Major burn injury triggers severe oxidative stress, a systemic inflammatory response, and a persistent hypermetabolic and hypercatabolic state with secondary sarcopenia, multiorgan dysfunction, sepsis and an increased mortality risk. Calorie deficit, negative protein balance and antioxidant micronutrient deficiency after thermal injury have been associated to poor clinical outcomes. In this context, personalized nutrition therapy with early enteral feeding from the start of resuscitation are indicated. Over the last four decades, different nutritional and pharmacological interventions aimed at modulating the immune and metabolic responses have been evaluated. These strategies have been shown to be able to minimize acute malnutrition, as well as modulate the immunoinflammatory response, and improve relevant clinical outcomes in this patient population. The purpose of this updating review is to summarize the most current evidence on metabolic response and nutrition therapy in critically ill burn patients.
La quemadura grave induce estrés oxidativo severo, respuesta inflamatoria sistémica, hipermetabolismo e hipercatabolismo severo y persistente con sarcopenia secundaria, disfunción orgánica, sepsis y mayor mortalidad. El déficit energético, el balance negativo de proteínas y la deficiencia de micronutrientes antioxidantes durante la agresión térmica están asociados a malos resultados clínicos. En este contexto, una terapia nutricional personalizada, priorizando la nutrición enteral precoz, está indicada desde el inicio de la fase de resucitación. En las últimas 4 décadas se han estudiado diferentes intervenciones nutricionales y farmacológicas moduladoras de la respuesta inmune y metabólica. Dichas estrategias han demostrado ser capaces de minimizar la malnutrición aguda, modular la respuesta inmunoinflamatoria y mejorar los resultados clínicos. El propósito del presente estudio de revisión es analizar la evidencia más reciente sobre la respuesta metabólica y la terapia nutricional en el paciente quemado crítico.
Critically ill burned patients are a model of trauma patient characterized by the early development of a state of hypermetabolism and severe hypercatabolism with an energy expenditure (EE) that can duplicate the EE at rest. These alterations can go on for months after the initial thermal aggression.1 The magnitude of this state depends on different biomolecular alterations keeping a direct relation to the extension of the total body surface area burned (TBSAB). On the other hand, thermal damage is an important cause of loss of macronutrients (proteins) and micronutrients (trace elements and vitamins) through the areas burned. The intense hypermetabolic and hypercatabolic response leads to developing acute malnutrition, secondary sarcopenia and acquired muscle weakness, which favors the appearance of infections, multiple organ dysfunction, sepsis, and eventually, death. On the other hand, the negative balance of antioxidant micronutrients during the thermal year promotes the development of oxidative stress, which maintains and perpetuates the aforementioned systemic inflammatory response, mitochondrial dysfunction, and metabolic alterations.
Back in 2015, Czapran et al.2 published the results of critically ill burned patients who required mechanical ventilation for over 72h and who were part of the International Nutrition Survey conducted between 2007 and 2011. The analysis of such results confirmed that these 90 patients had an estimated expenditure deficiency of 943±654kcal/d and an estimated protein deficiency of 49±41g/d2. On the other hand, these data reveal that 21% of the patients died within the follow-up period some 60 days after hospital admission at the intensive care unit (ICU), and those who died had higher energy (1.251±742 vs 861±607kcal/d, p=0.02) and protein (67±42 vs 44±39g/d, p=0.03)2 deficiencies.
For these reasons, the administration of the adequate metabolic and nutritional therapies is essential if we wish to promote the recovery of the critically ill burned patient by modulating his immunoinflammatory response and minimizing the acute malnutrition associated with his critical condition.3 In this sense, the implementation of an early, adequate, and individualized nutritional therapy has improved clinical results, especially by reducing the incidence of infectious complications, shortening hospital stays, and accelerating the process of healing the wounds.4 Consequently, nutritional therapy is the corner stone of the therapeutic strategy of the critically ill burned patient and should start at the phase of early resuscitation and go on while in the phase of healing and definitive rehabilitation. The goal of this review is to analyze our actual knowledge on metabolic alterations and nutritional strategies in critically ill burned patients, with special emphasis on aspects such as the targets of calories and proteins, the most recent evidence on pharmaco-nutritional and anticatabolic strategies in this population of critically ill patients.
