nature of the hypothesis. For categorical variables, a Chi-square test or a Fisher's exact test was used, as appropriate.
All the reported p-values were two-sided, and p-values of <0.05 were considered statistically significant. All data were arranged, processed and analyzed with SPSS® v.23.0 (Statistical Package for Social Sciences).
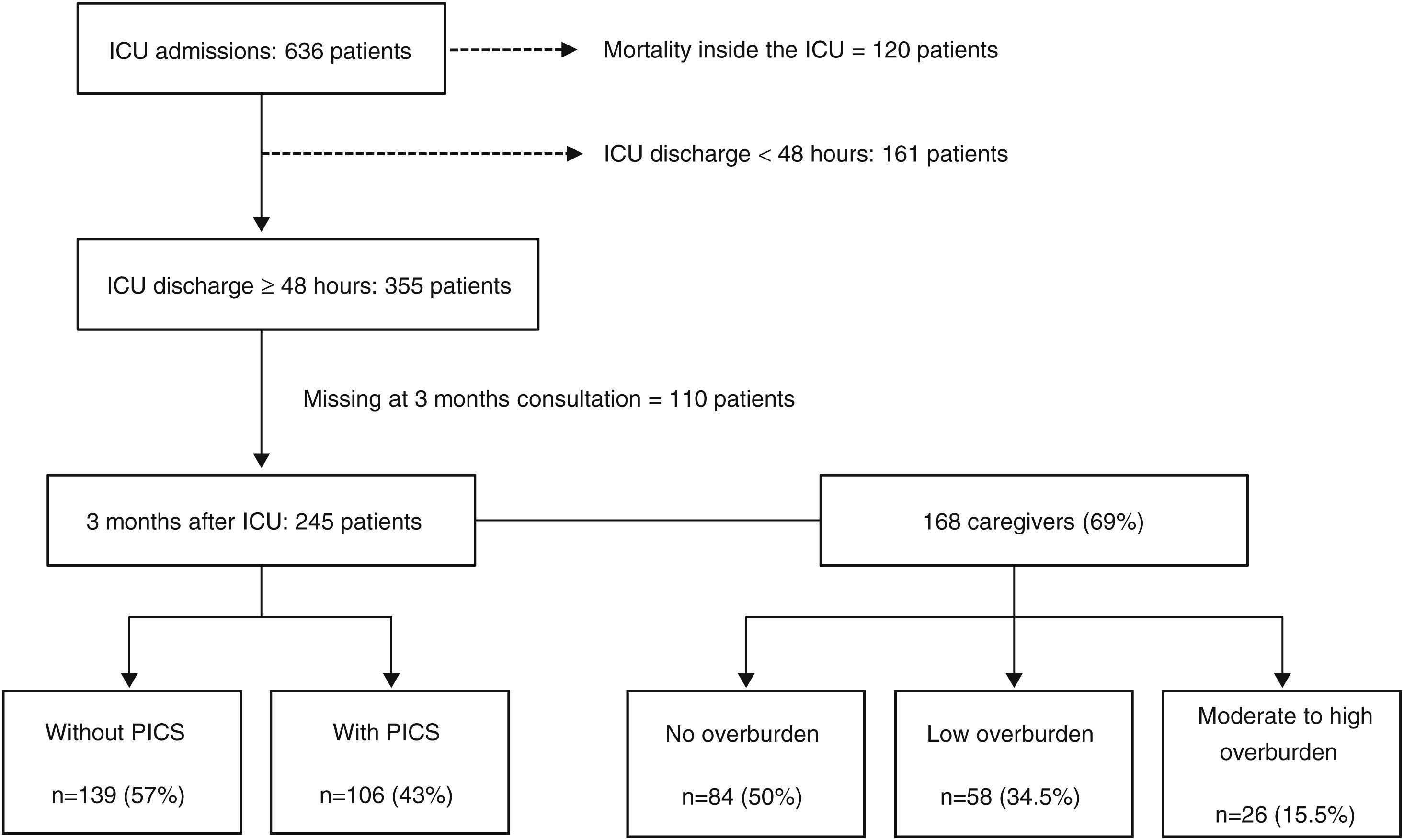
ResultsPatient's post-intensive care syndrome 3 months after ICU dischargeDuring the study period 636 patients were admitted to ICU. The most frequent admission motives were: septic shock, respiratory failure and post-major surgery. The mortality rate was 19% (n=120). From surviving patients, 161 were excluded from the study as they stayed less than 48h at the ICU. A total of 355 met the criteria to be followed by the Follow-up team and 245 were evaluated in the Follow-up Clinic 3 months after (Fig. 1). Fifty-seven patients died between ICU discharge and consultation and another 53 missed the clinic for different reasons. Patient characteristics at 3 months Follow-up Clinic are summarized in Table 1.
