This review focuses on fluid management of critically ill patients. The topic is addressed based on 10 single questions with simplified answers that provide clinicians with the basic information needed at the point of care in treating patients in the Intensive Care Unit. The review has didactic purposes and may serve both as an update on fluid management and as an introduction to the subject for novices in critical care.
There is an urgent need to increase awareness regarding the potential risks associated with fluid overload. Clinicians should be mindful not only of the indications for administering fluid loads and of the type of fluids administered, but also of the importance to set safety limits. Lastly, it is important to implement proactive strategies seeking to establish negative fluid balance as soon as the clinical conditions are considered to be stable and the risk of deterioration is low.
Esta revisión se centra en el manejo de fluidos en el paciente crítico. Discutimos el tema con un enfoque basado en 10 preguntas individuales con respuestas simplificadas, que ofrecen al personal clínico la información básica necesaria, a pie de cama, para tratar a los pacientes en las unidades de cuidados intensivos. Esta revisión tiene propósitos didácticos y puede servir tanto como actualización sobre el manejo de fluidos como una introducción al tema para los que comienzan a tratar a pacientes críticos.
Existe una necesidad urgente de aumentar la conciencia sobre los riesgos potenciales asociados con la sobrecarga de líquidos. Los médicos deben tener en cuenta no solo las indicaciones para administrar una carga de fluidos, sino también el tipo de fluidos administrados y la importancia de establecer límites de seguridad. Finalmente, es necesario implementar estrategias proactivas que tengan como objetivo un balance negativo de líquidos tan pronto como las condiciones clínicas del paciente crítico se consideren estables y el riesgo de deterioro sea bajo.
The purpose of this short review is to answer ten key questions regarding the administration of intravenous fluid in the intensive care (ICU) setting, a topic that is receiving growing attention for the increased awareness on the potential risks associated with fluid overload. The decision to infuse fluid in order to revert acute circulatory dysfunction leading to shock is based on a basic physiological concept: a symptomatic fluid loss (absolute or relative) should be replaced to revert symptoms. Fluid resuscitation in the context of circulatory shock is focused on aggressive and rapid fluid infusion (eventually associated with the administration of systemic vasopressors) in order to restore blood pressure. The target of rapid fluid administration is to improve cardiac preload, and consequently cardiac output and peripheral perfusion.1,2 While aggressive and prompt fluid resuscitation in the early phase of shock is a recommended intervention,2,3 hemodynamic targets in already resuscitated patients and safety limits indicating whether or not fluid infusion should be considered are not well-defined yet.2,4 Indeed, once hemodynamic stability has been reached, fluid management should be tailored. It is overtly evident that a targeted fluid management is of pivotal importance to improve the outcome of critically ill patients, as both hypovolemia and hypervolemia are harmful.1 Clearly hypovolemia may lead to decreased organ perfusion, but the side effects of fluid overload are increasingly recognized. Table 1 summarizes these side effects at different organ level.
Systemic effects of fluid overload.
| Organ/system | Some effects of fluid overload |
|---|---|
| Central nervous system | Jugular vein congestionIncreased backward venous pressure affecting brain perfusionElectrolyte shifts and increase in cerebral edemaRisk of worsening neuronal damage (i.e. in TBI patients) |
| Respiratory | Worsening gas exchanges and pulmonary edemaProlonged time to liberation from MV and increased incidence of VAPPleural effusions and increased need for thoracentesis |
| Cardiovascular | RV volume and/or pressure overloadPulmonary edema secondary to LV diastolic dysfunctionLV dilatation especially if pre-existing impaired LV systolic functionDisturbance in cardiac conduction and arrhythmias |
| Renal, hepatic and gastrointestinal | Increased splanchnic congestion with worsening splanchnic perfusionIncreased need for diuretic therapy and/or RRTWorsening hepatic functionIncreased risk of intra-abdominal hypertension and abdominal compartment syndrome |
| Skin and muscles | Increased tissue edema with impaired peripheral perfusionCompromised wound healing and development of pressure ulcersLoss of muscular tissue, decreased mobility |
For such reasons, ICU clinicians should be aware of the indications for administering fluids in the already resuscitated critically ill patients, possibly pursuing a standardized approach as both the amount of fluids and the rate of administration influence the cardiovascular response. When deciding to administer fluids to the critically ill patient, it is pivotal to set the limits of safety for fluid challenges, understanding the risks associated with even small amounts of extra fluids. Furthermore, it is becoming relevant for ICU clinicians to implement pro-active strategies aiming at negative fluid balances already in the initial phase of recovery from critical illness. Moreover, several types of fluids are available for clinical use. Although the existing evidence is currently supporting the use of crystalloid solutions in most ICU patients, there is not an “ideal” fluid for all patients and, as for many other medical treatments, “one size does not fit all”.
