To explore combined non-invasive-respiratory-support (NIRS) patterns, reasons for NIRS switching, and their potential impact on clinical outcomes in acute-hypoxemic-respiratory-failure (AHRF) patients.
DesignRetrospective, single-center observational study.
SettingIntensive Care Medicine.
PatientsAHRF patients (cardiac origin and respiratory acidosis excluded) underwent combined NIRS therapies such as non-invasive-ventilation (NIV) and High-Flow-Nasal-Cannula (HFNC).
InterventionsPatients were classified based on the first NIRS switch performed (HFNC-to-NIV or NIV-to-HFNC), and further specific NIRS switching strategies (NIV trial-like vs. Non-NIV trial-like and single vs. multiples switches) were independently evaluated.
Main variables of interestReasons for switching, NIRS failure and mortality rates.
ResultsA total of 63 patients with AHRF were included, receiving combined NIRS, 58.7% classified in the HFNC-to-NIV group and 41.3% in the NIV-to-HFNC group. Reason for switching from HFNC to NIV was AHRF worsening (100%), while from NIV to HFNC was respiratory improvement (76.9%). NIRS failure rates were higher in the HFNC-to-NIV than in NIV-to-HFNC group (81% vs. 35%, p < 0.001). Among HFNC-to-NIV patients, there was no difference in the failure rate between the NIV trial-like and non-NIV trial-like groups (86% vs. 78%, p = 0.575) but the mortality rate was significantly lower in NIV trial-like group (14% vs. 52%, p = 0.02). Among NIV to HFNC patients, NIV failure was lower in the single switch group compared to the multiple switches group (15% vs. 53%, p = 0.039), with a shorter length of stay (5 [2–8] vs. 12 [8–30] days, p = 0.001).
ConclusionsNIRS combination is used in real life and both switches’ strategies, HFNC to NIV and NIV to HFNC, are common in AHRF management. Transitioning from HFNC to NIV is suggested as a therapeutic escalation and in this context performance of a NIV-trial could be beneficial. Conversely, switching from NIV to HFNC is suggested as a de-escalation strategy that is deemed safe if there is no NIRS failure.
Explorar los patrones combinados de soporte-respiratorio-no-invasivo (SRNI), las razones para cambiar de SRNI y su potencial impacto en los resultados clínicos en pacientes con insuficiencia-respiratoria-aguda-hipoxémica (IRAH).
DiseñoEstudio observacional retrospectivo unicéntrico.
ÁmbitoCuidados Intensivos.
PacientesPacientes con IRAH (excluyendo causa cardíaca y acidosis respiratoria) que recibieron tanto ventilación-no-invasiva (VNI) como cánula-nasal-de-alto-flujo (CNAF).
IntervencionesSe categorizó a los pacientes según el primer cambio de SRNI realizado (CNAF-to-VNI o VNI-to-CNAF) y se evaluaron estrategias específicas de SRNI (VNI trial-like vs. Non-VNI trial-like y cambio único vs. múltiples cambios de NIRS) de manera independiente.
Variables de interés principalesRazones para el cambio, así como las tasas de fracaso de SRNI y la mortalidad.
ResultadosUn total de 63 pacientes recibieron SRNI combinado, 58,7% clasificados en el grupo CNAF-to-VNI y 41,3% en el grupo VNI-to-CNAF. Los cambios de CNAF a VNI ocurrieron por empeoramiento de la IRHA (100%) y de VNI a CNAF por mejora respiratoria (76.9%). Las tasas de fracaso de SRNI fueron mayores de CNAF a VNI que de VNI a CNAF (81% vs. 35%, p < 0.001). Dentro de los pacientes de CNAF a VNI, no hubo diferencia en las tasas de fracaso entre los grupos VNI trial-like y no-VNI trial-like (86% vs. 78%, p = 0.575), pero la mortalidad fue menor en el grupo VNI trial-like (14% vs. 52%, p = 0.02). Dentro de los pacientes de VNI a CNAF, el fracaso de VNI fue menor en grupo de cambio único vs. múltiple (15% vs. 53%, p = 0.039).
ConclusionesLos cambios de estrategia de SRNI son comunes en el manejo clínico diario de la IRHA. El cambio de CNAF a VNI impresiona de ser una escalada terapéutica y en este contexto la realización de un VNI-trial puede ser beneficioso. Al contrario, cambiar de VNI a CNAF impresiona de ser una desescalada terapéutica y parece segura si no hay fracaso del SRNI.
Non-invasive respiratory support (NIRS) such as non-invasive ventilation (NIV) or High-Flow Nasal Cannula (HFNC), is commonly used in acute hypoxemic respiratory failure (AHRF), a common complication of many diseases with a mortality of up to 45%.1 Its utilization has been shown to avoid the need for intubation improving clinical outcomes in selected patients but without clear benefits in mortality rates.2–4. The use of NIRS may directly reduce the complications associated with endotracheal intubation and invasive mechanical ventilation (IMV).5–11 However, approximately 37.5% of patients treated with NIRS still require endotracheal intubation.1,7,12–14
Although NIV was the only NIRS strategy available and used for AHRF for many years, in 2015, Frat et al. published a landmark paper supporting the role of HFNC in the management of AHRF, and its use rapidly increased over the years. They showed that its use was associated with lower mortality, more ventilator-free days, and a lower risk for intubation in subsets of severe hypoxemic patients.15–17. Currently, combined use of NIRS strategies has been described. In this regard, Frat et al. used HFNC as a rest tool to increase NIV tolerability, and Wang et al. used sequential HFNC and NIV in the post-extubation period.18,19 However, there is limited data regarding the specific switches performed in patients with AHRF (NIRS patterns) and their association with clinical outcomes.
Despite the significant benefits of NIRS, some studies have shown that patients who fail NIRS as the initial therapy for AHRF present worse outcomes. This has been convincingly demonstrated with NIV, especially in patients treated for pneumonia, but also with HFNC.20–22. The latest European Respiratory Society (ERS)/American Thoracic Society (ATS) guidelines for non-invasive AHRF management23 and the ERS guideline for the management of severe community-acquired pneumonia24 did not provide formal recommendation to follow when NIRS techniques fail and there are no specific standardized criteria for NIRS failure that can be used in clinical practice or research studies. In this context, two scales have been described and validated to predict NIRS failure, ROX index for HFNC and HACOR score for NIV.25,26 However, they are not commonly used in daily clinical practice due to their high specificity to be useful since they do not usually anticipate clinical criteria in predicting failure. Lack of recommendations in the national or international guidelines and the low usability of the available scales could lead to an uncontrolled use of NIRS, including multiple NIRS switches that could delay intubation, worsening the outcomes of some patients.27–29 In this sense, it has been described the imperative need to monitor the patient's clinical trend towards improvement, stagnation or deterioration during the initial use of NIV (NIV-trial), to avoid delaying endotracheal intubation, as it can lead to increased mortality.27–29 However, specific criteria to define the failure of a NIV-trial have not been established yet.