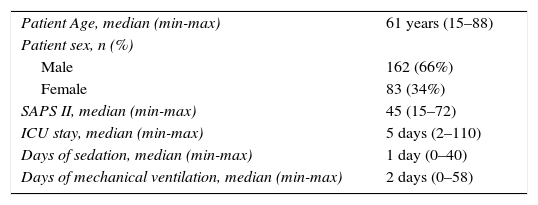
Patient characteristics at follow-up consultation 3 months after ICU.
| Patient Age, median (min-max) | 61 years (15–88) |
| Patient sex, n (%) | |
| Male | 162 (66%) |
| Female | 83 (34%) |
| SAPS II, median (min-max) | 45 (15–72) |
| ICU stay, median (min-max) | 5 days (2–110) |
| Days of sedation, median (min-max) | 1 day (0–40) |
| Days of mechanical ventilation, median (min-max) | 2 days (0–58) |
Abbreviations: n, number; Min, Minimum; Max, Maximum.
Three months after their ICU stay, 106 patients (43%) reported at least one component of PICS: 20% had depression, 19% anxiety, 11% post-traumatic stress disorder, 11% mobility impairment and 20% ICU acquired weakness.
Caregivers’ burdenOver the study period, 168 caregivers completed the survey, with a response rate of 69% as 77 patients failed to have their caregiver evaluated (Fig. 1). Exactly 50% (n=84) of the caregivers reported no overburden, 34.5% (n=58) experienced low overburden and 15.5% (n=26) felt moderate to high overburden.
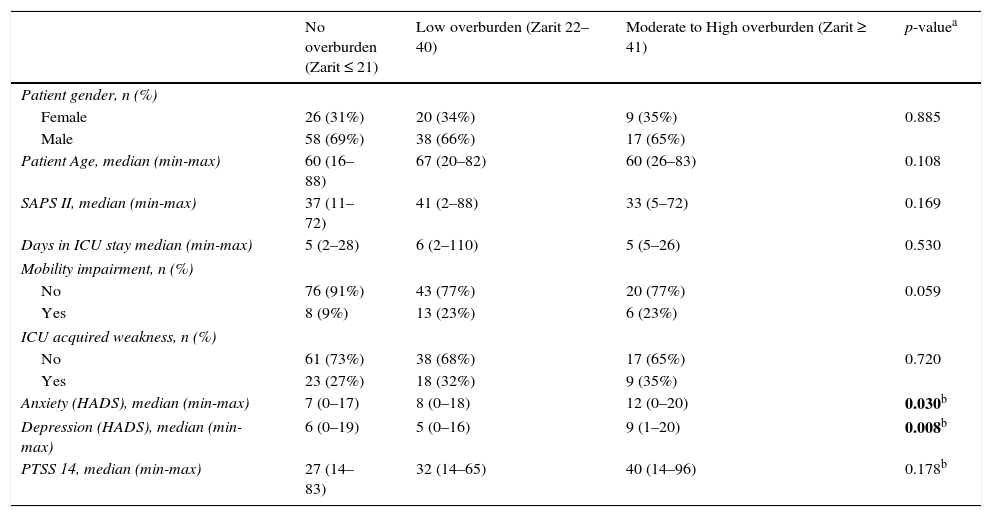
Impact of patient's PICS on caregiver's burdenImpact of patient's PICS on caregiver's burden was finally analyzed on a sample of 168 patients and caregivers (paired). From this group, two patients sent their answered questionnaires to the clinic but failed to be present there, so they were not evaluated for physical limitations. For that reason, for comparison between caregivers and physical PICS only 166 pairs were considered.