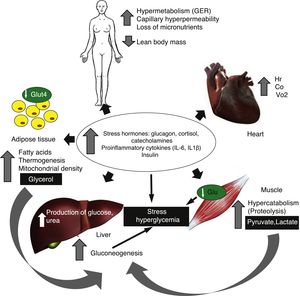
Energetic metabolism and inflammatory response in thermal damageTrauma causes systemic inflammation mediated by proinflammatory cytokines (interleukin IL-6, IL-1β, tumor necrosis factor TNF-α) and stress hormones that induce a significant and persistent hypermetabolic response. This response is characterized by an increased basal metabolic rate, cardiac output, myocardial oxygen demand, and also by the degradation of the muscle protein and insulin-resistance (Fig. 1).5 The hypermetabolic response induced by thermal aggression is characterized by an increased basal metabolic rate (up to 40% above normal values) with significant alterations of the mitochondrial function. In healthy individuals approximately two thirds of oxygen consumption is coupled with oxidative phosphorylation, and the remaining third is attributed to thermogenesis.5 In critically ill burned patients this ratio is reversed and one third of mitochondrial respiration is coupled with oxidative phosphorylation, while the remaining two thirds of total breathing dissipate as heat. This mismatch of mitochondrial oxidative phosphorylation in the skeletal muscle is a major contributing factor to the increased basal metabolic rate and also responsible for hypermetabolism.6,7 In that sense, Porter et al.8 showed that in these patients, the control of mitochondrial coupling is impaired, even two (2) years after thermal aggression with over 30% of the TBSAB, which is associated with a significant increase of thermogenesis. More recently, in one experimental model of thermal aggression, Szczesny et al.9 studied the modifications of mitochondrial bioenergetics and confirmed that they are time-dependent after the burn with reduced basal respiration and ATP turnover. Similarly, the authors of this study showed specific tissue damage on the DNA and, in particular, on the mitochondrial DNA of pulmonary tissue and cardiac striated muscle. Finally, this group studied the evolution of oxidative stress and the infiltration of neutrophils mediated by the activity of myeloperoxidase and confirmed that these effects were even more significant in the heart and lungs.9 This findings, added to the data derived from the study conducted by Porter et al.,8 confirm that, in the future, mitochondrial dysfunction may be a true therapeutic target in critically ill burned patients. However, such findings still need to be verified before conducting preclinical trials aimed at assessing the effectiveness and safety of these strategies.
Back in 2014, in one prospective cohort of 230 critically ill burned kids with over 30% of their TBSAB, Jeschke et al.10 showed that those individuals who would not survive to thermal damage had a more intense inflammatory response, shown by higher levels of IL-6, IL-8, granulocyte-colony stimulating factor, monocyte chemoattractant protein-1, C3 complement, α2-macroglobulin, haptoglobin, α1-acid glycoprotein and C reactive protein. Similarly, metabolic alterations were more significant in these patients with higher levels of glycemia, insulin, urea, and plasma creatinine. Finally, these authors showed that the EE at rest measured through indirect calorimetry was significantly higher among those who did not survive the critical burn. All these immunoinflammatory and metabolic alterations confirm that they are predictors of morbimortality in critically ill burned patients.10
The metabolism of glucoseDuring the early stages following the burn, the rate of production and oxidation of glucose, and poor tissue extraction from the burn may generate hyperglycemia and hyperlactatemia.11 Hyperglycemia (values >180mg/dl) is associated with adverse clinical outcomes such as hypercatabolism, hypermetabolism, delayed injury healing, higher incidence rate of infections and higher mortality.12,13 The thermal injury induces stress on the endoplasmic reticulum (ER) in the skin, and adipose and muscle tissue—a phenomenon associated with insulin-resistance.14 This stress on the ER is registered by different types of enzymes such as the inositol-requiring enzyme 1, the protein kinase RNA-like ER kinase, and the activating transcription factor 6; these proteins are responsible for transcription phenomena, genetic translation, deployment, translocation and protein secretion.15 Back in 2012, Jeschke et al.16 showed that the stress markers of ER remain high until 250 days after the aggression, which is consistent with insulin-resistance and stress hyperglycemia.