The aim of this study was to describe the pattern of combined NIRS use (HFNC and NIV), determining the reasons for switching NIRS and evaluating the association of specific NIRS switching strategies with clinical outcomes in patients with AHRF.
MethodsStudy design, participants and study groupsThis was a retrospective, single center and observational study. Data were collected for all patients admitted to the Critical Care Department of Hospital del Mar (Barcelona, Spain) with AHRF caused by a respiratory condition and who received both NIRS therapies combined, HFNC and NIV, as first respiratory support strategy between January 2017 and December 2018. Patients under the age of 18, AHRF caused by a cardiac condition or with respiratory acidosis were excluded from the analysis. Patients were classified based on the first NIRS switch performed in the HFNC-to-NIV group when they were initially treated with HFNC for their AHRF and a further switch to NIV happened or in the NIV-to-HFNC group when they were initially treated with NIV, and a further switch to HFNC occurred. NIRS switches were based on the clinical decisions of the treating physicians. A cross-sectional descriptive analysis was done at the time of inclusion, when the first therapy was initiated, as well as when the second therapy was initiated. Moreover, a longitudinal analysis was also performed to evaluate outcomes such as NIRS failure, ICU, and hospital length of stay (LOS), and mortality.
Data source and data collectionData source was the ICU stock software information in Hospital del Mar (IMASIS30), which provides hourly vital sign constants, devices connected to the patient (such as HFNC or NIV), ventilatory parameters, variables measured by the ventilator or bed monitor, patient location, and vital state. Therefore, data collection was manually and retrospectively performed from IMASIS, including all clinical and ventilatory data necessary to evaluate the study objectives. This included demographics, anthropometrics, comorbidities, severity indexes at admission, AHRF etiology, vital signs and arterial blood gases. Specific ventilatory variables such as the type, sequence, and parameters of ventilatory support received, reasons for switching and NIRS failure, ICU and hospital LOS and mortality, as well as data related to do not intubate orders (DNIO) were also extracted.
Specific switching groups analysesPatients in both switching groups were further classified in two subgroups depending on specific NIRS switching strategies and a descriptive analysis was performed to better understand their potential influence on NIRS failure, ICU and hospital LOS, and mortality.
HFNC-to-NIV groupSpecific NIRS switching strategy in this group of patients was defined based on previously described criteria used to perform a NIV-trial.28,29 Consequently, patients were stratified as: 1) NIV trial-like (those patients who were retrospectively inferring to meet the NIV-trial criteria and were ventilated under a controlled strategy) and 2) Non-NIV trial-like (those patients who did not meet the NIV-trial criteria and were not ventilated under a controlled strategy). To do that, all clinical data of included patients were evaluated during the 6 h after NIV starting. Patients exhibiting clinical improvement during this period of time as well as patients exhibiting clinical deterioration and who were intubated were both considered as ventilated under a controlled strategy (NIV trial-like) and those patients presenting clinical deterioration and who were not intubated, were considered as ventilated under a non-controlled strategy (non-NIV trial-like). Moreover, patients in whom a NIV-trial intention was reported in the electronic health report during this period of time were also included in the NIV trial-like group. Clinical deterioration was considered when a 5% worsening of parameters such as respiratory rate (RR), peripheral oxygen saturation (SpO2), arterial blood gas sample partial pressure of oxygen (PaO2), and the need for an increase in the fraction of inspired oxygen (FiO2) was observed from the start of the NIV technique and during the 6 following hours. Clinical improvement was considered when a 5% improvement of at least two of the parameters detailed above was detected in the same period of time.
NIV-to-HFNC groupIn this group of patients, specific NIRS switching strategy was based on the number of NIRS switches observed in NIV-to-HFNC patients. Consequently, patients were stratified regarding the number of switches as: 1) Single NIRS switch (those patients with only one NIRS switch described) and 2) Multiple NIRS switches (those patients with more than one NIRS change).
Statistical analysisCategorical variables were expressed as frequencies and percentages, and continuous variables as means and standard deviations (SD) when data were normally distributed, or otherwise as median and interquartile range (25th-75th percentile). The normality of the distribution of each variable was determined using the Kolmogorov-Smirnov test. Differences between groups were analyzed using the chi square test or Fisher’s exact test for categorical variables, and ANOVA, Student’s t-test or the Mann-Whitney U test for continuous data. Statistical significance was set at a p-value ≤ 0.05. Given a priori sample size estimation was not conducted, we assessed the statistical power of our analysis for the most important outcome (NIRS failure). We performed a power analysis for the chi-square test, which yielded a statistical power of 80%. This was calculated with a sample size of 63 patients, 1 degree of freedom, a significance level (alpha) set at 0.05, and anticipating a moderate effect size of 0.35. The data were analyzed using the Statistical Package for the Social Sciences (SPSS, Chicago, IL, USA) 18 version.
Ethical considerationsPatient identities were anonymized to ensure confidentiality. Due to the retrospective and non-interventional character of the study, individual patient consent was not required. The study and its database were developed and implemented in accordance with the amended Declaration of Helsinki in its latest version, and the study received approval from the Institutional Review Board of PSMAR (IRB code: 2020/9050). The preparation of this paper followed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) recommendations.