- 1.
How intravenous fluids should be defined? Fluids should be considered as drugs.
This is an easy and short answer. Fluids are drugs and therefore, physicians should be aware of the same limitations as they are for any other medication used in clinical practice: clear indication, precise amount to be administered at a set rate, and safety issues that may prompt stopping administration if undesired side effects occur. Such a drug, the hemodynamic effects of fluid administration may be assessed by considering the pharmaco-dynamic analysis of fluid challenge.5 In other words, the dose and the rate of administration of a fluid challenge may produce a different impact on right ventricular filling and, in turn, on the rate of fluid responders (FR). These aspects have been not entirely explained and, as a matter of facts, fluid challenge amount and rates for their administration are not fixed.6,7 As for other drugs such as antibiotics, fluids utilization have been described according to the four “D's”: drug, duration and dosing and de-escalation, with the latter receiving increasing attention over the recent years.8 As expected, the rate of complications with fluid therapy increases with under- or over-dosing and targeting the correct fluid balance remains a clinical challenge, as one size does not fill all patients and/or conditions.9
- 2.
What a fluid challenge is? The fluid challenge is a test to assess “preload responsiveness”.
Fluid challenges should be distinguished from the fluid bolus (or fluid loading). The latter refers to the administration of a large volume of fluid given rapidly for rescue purposes to reverse an acute hemodynamic instability and often performed without close hemodynamic monitoring. On the other hand, a fluid challenge represents a test performed to assess the hemodynamic effects of a definite (lower) amount of fluids administered in the belief that it will increase the mean systemic filling pressures, which is the driving force for the venous return. Physiologically, improving preload conditions with fluid administration will increase the stroke volume (SV). A positive response to fluid administration generates a significant increase in SV, it is called “fluid responsiveness” (FR) and it is present in healthy individuals and of course in patients with circulatory shock.10 Therefore, in patients with “preload-responsiveness” (physiologically better defined as “bi-ventricular responsiveness”), a fluid challenge will increase preload and in turn SV and cardiac index (CI). On the other hand, a “fluid unresponsive” patient will not significantly increase the SV after fluid administration, and inappropriate fluid administration is likely contributing to venous congestion and fluid overload.
In other words, the fluid challenge should be administered only under preload-dependency condition (i.e. cardiac performance laying on the step part of Frank-Starling curve, see further), in already resuscitated patients. The decision to administer fluids assumes that the plateau of cardiac performance as described by the Frank-Starling curve has not been reached; in other words, the heart is performing in the steep part of the curve, when an increase in preload is followed by an increase in the SV. However, the clinical assessment of the position of patient's cardiac performance in the Frank-Starling curve is rather complex, and this evaluation at the ICU bedside for the prediction of FR is not always used.11
It is pivotal to understand that administration of fluids is a “non-reversible” action and the risk of fluid overload is behind the corner. Considering the negative impact on patient's outcomes of fluid overload both in the ICU setting12–15 and in the surgical patient,16 whenever feasible clinicians should evaluate FR before giving a fluid challenge. Therefore, an advanced hemodynamic monitoring should be in place (or echocardiography should be performed) as the assessment of FR cannot rely only on arterial blood pressure measurements.17 Once again, the evaluation of FR and the administration of a fluid challenge applies to the already resuscitated and properly monitored ICU patients. On the other hand, evaluating FR is challenging during the resuscitation of the hypotensive patients in the emergency department as in most cases invasive hemodynamic monitoring is not yet in place. In these cases, fluid boluses (loading) are performed under the assumption that the patient is in the steep part of the Frank-Starling curve, as long as there are not obvious contraindications to fluid administration.