In these patients a moderate glycemic control (from 100 to 140mg/dl) with the use of IV insulin associates less glycemic variability and scarce risk of hypoglycemia, as it was confirmed by Stoecklin et al.17 in 229 adult patients seriously burned. Insulin mediates the glucose uptake in the adipose tissue and the skeletal muscle and inhibits hepatic gluconeogenesis. On the other hand, insulin modulates the production and release of proinflammatory cytokines (TNF-α and IL-1β) and anti-inflammatory IL-10, and the expression of adhesion molecules ICAM-1 and E-selectin.18 In this sense, therapy with IV insulin obtaining glycemia levels ≤130mg/dl seems to attenuate hypermetabolic response levels, since 140mg/dl are associated with reduced morbidity and mortality rates, which was already suggested by Jetschke et al.19 In the trauma patient, guidelines recommend initiating insulin therapy when glycemic levels reach ≥150mg/dl, which should be titrated in order to keep values <180mg/dl and especially <150mg/dl, thus avoiding hypoglycemia (values <70mg/dl).20
However, recently the concepts of diabetes paradox and, in particular, metabolic control have been introduced prior to the aggression by determining the levels of glycosylated hemoglobin.21 Thanks to this newly acquired knowledge, the objective range of glycemia while in critical condition will be determined by the value of glycosylated hemoglobin in such a way that levels >6.5–7.0 should make us be a little more tolerant with the objective range (160–220mg/dl); however, today, this phenomenon known as diabetes paradox and the new objective ranges have not been fully studied in critically ill burned patients.21
The protein metabolismSevere hypercatabolism generates sarcopenia, which is associated with organic dysfunction, muscle weakness, and higher mortality rates.22 In burned patients it is estimated that one square meter of burned skin causes a daily nitrogen loss (N) between 20 and 25g, leading to a 20–25% loss of lean body mass. Similarly, it has been estimated that the average loss of N in burned patients without nutritional therapy is more than 0.2g of N/kg/day (15–20g/day), leading to a 10% loss of body weight during the first week. This acute protein depletion is associated with immune dysfunction, scar tissue alterations, pressure ulcers, and a higher rate of infections.22
Hypercatabolic response is lower with the supply of exogenous insulin diverting the balance between synthesis and proteolysis, which basically happens in the skeletal muscle; in that sense, an increase of up to 400% in the protein synthesis with the supply of IV insulin has been reported. This insulin effect seems to be mediated by an increase in the transport of amino acids, and up to 500% increases in phenylalanine uptake have been reported.23 Similarly, non-nutritional strategies such as the use of propranolol increase the intracellular free amino acid recycling, which are reused during protein synthesis in the myocyte, and a higher phenylalanine uptake and protein fractional synthesis has been confirmed.19
The lipid metabolismThe burn is followed by fatty acid (FA) mobilization from the adipose tissue. Both lipolysis and the increase of FA flow toward the plasma are mediated by higher levels of catecholamines, glycagon, and adrenal corticotropin24; lipolysis becomes more significant between 5 days and 2 months after thermal aggression, being the alterations in the profile of fatty acids more evident between 7 and 10 days after the aggression. These alterations favor the inflammatory and immunosuppressive state that follows the burn. Also there is a persistent increase in the levels of glycerol, which translates into greater lipid peroxidation; similarly, most FAs are re-esterified, which is confirmed by the increase of LDL lipoproteins, triglycerides, and by the lower level of ketonic bodies.5 On the other hand, the analysis of the plasma FA profile shows an increase of saturated and monounsaturated FAs of proinflammatory action and reduced polyunsaturated FAs of anti-inflammatory profile. Finally, we should mention here that the increased lipolysis following the burn contributes to a higher morbimortality rate due to fat infiltration, particularly in the liver, which is associated with insulin-resistance.25