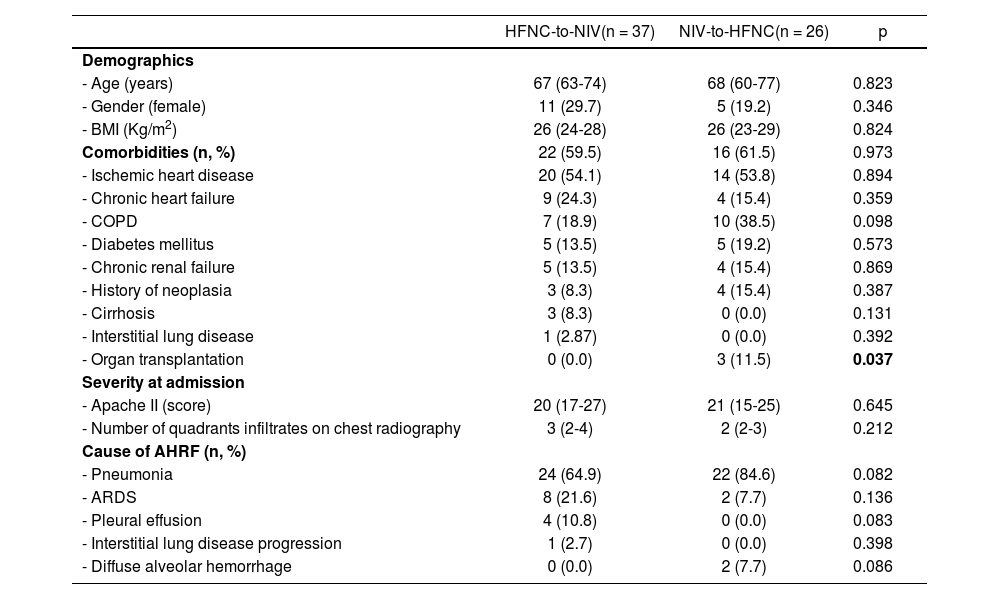
ResultsDistribution and characteristics of patientsA total of 194 patients were admitted to the ICU for AHRF needing NIRS as initial respiratory support strategy during the study period. Among them, 63 (32.5%) patients underwent both, HFNC and NIV, which were classified as following: 37 patients (58.7%) in the HFNC-to-NIV group and 26 patients (41.3%) in the NIV-to-HFNC group. Table 1 shows the main characteristics of included patients in both groups.
Patients characteristics in both study groups.
| HFNC-to-NIV(n = 37) | NIV-to-HFNC(n = 26) | p | |
|---|---|---|---|
| Demographics | |||
| - Age (years) | 67 (63-74) | 68 (60-77) | 0.823 |
| - Gender (female) | 11 (29.7) | 5 (19.2) | 0.346 |
| - BMI (Kg/m2) | 26 (24-28) | 26 (23-29) | 0.824 |
| Comorbidities (n, %) | 22 (59.5) | 16 (61.5) | 0.973 |
| - Ischemic heart disease | 20 (54.1) | 14 (53.8) | 0.894 |
| - Chronic heart failure | 9 (24.3) | 4 (15.4) | 0.359 |
| - COPD | 7 (18.9) | 10 (38.5) | 0.098 |
| - Diabetes mellitus | 5 (13.5) | 5 (19.2) | 0.573 |
| - Chronic renal failure | 5 (13.5) | 4 (15.4) | 0.869 |
| - History of neoplasia | 3 (8.3) | 4 (15.4) | 0.387 |
| - Cirrhosis | 3 (8.3) | 0 (0.0) | 0.131 |
| - Interstitial lung disease | 1 (2.87) | 0 (0.0) | 0.392 |
| - Organ transplantation | 0 (0.0) | 3 (11.5) | 0.037 |
| Severity at admission | |||
| - Apache II (score) | 20 (17-27) | 21 (15-25) | 0.645 |
| - Number of quadrants infiltrates on chest radiography | 3 (2-4) | 2 (2-3) | 0.212 |
| Cause of AHRF (n, %) | |||
| - Pneumonia | 24 (64.9) | 22 (84.6) | 0.082 |