As a matter of fact, preload responsiveness does not necessarily imply the need of fluid administration to improve tissue perfusion (see further, question n 7).
- 3.
When should I give a fluid challenge? The fluid challenge should be given to a responsive patients needing stabilization with limited risk of overload.
The fluid challenge is a diagnostic approach to hemodynamic management which aims at identifying the patients who respond to fluid administration with an increase in SV and CI. Unfortunately, in the clinical practice fluid challenges are still given with large worldwide variability in the indications, amount, rate and safety limits adopted (if any!) both clinically11 and in research studies.6
From theoretical perspectives, in presence of signs of tissue dysoxia (see Table 2), fluids are given in order to improve oxygen delivery (DO2) through an increase in SV and CI in the presence of the following three conditions:
- •
signs of hemodynamic instability and/or hypo-perfusion (high or increasing values of lactates, prolonged capillary refill time and skin mottling, increased CO2 gap, abnormal ScvO2),
- •
FR (often described as “preload responsiveness”, possibly better if reported as “biventricular responsiveness”),
- •
limited risks of fluid overload, so that the fluid administration has a low risk of worsening tissue perfusion (i.e. aggravating peripheral edema), gas exchanges (increase in extravascular lung water) and/or cardiac performance (i.e. right ventricular dilatation).
- 4.
Does an increase in cardiac index after fluid administration mean improving the DO2? This is not always the case.
Assessment of tissue dysoxia at the bedside.
| Advantages | Drawbacks | Clinical utility | |
|---|---|---|---|
| CRT and Skin mottling | -Easy to perform-Costless | -Both are operator dependent and affected by ambient and skin temperature-CRT is influenced by the different duration of pressure applied. Best method for performing CRT is still debated-Skin mottling is of difficult evaluation in patients with dark skin | Both are part of a simple clinical examination at bedside. If CRT ≤2s, should be considered normal, higher values may indicate perfusion defects. Skin mottling may be equally helpful but should be evaluated with a standardized scale (from 0 indicating no mottling, to 5 where extremely severe mottling area going beyond the fold of the knee) |
| Lactate | -Available as POC-Reference value available-Does not distinguish the etiology of shock | -Normal values do not exclude acute circulatory dysfunction-Not a direct measure of tissue perfusion-Systemic values affected by clearance and by overall perfusion | Lactate normalization may indicate successful resuscitation.Persistence of severe hyperlactatemia for a prolonged period is associated with negative prognosis. |
| ScVO2 | -Available as POC-Reference value available-May help distinguishing between causes of shock | -Need for a CVC in the superior cava vein (or a pulmonary artery catheter, in which case a sample for evaluation of SVO2 can be performed).Normal or high values are less indicative of the degree of shock. | The optimization of low ScVO2 (<70%) has been successfully used in a protocolized approach to septic shock. |
| ΔPCO2 | -Available as POC-Reference value available-May help distinguishing between causes of shock | -Need for both arterial and central venous blood gas analysis-Need for a CVC in the superior cava vein and of an arterial catheter or sample. | High values (>6mmHg) can identify inadequately resuscitated patients (insufficient blood flow to the tissues). |
CRT, capillary refill time; ScVO2, central venous oxygen saturation; ΔPCO2, the venous-to-arterial CO2 tension difference; SBP, systolic blood pressure; MAP mean arterial pressure; CO, cardiac output; CVC, central venous catheter; ICU, intensive care unit.