Oxidative stress and state of antioxidant micronutrientsBurns represent a model of oxidative stress with severe depletion of endogenous antioxidant defenses due to excessive urinary excretion and, through burned areas, of antioxidant micronutrients such as copper (Cu), selenium (Se) and zinc (Zn).26 This phenomenon is especially evident toward the end of the first week following thermal aggression. Similarly, capillary effusion due to systemic inflammation explains the redistribution of trace elements during the acute phase, reducing the antioxidant capability and damaging the mechanisms of tissue repair. Recently, in 15 patients burned with an average 29±25% of their TBSAB, Jafari et al.27 assessed the level of 12 trace elements in the exudates of the areas burned. For most micronutrients and, in particular, Se, Cu, Zn, boron (B), bromine (Br), iron (Fe) and iodine (I) the most significant losses happened during day one, with less losses reported after the first 24h.27
Also, these patients had vitamins A, C, D and E deficiencies; in this sense, during the last few years, the study of vitamin D has been very interesting in different populations of critically ill patients.28 Recently, in 318 burned patients, Blay et al.29 confirmed severe deficiencies (25-dihydroxyvitamin D<10ng/ml) in n=46 (14.5%), insufficiencies (10–29ng/ml) in n=207 (65.1%) while the remaining 20.4% of patients showed normal serum levels of vitamin D. In the group of patients with vitamin D insufficiency or deficiency, the authors confirmed longer ICU and hospital stays.29 These findings, added to the pioneering work conducted by Berger et al.,30,31 are responsible for the interest shown during the last 30 years trying to implement the strategy of providing antioxidant micronutrients to critically ill burned patients.
The route of nutritional therapyThe enteral route is the route of choice in critically burned patients;32 on this regard, the American Burn Association (ABA),33 and back in 2011, the Spanish Society of Intensive and Critical Care Medicine and Coronary Units and the Spanish Society for Parenteral and Enteral Nutrition (SEMICYUC-SENPE)34 recommend starting enteral nutrition as soon as possible. Similarly, the guidelines adopted by the Inflammation and Host Response to Injury (Glue Grant)35 recommend early enteral nutrition (EN) although the optimal time to start EN is never mentioned. Back in the year 2011, Moisier et al.4 confirmed that 80% of 153 burned patients started EN during the first 24h, while 95% during the first 48h. Early EN was associated with shorter ICU stays (p=0.03) and less aggressive infections of the injuries (p=0.01). Some studies have already shown that very early EN during the first 6–12h is safe, modulates the hypermetabolic response, reduces significantly the levels of catecholamines, cortisol, and glycagon, and increases the production of immunoglobulins.32,34 This nutritional strategy protects the intestinal barrier integrity, motility and splanchnic blood flow; also, as Vicic et al.36 confirmed, an early EN reduces the rate of infections, except for nosocomial pneumonia. However, and based on the actual evidence available, early EN in burned patients has not always given clinical benefits. Back in 2015, Guo et al.37 conducted a systematic review and one meta-analysis including 6 randomized clinical trials (RCT) of critically burned patients, and then proceeded to assess how early EN impacted relevant clinical outcomes in burned patients such as the injury infection rate, the duration of mechanical ventilation, the use of antibiotics, and the mortality rate. Although upon the authors¿ request this study was eliminated from PubMed and the journal electronic site, the analysis of results did not show any clinical benefits from early EN in adult critically ill burned patients.
On the issue of nutritional benefits in burned patients, back in 2015, Sudenis et al.,38 in a cohort of 90 burned patients with over 10% of their TBSAB showed that on day 1 after the burn, the effective supply of calories through enteral route was 19%, and on day 14 it was 91%, having the EN been initiated an average 9.5h after hospital admission.