| - ARDS | 8 (21.6) | 2 (7.7) | 0.136 |
| - Pleural effusion | 4 (10.8) | 0 (0.0) | 0.083 |
| - Interstitial lung disease progression | 1 (2.7) | 0 (0.0) | 0.398 |
| - Diffuse alveolar hemorrhage | 0 (0.0) | 2 (7.7) | 0.086 |
Data expressed as frequencies and percentages [n(%)] or medians and interquartile ranges (IQR or 25th-75th percentile).
HFNC: high flow nasal cannula, NIV: non-invasive ventilation, BMI: body mass index, COPD: chronic obstructive pulmonary disease, APACHE: acute physiology and chronic health evaluation, AHRF: acute hypoxemic respiratory failure, ARDS: acute respiratory distress syndrome.
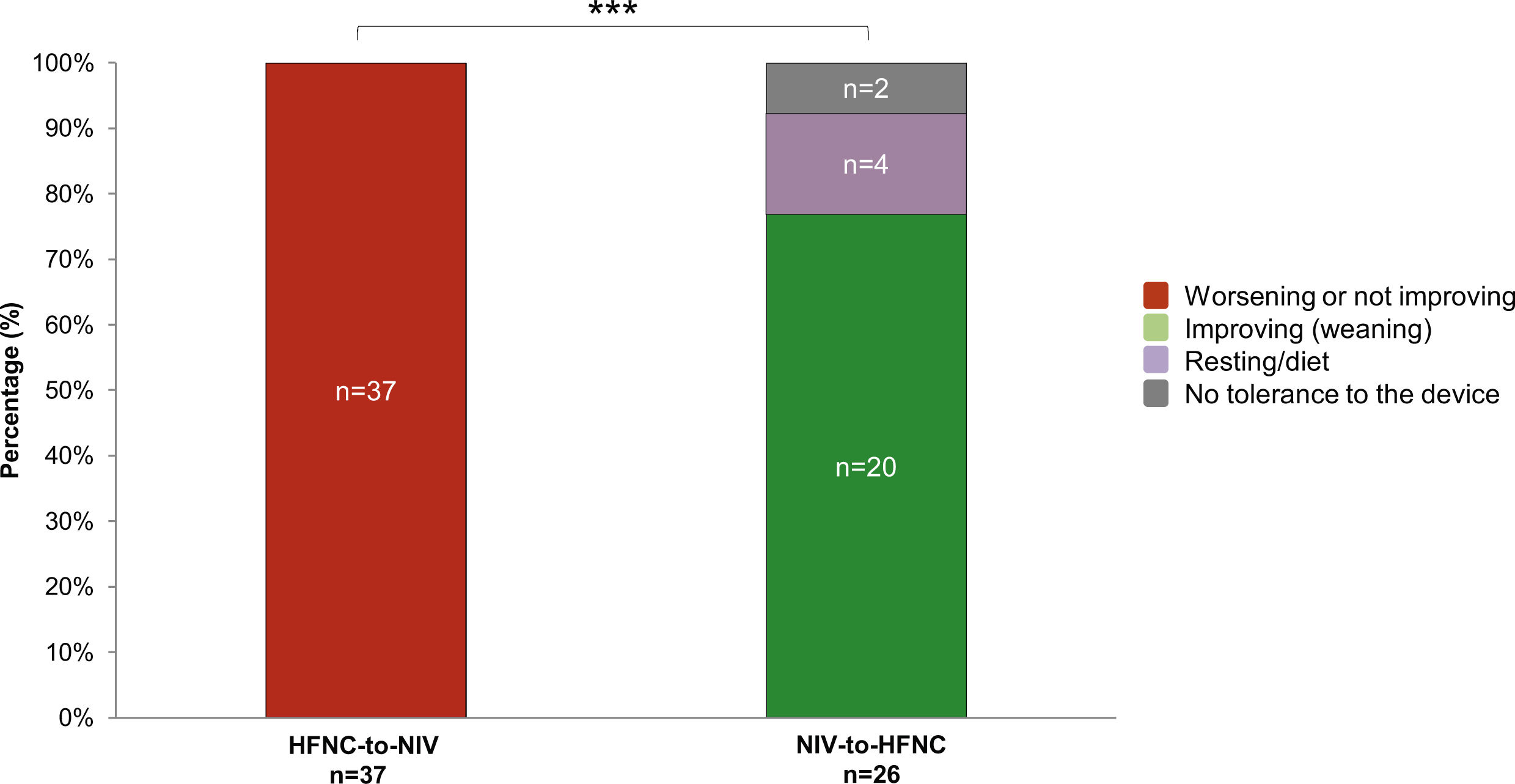
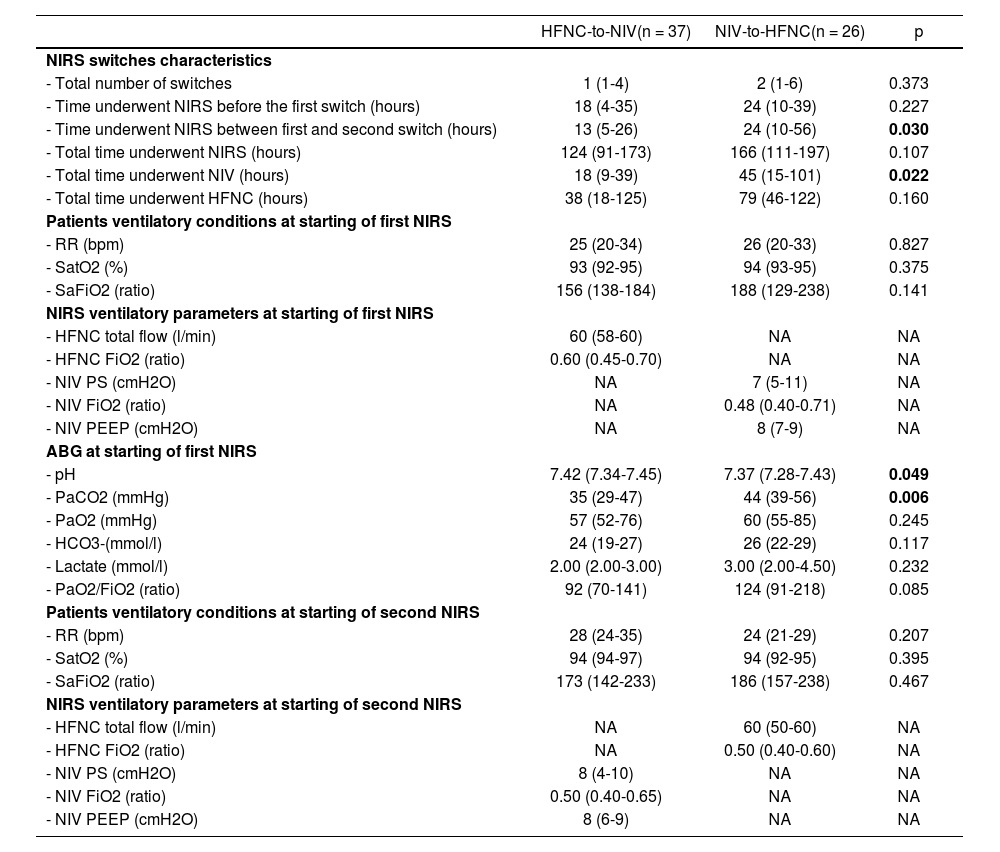
Table 2 shows the main NIRS switches characteristics. Patients in the group NIV-to-HFNC tended to present higher number of NIRS switches than patients in the group HFNC-to-NIV (2 (1–6) vs. 1 (1–4) switches, p = 0.373). NIV-to-HFNC patients spent more time undergoing NIRS than HFNC-to-NIV (166 (111–197) vs. 124 (91–173) hours, p = 0.107), either NIV (45 (15–101) vs. 18 (9–39) hours, p = 0.022) or HFNC (79 (46–122) vs. 38 (18–125) hours, p = 0.160). Respiratory worsening or not improving was the reason leading to the first NIRS change in all HFNC-to-NIV patients (n = 37, 100%). Otherwise, respiratory improvement (NIV weaning), was the most common reason for change in NIV-to-HFNC patients with 77% (n = 20) (Fig. 1). The data regarding respiratory and ventilatory-related variables at the start of first and second NIRS are also detailed in Table 2.