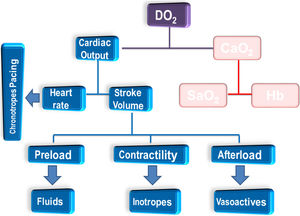
Clinicians should be aware of three main factors interposing between an improved DO2 and the oxygen utilization. First, as shown in the left side of Fig. 1, an increase in CI will ultimately contribute to an improved DO2, providing that the arterial concentration of oxygen (CaO2, right side of figure) remains unchanged. Fluid administration causes some degree of hemodilution with drop in hemoglobin levels; moreover, in case of elevated lung permeability also the oxygen saturation (SaO2) may drop. As example, the indexed DO2 in a patient with Hb=9g/dl, SaO2=97% and CI=2.7L/min is 316ml/min/m2. Assuming a good hemodynamic response to the administration of fluids (ΔCI=+15%, CI=3.1L/min), if a concomitant drop in both Hb (i.e. 8.4g/dl) and SaO2 (95%) occur, then the ultimate increase in DO2 will be marginal (indexed DO2=331ml/min/m2).
Factors conditioning the oxygen delivery (DO2) to tissues and interventions from hemodynamic perspectives. The right side of the figure is intentionally left in shadow as the focus of the review is not the approach from transfusion and ventilatory perspective. CaO2: arterial concentration of oxygen; Hb: hemoglobin; SaO2: saturation of oxygen.
Second, a straightforward assumption that increasing CI translates into greater DO2 has a pitfall in the role of the microcirculation. Indeed, the percentage of perfused vessels (study of microcirculation using microscopy) does not always follows linearly the increases in CI.18 In practice, the macro/micro-circulation coherence is not always preserved with large variability in the microcirculatory response at the end of fluid challenge.19 While in some patients an increase in CI produces recruitment at microcirculatory level, in others the fluid redistribution and the interstitial leakage of fluids may decrease O2 diffusion, potentially worsening the DO2.
Finally, a third limitation is beyond the microcirculation and relies on alterations at cellular level and in particular on the mitochondria ability to uptake and properly use the O2 delivered. The most typical case is seen in septic patients where O2 extraction and utilization at cellular level is profoundly impaired.20
- 5.
How fluid-responsiveness should be assessed in clinical practice? Fluid-responsiveness should be assessed using dynamic variables, being aware of the limitations of each test
While it seems clear from scientific perspective that static hemodynamic parameters (such as central venous pressure, CVP) have poor performance21 and should not be used to assess FR in critically ill patients, several dynamic parameters have been investigated and are potentially useful. In this regard, the heart-lung interaction during positive pressure ventilation plays a pivotal role in the interpretation of hemodynamic variations. Indeed, the swing in intra-thoracic pressure during mechanical ventilation and the consequent cyclic changes in venous return are a pre-requisite for most tests of FR.