However, an important aspect that may limit the use of the enteral route in burned patients is GI dysfunction, and intestinal failure due to abdominal hypertension, and eventually, abdominal compartment syndrome (ACS). In fact, the energic supply with fluids reduces the abdominal wall and paralytic ileus compliance that can lead to ACS. In that sense, the appearance of intestinal dysfunction contraindicates the enteral route and indicates parenteral nutrition (PN).39 On the composition of PN in burned patients, the type of lipid emulsion to use has been studied in different clinical trials. Back in 2005, García de Lorenzo et al.40 conducted one RCT in 22 critically ill burned patients where they studied one emulsion containing olive oil (ClinOleic® 20%, Baxter, France) compared to another 50/50 emulsion of LCT and MCT (Lipofundin® 20%, B. Braun, Germany). The group of patients who received the olive oil-rich emulsion showed less alterations in the hepatic function test, although no differences were seen in the acute phase parameters, the tolerability of PN, and the metabolism of fatty acids. Also, back in 2008. Mateu-de Antonio et al.41 conducted one retrospective study of 2 cohorts and analyzed the effects of a 100% soybean oil lipid emulsion (Intralipid® 20%, Fresenius Kabi, Spain) compared to an alternative emulsion rich in olive oil (ClinOleic® 20%, Baxter, Spain). The analysis of results did not show any differences between both groups in the incidence of infection, duration of ICU and hospital stays, or in the mortality rate, although the peak value of leukocytes was high (p=0.036) at the end of PN in the cohort that received the olive oil-rich lipid emulsion.41
Nutritional requirementsThe nutritional requirements of critically ill burned patients are high due to severe hypermetabolism and hypercatabolism. This is why the guidelines on nutritional therapy are based on optimizing the supply of calories and proteins, leading to better survival rates among these patients. The energy supply needed by every patient is different and is based on the patient's condition after suffering the thermal aggression, as Cunninghan42 confirmed in a review of studies that used indirect calorimetry to measure basal EE. This is why the EE needs to be assessed daily and individually, preferably using the indirect calorimetry procedure, which is actually considered the standard of reference today. However, this resource is not always available in burned centers, making the use of prediction equations a routine practice. Rimdeika et al.43 showed that the use of one predetermined value of 25–30kcal/kg of body weight may result in enteral hyponutrition, which is why this strategy is not recommended today.
On the use of prediction equations, the Toronto equation (Table 1) seems to be the most adequate one of all, since it estimates the variability of energetic requirements together with the course of the disease. In critically ill burned kids, the Schoffield equation has turned out to be the equation of choice.44 In this sense, several studies have shown that the increase of EE is more significant during the first stages of the burn, to later decline progressively.
Use of predictive equations in adult critically ill burned patients.
| Prediction equations for the assessment of energetic needs in critically ill burned patients |
| Toronto equation (results come close to indirect calorimetry) EER=(−4343+[10.5×% BSA]+[0.23×caloric intake]+[0.84×Harris Benedict]+[114×rectal temperature in °C]−[4.5×day post-burn]) |
| Carlson equation EER=BME×(0.89142+0.01335×TBSAB)×m2×AF |
| Harris-Benedict equation (the result should be multiplied by the stress factor [1.2–2.0]) |
| Men: 66.437+(5.0033×height [cm])+(13.7516×weight [kg])−age [years]) |
| Women: 655.0955+(1.8496×height [cm])+(9.5634×weight [kg])−(4.6756×age [years]) |
AF, activity factor of 1.25; BME, basal metabolic expenditure; m2, square meters of body surface; BSA, body surface area; EER, estimated energetic requirements; TBSAB, total body surface area burned.