Patient's anxiety and depression at 3 months (median HADS of 12 for anxiety and Median HADS of 9 for depression) has a statically significant association with higher degrees of caregiver's overburden (Zarit ≥ 41). Physical components of patients’ PICS at 3 months failed to show influence on caregivers’ burden. There were no differences in caregivers’ burden regarding patients gender, age, SAPS II and ICU length of stay (Table 2).
Association between patients’ PICS and caregivers’ burden 3 months after ICU.
| No overburden (Zarit ≤ 21) | Low overburden (Zarit 22–40) | Moderate to High overburden (Zarit ≥ 41) | p-valuea | |
|---|---|---|---|---|
| Patient gender, n (%) | ||||
| Female | 26 (31%) | 20 (34%) | 9 (35%) | 0.885 |
| Male | 58 (69%) | 38 (66%) | 17 (65%) | |
| Patient Age, median (min-max) | 60 (16–88) | 67 (20–82) | 60 (26–83) | 0.108 |
| SAPS II, median (min-max) | 37 (11–72) | 41 (2–88) | 33 (5–72) | 0.169 |
| Days in ICU stay median (min-max) | 5 (2–28) | 6 (2–110) | 5 (5–26) | 0.530 |
| Mobility impairment, n (%) | ||||
| No | 76 (91%) | 43 (77%) | 20 (77%) | 0.059 |
| Yes | 8 (9%) | 13 (23%) | 6 (23%) | |
| ICU acquired weakness, n (%) | ||||
| No | 61 (73%) | 38 (68%) | 17 (65%) | 0.720 |
| Yes | 23 (27%) | 18 (32%) | 9 (35%) | |
| Anxiety (HADS), median (min-max) | 7 (0–17) | 8 (0–18) | 12 (0–20) | 0.030b |
| Depression (HADS), median (min-max) | 6 (0–19) | 5 (0–16) | 9 (1–20) | 0.008b |
| PTSS 14, median (min-max) | 27 (14–83) | 32 (14–65) | 40 (14–96) | 0.178b |
Abbreviations: n, number; Min, minimum; Max, Maximum; HADS, Hospital Anxiety and Depression Scale; PTSS 14, Post-Traumatic Stress Syndrome 14 Questions Inventory.
The main finding of this study is that the presence of psychological components of Post Intensive Care Syndrome 3 months after ICU seems to influence negatively the overburden of caregivers. On the other hand, physical problems failed to show important impact in caregivers’ overburden.
As far as we know, no study directly related the different components of PICS-P at 3 months with caregiver's burden at this same time. We believe that our findings show an important relation between them that might help defining a strategy to identify and deal with caregivers at risk.