NIRS switches characteristics and patients' characteristics at starting of first and second NIRS in both study groups.
| HFNC-to-NIV(n = 37) | NIV-to-HFNC(n = 26) | p | |
|---|---|---|---|
| NIRS switches characteristics | |||
| - Total number of switches | 1 (1-4) | 2 (1-6) | 0.373 |
| - Time underwent NIRS before the first switch (hours) | 18 (4-35) | 24 (10-39) | 0.227 |
| - Time underwent NIRS between first and second switch (hours) | 13 (5-26) | 24 (10-56) | 0.030 |
| - Total time underwent NIRS (hours) | 124 (91-173) | 166 (111-197) | 0.107 |
| - Total time underwent NIV (hours) | 18 (9-39) | 45 (15-101) | 0.022 |
| - Total time underwent HFNC (hours) | 38 (18-125) | 79 (46-122) | 0.160 |
| Patients ventilatory conditions at starting of first NIRS | |||
| - RR (bpm) | 25 (20-34) | 26 (20-33) | 0.827 |
| - SatO2 (%) | 93 (92-95) | 94 (93-95) | 0.375 |
| - SaFiO2 (ratio) | 156 (138-184) | 188 (129-238) | 0.141 |
| NIRS ventilatory parameters at starting of first NIRS | |||
| - HFNC total flow (l/min) | 60 (58-60) | NA | NA |
| - HFNC FiO2 (ratio) | 0.60 (0.45-0.70) | NA | NA |
| - NIV PS (cmH2O) | NA | 7 (5-11) | NA |
| - NIV FiO2 (ratio) | NA | 0.48 (0.40-0.71) | NA |
| - NIV PEEP (cmH2O) | NA | 8 (7-9) | NA |
| ABG at starting of first NIRS | |||
| - pH | 7.42 (7.34-7.45) | 7.37 (7.28-7.43) | 0.049 |
| - PaCO2 (mmHg) | 35 (29-47) | 44 (39-56) | 0.006 |
| - PaO2 (mmHg) | 57 (52-76) | 60 (55-85) | 0.245 |
| - HCO3-(mmol/l) | 24 (19-27) | 26 (22-29) | 0.117 |
| - Lactate (mmol/l) | 2.00 (2.00-3.00) | 3.00 (2.00-4.50) | 0.232 |
| - PaO2/FiO2 (ratio) | 92 (70-141) | 124 (91-218) | 0.085 |
| Patients ventilatory conditions at starting of second NIRS | |||
| - RR (bpm) | 28 (24-35) | 24 (21-29) | 0.207 |
| - SatO2 (%) | 94 (94-97) | 94 (92-95) | 0.395 |
| - SaFiO2 (ratio) | 173 (142-233) | 186 (157-238) | 0.467 |
| NIRS ventilatory parameters at starting of second NIRS | |||
| - HFNC total flow (l/min) | NA | 60 (50-60) | NA |
| - HFNC FiO2 (ratio) | NA | 0.50 (0.40-0.60) | NA |
| - NIV PS (cmH2O) | 8 (4-10) | NA | NA |
| - NIV FiO2 (ratio) | 0.50 (0.40-0.65) | NA | NA |
| - NIV PEEP (cmH2O) | 8 (6-9) | NA | NA |
Data expressed as frequencies and percentages [n(%)] or medians and interquartile ranges (IQR or 25th-75th percentile).
NIRS: non-invasive respiratory support, HFNC: high flow nasal cannula, NIV: non-invasive ventilation, FiO2: fraction of inspired oxygen, RR: respiratory rate, Bpm: breaths per minute, SatO2: peripheral oxygen saturation, SaFiO2: SatO2/FiO2 ratio, PS: pressure support, PEEP: positive end-expiratory pressure, ABG: arterial blood gases, PaCO2: carbon dioxide partial pressure in arterial blood gas sample, Pa02: oxygen partial pressure in arterial blood gas sample, HCO3-: bicarbonate.
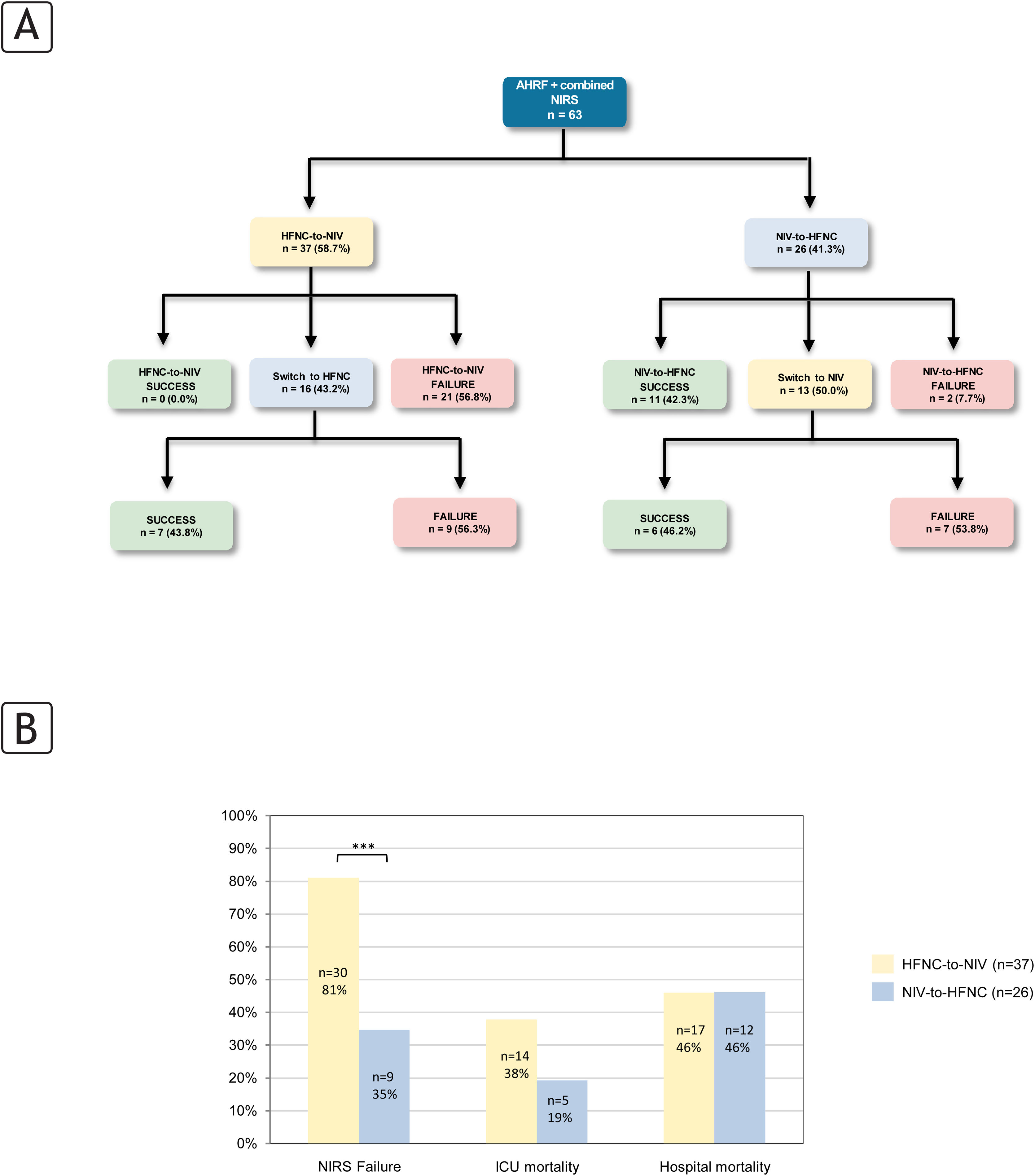
Fig. 2 shows failure and mortality rates of patients included in both study groups. Briefly, while there were a higher percentage of patients who directly failed after the first NIRS change in the HFNC-to-NIV group than in the NIV-to-HFNC (56.8% vs. 7.7%, p < 0.001), no differences were found after the second NIRS change in both groups (56.3% vs. 53.8%, p = 0.897) (Fig. 2A). Overall, HFNC-to-NIV patients had a higher rate of NIRS failure compared to NIV-to-HFNC patients without significant differences in ICU or hospital mortality (Fig. 2B).
