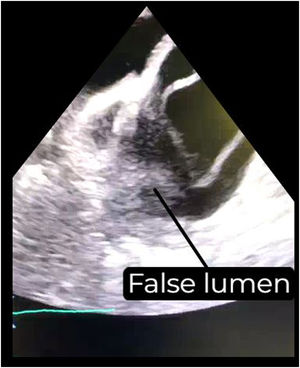
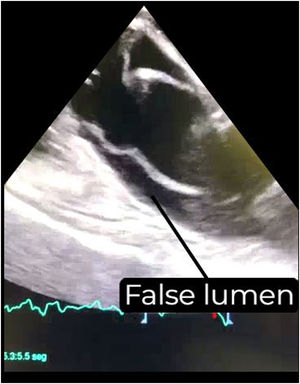
This is the case of a 67-year-old patient with a past medical history of abdominal aortic endoprosthesis who went into cardiac arrest after experiencing sudden chest pain. Upon arrival of the emergency medical services, ventricular fibrillation (VF) was recorded, which was defibrillated, while ST-segment elevation was observed in the left precordial leads. Afterwards, the patient experienced a second cardiac arrest, this time in asystole, leading to intubation and mechanical chest compressions as a possible myocardial infarction code. A transesophageal echocardiography (TEE) had to performed because there was no window of opportunity to perform a transthoracic echocardiography (TTE). The TEE revealed the presence of a type A aortic dissection with intimal flap in the mid-esophageal long-axis view of the aortic valve and ascending aorta (Videos 1 and 2; Figs. 1 and 2). Given the prolonged duration of cardiac arrest with this diagnosis, resuscitation maneuvers were ceased, resulting in the patient passing away 30min later, with an incipient intramural thrombus formation due to blood stasis (Video 3; Fig. 3).
Intra-arrest TEE in a patient with the airway isolated is an extremely useful tool to guide real-time and continuous resuscitation maneuvers and try to reach an etiological diagnosis. Its main limitation may be the time required to place the probe and the level of experience required. However, this can be reasonably overcome with training in simple acquisition protocols of a few views, as described in the medical literature.
Conflicts of interestNone reported.
FundingNone whatsoever.