Several articles show that family members of critically ill patients are at risk for anxiety and depressive conditions, and the combination of this is known as PICS-F, though there is disagreement on what the term “caregiver burden” means. A recent review from Van Beusekom et al.8 analyses the usual reported burden and the tools used to measure it. It is discussed that caregivers have extensive burdens, from changes in psychological status, employment and lifestyle to decreased quality of life. This review paper reported caregivers’ burden prevalence between 16% and 90% during ICU or hospital stay, between 12.2% and 26.2% at 3 months, 4.7% and 36.4% at 6 months and between 22.8% and 44% at 12 months after ICU discharge. In our population, the prevalence of patients’ PICS is consistent with this and other studies.3,4
Caring and dealing with an acutely ill loved one can be stressful and difficult to handle. The psychological recovery of the family has tended to be forgotten and high rates of anxiety, depression and Post-Traumatic Stress Disorder have been reported in caregivers.18 PICS-F and caregiver's burden should be assessed so caregivers can receive professional care if necessary. It's not clear what is the best method for their assessment and several scales were used, like Zarit Burden Interview,13 Hospital Anxiety and Depression Scale subscale11 or “Post-Traumatic Stress Syndrome 14 Questions Inventory (PTSS-14)”.12 In this study, Zarit Burden Interview was used because it's a simple self-answering questionnaire already translated, used and validated in the Portuguese population.16
Identifying predictors of adverse caregivers’ outcome is fundamental for targeting intervention strategies. Previous identified caregiver's risk factors for PICS-F are female gender, younger relative, being a spouse, older patients age, more chronic conditions, lifestyle interference, lower mastery and overload.6,19 In our study patient gender, age, severity of illness and length of ICU stay also failed to show influence on caregiver's burden.
Few studies have evaluated patient specific predictors of caregivers’ burden or PICS-F. Some studies try to relate physical and functional PICS-P with caregiver burden with inconsistent results.13,20–23 Swoboda et al. found a relation between caregiver burden using a family impact survey and patient functional status using the Sickness Impact Profile.21 Choi et al. finds a relation between caregiver burden using the Zarit interview and patient functional status using the Activities of Daily Living.20 All the studies show a small sample size in a single centre with important selection bias. However other studies fail to find a significant relation between the family burden and the physical patient status20,22,23 and are in accordance with our findings. Notably Van Pelt et al. finds a lack of relation between caregiver burden using the Centre for Epidemiologic Studies Depression and patient functional status using the Activities of Daily Living in their ICU cohort patients.22 Also in accordance with our study, Choi et al. show that remains high even caregiver distress if the patient regains pre-admission functional status.20
Regarding studies that relate psychological PICS-P with caregiver burden: we’ve only found one paper from Cameron et al.24 and this study is in line with ours. They found that caregiver emotional distress was higher when the ARDS survivors reported more depressive symptoms. The survivors’ functional status, expressed as the distance walked in 6min, was not associated with the informal caregiver emotional stress, also in accordance with what we found.
Both previous studies and ours suggest that it is easier for relatives to accept and adapt to physical limitations than to deal with a psychologically wounded patient. More studies are needed to understand caregiver role and burden in the care of ICU patients.
This study has some limitations that have to be pointed out. It is a single-centre study with a small sample that may be insufficient to extrapolate results onto the general population. Furthermore, the questionnaire was self-reported but not anonymous as mail was sent to the ICU patient, so caregivers may have been afraid to be judged by their relatives or professionals for their answers. More importantly we did not collect data on the caregiver characteristics that we could relate to its burden.
Additionally, the responses of the 31% of the caregivers who did not participate in the study could have a significant impact on the conclusions drawn.
In conclusion, the caregiver's role is frequently under-looked by professionals, but is nonetheless essential in the patient's recovery. Our study shows that post ICU patient anxiety and depression play an important role in the burden of caregivers.
Identification of PICS-P is fundamental not only to define an early strategy for patients but also to prevent overburden and PICS-F in caregivers. A structured multidisciplinary approach is crucial and should be designed to identify, support and help caregivers at risk. A more comprehensive study is required to better understand the connections between different components of PICS-P and PICS-F.
FundingNone.
Contribution of the authorsJT, DC, EM, CV, AF, RA and EG designed the study and managed data collection. Analysis and interpretation of data was undertaken by CCD. JT and EG wrote the first manuscript draft and were responsible for subsequent collation of inputs and redrafting. DC, EM and RA helped to revise the manuscript. All authors read and approved the final manuscript.
Conflict of interestsNone.