Flowchart and patients’ outcomes related to study groups. (A) First and second switch detail, (B) global failure analysis based on first NIRS choice.
AHRF: acute hypoxemic respiratory failure, NIRS: non-invasive respiratory support; HFNC: High Flow Nasal Cannula; NIV: non-invasive ventilation.
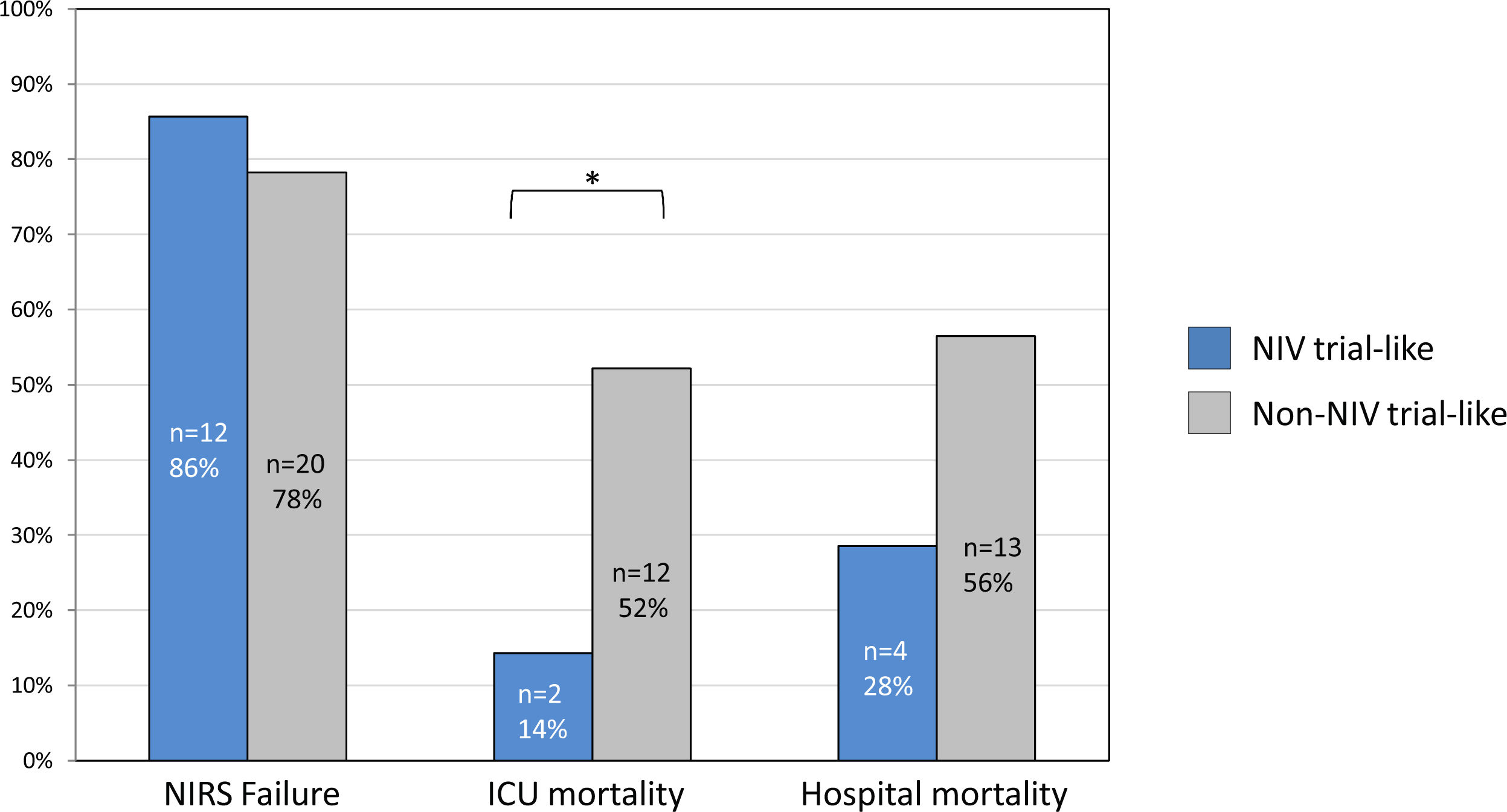
A total of 14 patients (37.8%) were classified in the NIV trial-like group, while 23 patients (62.2%) in the non-NIV trial-like group. Main clinical characteristics and data related to timings underwent NIRS are shown in OS Table 1 (Supplementary material). Although not statistically significant, there were 5 patients with a DNIO in the non-NIV trial-like group, while there were none in the NIV-trial-like group (p = 0.061).