Back in 2010 one retrospective, observational analysis of an heterogeneous population of critical patients that did not include burned patients showed that the mortality rate at 60 days was significantly lower when, on day 12, patients received 80–85% of the estimated caloric target.45 More recently, Nicolo et al.46 confirmed, in a group of critical patients of similar characteristics, reduced mortality rates when over 80% of the protein prescribed was administered on day 4 (odds ratio [OR]: 0.68; 95% confidence interval [CI]: 0.50–0.91) and day 12 (OR: 0.60; 95% CI: 0.39–0.93). Also, the authors confirmed that time-to-hospital discharge was shorter when patients received ≥80% of the prescribed protein (hazard ratio [HR]: 1.25; 95% CI: 1.04–1.49) on day 12.46 Thus, optimizing the supply of calories and proteins is achieved through the implementation of a protocol of nutritional adequacy. In critically ill burned patients Conrad et al.47 recently showed that the implementation of one nutritional algorithm by the nursing staff satisfied 100% of the calories prescribed in 85.4% of the days compared to 61.6% of the days in the retrospective control group on EN; however, no differences were seen in the mortality rate, ICU stay, and duration of mechanical ventilation between the two groups.
CarbohydratesThe dose of carbohydrates (CH) should be 4–5g/kg/day and they should not exceed 1400–1500kcal/day as CH34 (Table 2). Diets rich in CH and proteins promote the lean body mass re-composition by increasing the synthesis of proteins and releasing endogenous insulin.48 However, in burned patients with at least 10% of their TBSAB, the reduced risk of nosocomial pneumonia could be the only clinical benefit following the use of enteral formulae rich in proteins and CH, and poor in lipids.48
Actual recommendations of macro and micronutrients in the critically ill burned patient.
| Nutrient | Daily dose suggested | Comment |
|---|---|---|
| Proteins | 1.5 at 2.0g/k/d | Daily supply <20–25% of the total caloric supply. Dose >2.2g/kg/d do not improve the optimal balance of proteins32,34 |
| Lipids | 1.0–1.5g/kg/d | <30% of non-protein calories. Optimize n3/n6 ratio. |
| Carbohydrates | 5–7g/kg/d | Do not exceed 1400–1500kcal/d as carbohydrates. Supply should not exceed 5.0mg/kg/min32,34 and the levels of glycemia 140–180mg/dl should be maintained with IV insulin (in the absence of DM) |
| Glutamine | 0.3–0.5g/kg/d | Should not be administered in the presence of hepatic and renal failure. The definitive recommendation is pending the results from the RE-ENERGIZE study54 |
| Coppera | 4.0–5.0mg | |
| Seleniuma | 300–500μg | Administered as IV sodium selenite or selenious acid |
| Zinca | 25–40mg | |
| Chrome | 15mg/d | |
| Vitamin Ca | 1.0–3–0g/d | First 24h: 66mg/kg/h58 until 110g during the first 24h |
| Vitamin Da | ≤70 years: 600IU>70 years: 800IU | Vitamin D3 (oral, enteral or parenteral). Vitamin D deficiencies are common (50%) although there is still no definitive recommendation on its supplementation75 |
| Vitamin Aa | 10,000IU | |
| Vitamin Ea | 20–25IU |
DM, diabetes mellitus; IV, intravenous; IU, international units.
In burned patients, the doses should be between 1.5 and 3.0-fold higher than the standard recommended dose and maintained based on the total body surface area burned (see text).
Fat percentage should be around 15–18%, never exceeding 20–30% of the total caloric non-protein supply (1.0–1.5g/kg/day).34 The greatest source of lipids is omega-6 fatty acids (proinflammatory effect). In burned patients, enteral formulae rich in omega-3 fatty acids such as eicosapentaenoic acid, γ-linolenic acid, and antioxidant micronutrients have not been studied yet. On the other hand, supplementations with omega-3 as the only immunonutrient strategy have had beneficial effects modulating the inflammatory response, promoting better tolerance to glucose and a lower risk of infections; indeed, in 92 patients with a TBSAB>15% and inhalation injury, Tihista et al.49 compared the effects of an enteral formula with 50% of the lipids as omega-3 vs one conventional formula low on fats (18% of energetic supply). The analysis of results showed that patients who receive omega-3-rich diets exhibit less episodes of sepsis and septic shock, and higher tolerance to EN.