The most studied index for FR evaluates the cyclic variability of pulse pressure (difference between systolic and diastolic arterial pressure), and the possibility of FR is most commonly considered when pulse pressure variation is ≥13%.22–25 A similar concept applies to the variability in SV (requiring advanced hemodynamic monitoring or echocardiography) with a slightly lower threshold to identify FR.21,23 However, these two tests can be trustworthy only in a minority of ICU patients, since their reliability relies on presence of sinus rhythm, controlled mechanical ventilation with no spontaneous breathing efforts, tidal volume ≥8ml/kg of ideal body weight, lung compliance ≥30ml/cmH2O, and no increase in intra-abdominal pressure (as main limitations).26
Clinicians should be aware that, when ventilating with low tidal volumes (i.e. 6ml/kg), there is an option to perform a tidal volume challenge technique for assessing FR, as described by Myatra and colleagues.27 The authors tested the hypothesis that absolute changes in pulse pressure variation or in SV variation produced by an increase in the tidal volume from 6 to 8ml/kg for only one minute would discriminate FR from non-responders.27 As the widespread use of protective ventilation would impair the performance of several dynamic tests, the tidal volume challenge test may offer the opportunity to evaluate FR even in these patients, decreasing the risk of falsely negative results.28 However, it should be noted that this promising test has been evaluated in a small-sized single center study,27 or on elective neurosurgical patients in the operating room.29
The echocardiographic evaluation of the variation in inferior vena cava diameter has received a great attention due to the increasing use of critical care echocardiography.30 However, its reliability seems lower than thought before,31,32 and it shares many limitations as the above described tests. Similarly, variation in superior vena cava with trans-esophageal echocardiography may be used in selected patients.33 Unfortunately, also these index showed limited clinical applicability, when applied in a large ICU population.34
When limitations preclude the use of these tests, ICU clinicians should keep in mind the applicability of two other options: the passive leg raising and the end-expiratory occlusion test. These maneuverers have different hemodynamic impact, and for the correct interpretation of their cardiovascular effects an advanced hemodynamic monitoring should be in place measuring the CI. Importantly, clinicians should remember that cut-offs for defining fluid-responsiveness is 15% variation in CI for passive leg raising and only 5% for end-expiratory occlusion test. More details on these tests are provided elsewhere35,36; we would like to remind the importance of maneuvers as these ones that do not require fluid administration and therefore have the advantage of being reversible (fluid are not given and there is no risk of overload due to these tests).
- 6.
If an indication to give fluid exists, how should I give them? I should give fluids closely monitoring effects (and safety limits), and standardized approach
Once the FR has been evaluated and provides indications for a fluid challenge, we suggest that clinicians follow the same approach they use for any drug prescription, having a clear idea on
- •
the type and amount of fluid to be given,
- •
the rate of administration, and
- •
what are the safety limits to stop infusion.
Moreover, it would be ideal to agree and standardize the practice of performing fluid challenges within each group of ICU. The type of fluid is a complex decision and may vary according to patient's characteristics, underlying disease and concomitant electrolyte/metabolic conditions (see further questions 8 and 9). Although there is no established recommendation on the amount of fluids that should be used, the proportion of FR to fluid challenges varies greatly according to the amount given, as shown in a recent study on postoperative cardiac patients (1ml/kg: 20%; 2ml/kg: 35%; 3ml/kg: 45%; 4ml/kg: 60%, in all cases given in 5min).37 Moreover, a systematic review showed that the rate of administration may play a more important role and the proportion of FR is lower in studies performing a fluid challenge in more than 30min.7 This is probably due to the increased redistribution/leak in critically ill patients over longer periods of administration. Although no guidelines has been established, it is authors opinion that fluid challenges should be given in reasonable amount (4ml/kg) and in a relatively short timeframe (5–10min), possibly adopting a standardized approach in each ICU. Safety limits (i.e. monitoring an abrupt increase in CVP is a possible safety limit during fluid challenge, especially if coupled with a no significant improvement in CI) should be always set in the mind of clinicians prescribing a fluid challenge. Moreover, while tests for FR are predictive measures, clinicians should perform the final evaluation on the result of their fluid challenge at the bed-space, keeping in mind that the largest variation in CI occurs within one minute of fluid challenge, and that effects on variation of CVP (safety measure) are lost after 10min.5
- 7.
When clinicians should be more careful in fluid administration? Several clinical conditions suggest a caution approach to fluid administration
Being “fluid-responder” in a test for “preload-responsiveness” is a physiologic condition and under conditions of tested FR, several circumstances should be taken into account when ultimately deciding if fluids should be given. Describing in details all the conditions where even a small extra amount of fluids can be harmful is beyond the scope of the present manuscript. However, we summarize the most common conditions that should be kept in mind by clinicians prescribing a fluid challenge.