Fig. 3 shows the differences between both groups regarding NIRS failure and ICU and hospital mortality rates. There were no significant differences in NIRS failure rates between the NIV trial-like and non-NIV trial-like groups. ICU mortality was statistically significantly lower in the NIV trial-like group compared to the non-NIV trial-like group and the hospital mortality rate also showed a trend towards being lower in the NIV trial-like group, but it did not reach statistical significance. Among those who presented NIRS failure, the ICU mortality rate was significantly lower in the NIV trial-like group compared to the non-NIV trial-like group (16.7% vs. 66.7%, p = 0.007). The hospital mortality rate was also lower in NIV trial-like group, but it did not reach statistical significance (33.3% vs. 66.7%, p = 0.073). This difference persisted when excluding patients with a DNIO from the analysis, with the ICU mortality rate being 16.7% vs. 57.1%, p = 0.034. OS Fig. 1 (Supplementary material) provides a detailed overview of the time course of NIRS therapies stratified by following or not a controlled NIRS switching strategy (NIV trial-like), including the timing and outcomes (IMV, ICU and hospital mortality). In this Figure, all patients are aligned at the initiation of NIV, with previous therapies displayed to the left and subsequent therapy courses to the right from that reference time point.
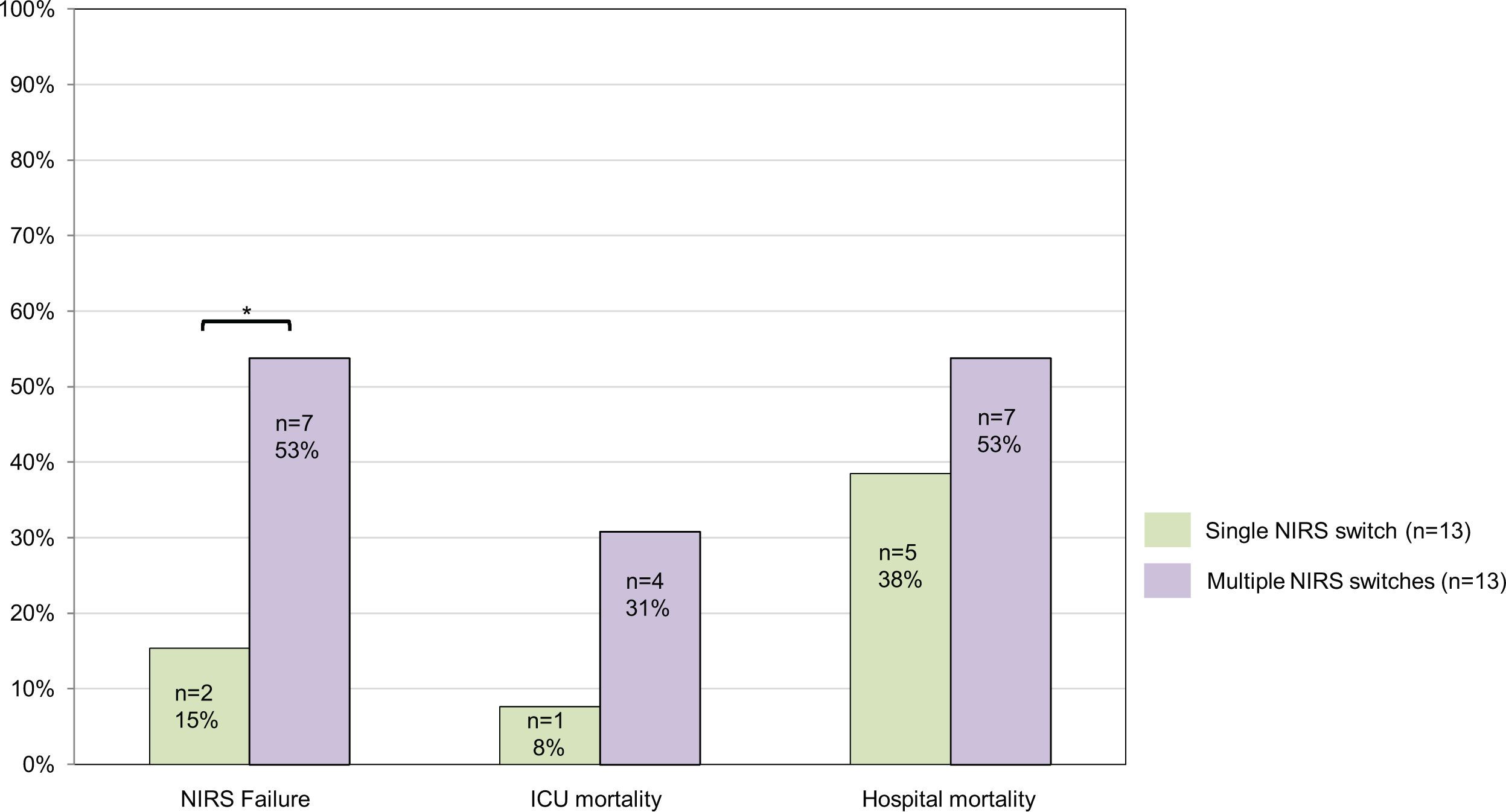
Single NIRS switch vs. multiple NIRS switches within NIV-to-HFNCA total of 13 patients (50.0%) were classified in the single NIRS switch group, while 13 patients (50.0%) in the multiple NIRS switches group. Main clinical characteristics and data related to timings underwent NIRS are shown in OS Table 2 (Supplementary material).
In 62% of patients from the multiple NIRS switches group, worsening was the reason for the second switch, of which 63% were due to the unresolved cause of AHRF that initially prompted the start of NIRS. The rate of NIV failure was lower in the single NIRS switch group compared to the multiple NIRS switches group, as well as the ICU and hospital mortality although without significant differences (Fig. 4). Moreover, they also presented a shorter ICU LOS (5 [2-8] vs. 12 [8-30] days, p = 0.001). OS Fig. 2 (Supplementary material) provides a detailed overview of the time course of NIRS therapies, including the timing and outcomes (IMV, ICU and hospital mortality) for patients with a single switch from NIV-to-HFNC and those who underwent multiple switches.
DiscussionIn this study we evaluated the combined use of NIRS (HFNC and NIV) in patients admitted to the ICU due to AHRF, determining the reasons for switching NIRS and evaluating the association of controlled strategies with clinical outcomes in these patients. The key findings of our study are as follows: 1) combined NIRS strategies is used in 32.5% of patients with AHRF needing NIRS; 2) clinical worsening is the main reason for switching from HFNC to NIV which is associated with higher rates of NIRS failure; in contrast, the main reason for switching from NIV to HFNC is clinical respiratory improvement, with a lower rate of NIRS failure; 3) following controlled NIRS switching strategies when combined NIRS is used, could be related with better outcomes.