- •
Right ventricular dysfunction: even a tiny amount of fluids may over-distend the failing right heart and in many cases it is very difficult to revert it. Moreover, right ventricular failure is associated with false positives in tests for FR.28
- •
Left ventricular diastolic dysfunction: in cases of increased left atrial pressure due to increased left ventricular filling pressures and diastolic dysfunction, an extra amount of fluid may worsen further the heart performance and, more importantly, it may further increase backward pressure on the pulmonary circulation with worsening oxygenation. Of note, diastolic dysfunction is associated with worse outcome in sepsis38,39 and higher failure in weaning from mechanical ventilation.40,41
- •
Acute lung injury: in case of increased lung permeability fluids easily move to the extravascular space with increase in alveolar water and deterioration of pulmonary edema. For this reason, patients with acute respiratory distress syndrome seem to benefit from a conservative fluid strategy approach.42,43
- •
Kidney injury: although de-hydration is a cause of acute kidney injury, most ICU patients are not de-hydrated. Clinicians should keep in mind that in case of already established kidney damage, the excess of fluid cannot be easily removed (i.e. by increasing does of diuretics), and renal replacement may be the only option. Moreover, an increased CVP and backward pressure on kidneys may decrease their perfusion pressure, creating a vicious circle.44
- •
Hepatic and Gastrointestinal: the effects of venous congestions produce similar issues at gastrointestinal and hepatic level, with the risk of worsening their perfusion. Patients at risk of intra-abdominal hypertension may experience aggravation of their clinical conditions with interstitial leakage of fluids.45
Of note, it has been recently tested the ability of a point-of-care ultrasound assessment of venous congestion (so-called “VEXUS), which focus on daily ultrasound assessment of hepatic, portal, intra-renal vein Doppler and inferior vena cava ultrasound. In a pioneer single-center study conducted during the first 72hours after cardiac surgery, the authors were able to identify five prototypes of venous excess combining the above ultrasound parameters.46 These findings deserve further attention and validation.
- 8.
Is there any differences between classes of crystalloids? Yes. Balanced solutions have better profile, but one size does not fit all patients.
Crystalloids are the most commonly used intravenous fluids, and although in a very simplified approach they can be classified in unbalanced and balanced solutions according to the concentration of electrolytes. The first group embrace solutions containing different concentration of sodium and chloride only (most commonly 0.9%, 3%, 7.5%) with strong ion difference equal to 0. On the opposite the group of balanced solutions have different electrolytes composition and a positive value of strong ion difference, ranging between 27 (Acetate Malate and Ringers’ solutions) and 50 (Acetate Gluconate solution). The detailed description of all the solutions is beyond the scope of the present manuscript, and readers are referred elsewhere.47
One of the greatest issues that should be considered at the bed-space when using unbalanced solutions (i.e. saline solution) is the higher load of chloride administered. This exposes the patient to greater risks of hyper-chloremic acidosis and renal injury.48 Two recent single-center, pragmatic, multiple-crossover trials from the same group of authors have recently compared balanced (Lactate Ringer or Acetate Gluconate) vs saline solution 0.9% in the ICU setting,49 or in non-critically ill adult patients admitted to the Emergency Department.50 In the study on ICU patients, the use of balanced crystalloids reduced the major adverse kidney events within 30 days (composite outcome of in-hospital mortality, new renal replacement therapy, and persistent renal dysfunction). Interestingly, these results were achieved despite a low amount of fluids given, with a median around 1000ml for both groups from admission to day 30 or discharge, whichever came first.49 In the study in non-critically ill adults, there were no difference in hospital-free days between groups but also in this study the group randomized to balanced crystalloids reported lower incidence of major adverse kidney events within 30 days (secondary outcome).50 These reported effects on kidney function may be explained by the dose-dependent hyper-chloremic acidosis as this condition favors the contraction of vascular smooth muscles, potentially reducing renal perfusion, causing harmful effects on renal function even at low doses.51 There is preclinical evidence that administration of saline solutions causes not only hyper-chloremic metabolic acidosis, but also inflammation, hypotension and acute kidney injury.52
It is apparent that, when deciding to administer a crystalloid solution, in most cases a balanced one may be preferred, but some peculiarities should be always kept in mind. As examples, these solutions contain potassium and could be contraindicated in case of renal failure and risk of dialysis; furthermore, these solutions are slightly hypotonic (range 277–304mOsm/L) and their use in patients with traumatic brain injury should be very cautious to avoid aggravation of cerebral edema.53 Moreover, lactate buffered solutions (i.e. Lactate Ringer) may potentially cause a small increases in serum lactate concentration, especially among patients with impaired hepatic function.54 Of note, the Surviving Sepsis Campaign recommends crystalloids as fluid of choice for initial resuscitation and subsequent intravascular volume replacement in patients with sepsis and septic shock with no specific indications between balanced or unbalanced solutions.2 As the present manuscript is written during the recent pandemic of coronavirus disease we remind readers that expert consensus for patients in shock suggests buffered crystalloid solutions over unbalanced55 and to take in high consideration the risk of renal injury.56
In summary, there is not an ideal solution fitting for all critically ill patients, as there is not an ideal antibiotic for all infections.
- 9.
Is there any differences between crystalloids and colloids? Yes, and there are important differences between types of colloids
Colloids have been introduced in the clinical practice because of their theoretical capability to remain longer in the intravascular space as compared to crystalloids, for the generation of higher osmotic pressure in the circulation due to the presence of macromolecules in the solution. Examples of colloids are albumin, hydroxyl-ethyl-starch (HES), gelatins and dextran. Albumin is a natural colloid dissolved in an unbalanced solution (saline), gelatins and HES (with the exception of the unbalanced Voluven®) are balanced solutions with a positive strong ion difference (range 28–56). Colloids particles are too large to pass semi-permeable membranes such as capillary membranes; thus colloids should theoretically remain longer in the intravascular space than crystalloids, possibly reducing the amount of fluids administered. However, one should keep in mind that such theoretical conditions are subverted in critically ill patients, where increased permeability, endothelial damage and several other factors affect the trans-membrane shift of fluids. Indeed, despite theoretical advantages, colloids have mostly failed in showing advantage in critically ill patients. Importantly, a differentiation should be made between natural colloids (albumin) and synthetic colloids.
Albumin – A landmark trial in 2004 showed that 4% albumin for fluid resuscitation in critically ill patients resulted in similar outcomes at 28 days as compared with saline solution 0.9%, despite albumin significantly reduced the overall amount of fluids given (saline solution to albumin administration ratio during the first 4 days was 1.4).57 Interestingly, the secondary analyses showed an increased risk of death in patients with traumatic brain injury, but on the contrary there was a trend toward lower mortality in septic patients receiving albumin (p=0.09). This led to the design of a randomized controlled trial in patients with severe sepsis comparing albumin 20% replacement (to keep plasmatic values ≥3g/dl) to crystalloids alone. The ALBIOS study (published 10 years later) showed that albumin did not improve the rate of survival at 28 and 90 days, but a reduction in 90-day mortality was seen in the post hoc analysis for the albumin group in patients with septic shock.58 There is conflicting evidence on the role of albumin in critically ill patients with sepsis. Two meta-analyses included studies in whom patients received crystalloids as well as synthetic colloids in the control arm, and showed no difference in the mortality rates between groups.59,60 On the contrary, a third meta-analysis including as control group patients receiving only crystalloids found that 90-day mortality of patients in septic shock was significantly lower with albumin.61