Very few studies have been published on NIRS switches. Moreover, they do not discuss the impact of NIRS switch as a management strategy for AHRF, but rather as a rest tool for NIV (using HFNC during resting periods) or they analyze switches in different scenarios such as COVID-19 pandemics31 or during the weaning phase of mechanical ventilation in the post-extubation period.18,19 Recently, Marin-Corral et al.31 have published a Spanish multicentric study including 3889 COVID-19 patients describing the use of initial NIRS (HFNC or NIV) and their subsequent changes.31 Their results showed that 43% of critically ill COVID-19 patients initially underwent NIRS, 75% of them HFNC and 25% NIV. Moreover, among those severe patients who underwent NIRS due to COVID-19 AHRF, 11% were on combined NIRS strategies, being slightly more frequent the switch from HFNC to NIV (52.8%) than NIV to HFNC (47.2%). However, there are important limitations that do not allow us to compare these results. Importantly, in the COVID-19 scenario pandemic overload meant that decisions had to be made based on resource availability, including switches of NIRS strategy in order to reserve IMV for refractory cases. In this context, further research will be needed to evaluate the impact of pandemic in the future habits on the management of these patients in our environment.
Our study shows that the main reason for switching from HFNC to NIV is the clinical worsening of the patient, leading to an escalation in respiratory support. This is consistent with findings in the literature.32–35 Studies comparing HFNC with NIV have shown improved oxygenation with NIV but no reduction in work of breathing, as indicated by respiratory rate or inspiratory effort.15,36,37 Therefore, it would make sense to switch from HFNC to NIV during AHRF to improve hypoxemia. However, as there is not always an improvement in work of breathing (WOB) with NIV, it is logical that the failure rate of NIV is quite high. This may be because a significant percentage of patients experience a transient improvement in oxygenation without sufficient mechanical support, leading to a lack of improvement in respiratory mechanics.
High failure NIRS rates in patients switching from HFNC to NIV due to clinical worsening could suggest not recommending this strategy when HFNC fails. However, a different scenario arises when a NIV trial is performed as a controlled monitoring of NIRS in these patients. As previously described by Tomii et al., patients who undergo a NIV trial during AHRF of various causes, instead of proceeding directly to IMV, have a higher survival rate compared to those who do not undergo a NIV trial.38 Additionally, delayed intubation resulting from any NIRS intervention is known to be associated with increased mortality.6,39–41 In our study we retrospectively inferred those patients that could be treated following or not a controlled NIRS strategy based on NIV-trial criteria. In agreement with previous findings, our results suggest that a NIV trial after switching from HFNC therapy could be related with better outcomes decreasing the mortality rates in these patients undergoing both NIRS therapies. Therefore, based on our data, in those patients initially treated with HFNC who need switching to NIV, we recommend establishing thorough monitoring of the patient during the first 4−6 h of NIV use (to perform a NIV-trial). If clinical improvement does not occur during this period, it should be considered the endotracheal intubation and initiation of IMV to avoid unnecessary delays that could increase mortality.
Our results also show that the switch from NIV to HFNC is associated with clinical improvement in the patient, making it a potential therapeutic de-escalation. Despite HFNC providing lower oxygenation than NIV, in the context of clinical improvement and therefore improved oxygenation, a de-escalation to HFNC makes sense. Furthermore, it is widely recognized in the literature that HFNC is better tolerated than NIV.42 Therefore, once a patient improves with NIV and has lower oxygen requirements, transitioning to HFNC can increase comfort and tolerance to NIRS.3 In a different scenario, if the patient deteriorates while already on HFNC after NIV, and is switched back to NIV, the outcomes are not as favorable. In this situation, based on our results, the failure rate of NIV increases; and both ICU and hospital mortality also tend to increase. No specific recommendations can be made based on our findings; however, according to the results of the NIV-trial, applying NIV under strict supervision could be considered a valid therapeutic option.
This study has several limitations that should be acknowledged. First, it is a retrospective, single center study with a small sample size. It should be noted that although the study was retrospective, all the data analyzed were transferred directly and prospectively to the data management system of our ICU, and all the patients were treated by a homogeneous medical staff team. Then, all patients included in this study were thoroughly and comprehensively analyzed throughout their entire course, with detailed hourly assessments from their arrival at the ICU until their discharge, transfer, or death. Therefore, despite being retrospective, the detailed hourly analysis of each patient was specific and meticulous. Second, our patients did not undergo a prospective NIV trial; instead, it was inferred based on extensive and detailed clinical data collected after initiation of NIV and the clinician’s approach to the indication for initiation IMV. Third, the guidelines on respiratory failure, including guidelines on acute hypercapnic respiratory failure, do not provide specific details about the characteristics of an NIV trial. They only specify that if NIV fails, it should be discontinued and that the trial should be of short duration (without specifying the time). In this regard we have used the clinical criteria most used in previous studies where a NIV trial was used.23,43
ConclusionsIn conclusion, this study demonstrates that NIRS combination is used in real life and that both switches’ strategies, HFNC to NIV and NIV to HFNC are common in AHRF transitioning from HFNC to NIV is suggested as a therapeutic escalation and in this context performance of a NIV-trial could be beneficial. Conversely, switching from NIV to HFNC is suggested as a de-escalation strategy that is deemed safe if there is no evidence of NIRS failure. Further research is needed to elucidate the impact of the NIRS switch strategy in patients with AHRF.
Authors’ contributionsFJPG, JMC and JRM conceived and designed the study.
FJPG, JMC, AC, PPT, LP, JRB and MCG contributed to patient recruitment.
FJPG, JMC, OF, MIR and JRM made important intellectual contributions and actively participated in the interpretation of the data.
FJP and JMC wrote the paper.
AC, PPT, LP, OF and MIR made contributions to the writing and conceptual presentation of the results.
All authors contributed to critical examination of the paper for important intellectual content and approval of the final manuscript.
Conflict of interest statementsJRM: grants and non-financial support from Fisher & Paykel, personal fees from Dextro.
None of the other authors have any conflicts of interest to declare.
Role of funding sourceNo funding was received for this study.
Funding and role of the sponsorsNo funding was received for this study.
Ethics committee approvalThe institutional review board of PSMAR approved the original study (IRB Ref 2020/9050).
We thank Victor Boutonnet, Llesmil Ahuirand, Tomás Boutonnet and María Miñana for help with the data processing and Victor Fanjul for statistical support.