Synthetic colloids – In three large RCTs comparing synthetic colloids (HES) and crystalloids the ratio of crystalloids to HES administered has been mostly in the range of 1.0–1.2 (decrease up to 20% of the volume administered in the HES group), far less than expected.62–64 Only one RCT showed a more pronounced reduction in the volume of fluids administered in the HES group, with a ratio of 1.5.65 The small reduction in the volume of fluids administered does not seem clinically relevant and, on the contrary, it is counterbalanced by known side-effects of HES such as the renal injury.63,64 There also no data supporting advantages in long-term outcomes and cost-effectiveness analysis.66 In January 2018, the European Medical Agency safety committee recommended suspending the marketing authorizations of these medicines because they continued to be used in critically ill patients and patients with sepsis despite restrictions already introduced 5 years earlier.67 Although starches have been subsequently reintroduced on the market (provided that training, controlled access and warnings on the packaging are implemented), HES solutions have several contraindications (sepsis or critically illness, renal impairment or ongoing renal replacement therapy, severe coagulopathy, intracranial or cerebral hemorrhage, burn injuries, severe hyperkalemia, hypernatremia, hyper-chloremia, impaired hepatic function, congestive heart failure, organ transplant). The use of HES should be restricted to the initial phase of volume resuscitation and to acute blood loss when crystalloids alone are not considered sufficient.
- 10.
When should I start taking fluids off? As soon as possible if the patient is not at risk of shock
As already mentioned fluid overload is defined an increase in 10% of body weight from ICU admission.8,68–71 Regarding the approach with fluid therapy, progression of critical illness and fluid administration has been conventionally divided in four stages. The initial phase is represented by the “resuscitation” (or salvage) period where fluids are given in large amount to support end-organ perfusion and maintain vital signs during life-threatening conditions associated with impaired tissue perfusion. As result there is a rapidly growing curve of fluid balance. This period is followed by the “optimization”, a phase where fluid administration starts to be tailored according to targeted hemodynamic and perfusion variables, still with a trend toward more positive fluid balance. The third phase is known as “stabilization” and fluids are only used for ongoing maintenance. By this time the patient has reached the peak of cumulative fluid balance (curve of fluid balance plateaus), is not anymore in a shock state (or at imminent risk), and possibly some fluids are starting to be mobilized and removed.
The last phase is called “evacuation” (or de-escalation) and it lasts much longer than the previous periods, from days to weeks. It refers to late goal-directed fluid removal associated with conservative fluid management. Indeed, during de-escalation becomes important to achieve a negative fluid balance with elimination of fluid excess gained during the most severe stages of critical illness. De-escalation with fluid removal has been described as the fourth “D” of fluid therapy (together with “drug”, “duration” and “dosing”), likewise it happens for other drugs (i.e. antibiotics). During this period the oral intake should be promoted, and unnecessary intravenous fluids should be avoided. Retrospective evidence has suggested that negative fluid balance on day 3 of ICU stay accomplished with de-resuscitation is associated with improved patient outcomes.72 It is currently under investigation the role of conservative fluid administration and de-resuscitation in order to improve patients’ recovery after critical illness.73 In order to achieve negative fluid balance, clinicians pursuing aggressive de-resuscitation may use diuretics and eventually renal replacement therapy. However, they should balance the risk of being too aggressive with fluid removal as hypovolemia may trigger hemodynamic deterioration and hypo-perfusion with end-organ damage.
ConclusionsIn conclusion we provide a short summary with key question and answer aiming at increasing the basic knowledge on the fluid management of critically ill patients. The manuscript spans from the indications, the modalities of administration and the safety limits when deciding to perform a fluid challenges, and emphasizes the increasing awareness on the importance of active de-resuscitation.
Ethics approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Availability of data and materialNot applicable.
Authors’ contributionsFS and MA designed the review and the format, and wrote the initial draft. AM and MC critically revised the draft and made substantial changes. All the authors agreed on the manuscript content.
FundingNone.
Conflict of interestThe authors declare that they have no conflict of interest.