ProteinsCritically ill burned patients have protein requirements 50% higher than those of healthy subjects under fasting conditions, which is why the protein requirement needs to be below 20–25% of the total caloric supply (from >1.5 to 2.0g/k/day)34 (Table 2). However, the optimal protein supply in these patients has not been established yet.
Specific nutrients: glutamineGlutamine, one essential amino acid for the management of critical condition, has been a growing controversy for the last few years. Back in 2001, Oudemans-van Straaten et al.,50 in a cohort of 80 surgical critically ill patients, showed that plasma levels of glutamine <0.42mmol/l were associated with higher mortality rates. Nevertheless, more recently, Heyland et al.51 could not confirm glutamine deficiency in the presence of two or more organic dysfunctions.
Back in the year 2013, the study Reducing Death due to Oxidative Stress, one international, multicenter RCT (n=1.223), administered glutamine and antioxidants following a 2×2 factorial design.51 Patients supplemented with glutamine received a dose of 0.35g/kg/day (Dipeptiven®, Fresenius Kabi, Germany) through parenteral route and another 30g/day through enteral route. The analysis of results showed that providing high doses of glutamine increased hospital mortality in the presence of organic dysfunction. More recently, Van Zanten et al.,52 administered a diet rich in glutamine, omega-3 fatty acids and antioxidants to 300 medical and surgical critically ill patients versus a protein-rich enteral diet. In the critically ill patients the glutamine-rich diet was associated with a higher mortality rate at 6 months (53.7% vs 34.5% in the control group, p=0.044).
So far, very few RCTs have been published studying the administration of glutamine dipeptides in critically ill burned patients. Back in 2013, Lin et al.,53 after providing 4 RCTs (n=155) showed that the administration of glutamine could be associated with a lower incidence of gram-negative bacteremia (OR: 0.27, 95% CI: 0.08–0.92, p=0.04) and hospital mortality (OR=0.13, 95% CI: 0.03–0.51, p=0.004). More recently, after including 6 RCTs, (n=225) Zanten et al.,54 showed a positive effect of enteral glutamine administration in the overall survival rate (risk ratio [RR]: 0.22, 95% CI: 0.07–0.62, p=0.005), and significantly shorter hospital stays (weighted mean difference, expressed in days: 6.06, 95% CI: 9.91–2.20, p=0.002), although no effect on nosocomial infections was confirmed.54
At present, Heyland et al.55 are conducting the study RandomizEd trial of ENtERal Glutamine to minimIZE thermal injury (RE-ENERGIZE, NCT00985205), a double-blind, multicenter, pragmatic RCT that will be including 2700 critically ill burned patients treated with enteral glutamine (0.5g/kg/d) or placebo. This RCT is being conducted in over 60 burned centers of Canada, U.S., Europe and Latin America and its primary goal will be to assess hospital survival; secondary goals are the incidence of nosocomial bacteremia due to gram-negative bacilli, ICU and hospital stays, and the quality of life after the burn. Results are expected by 2021.
Antioxidant micronutrientsTrace elements: antioxidant cocktailsThe pioneering works conducted by a Swiss group led by Berger30,31 in burned patients suggest that providing antioxidant cocktails reduces the incidence of infectious complications. Thus, back in 2006, after adding 2 RCTs (n=41), Berger et al.30 confirmed that providing Cu 2.5 at 3.1mg/d, Se 315 at 380μg/d, and Zn 26.2 at 31.4mg/d for 8–21 days reduced the incidence of nosocomial pneumonia. Then the same group showed that the parenteral supply of one antioxidant cocktail with Cu, Se and Zn for 14–21 days improved both the antioxidant status and the skin and plasma levels of Se and Zn associated with a lower incidence of pneumonia.31
Back in 2015, Kurmis et al.56 showed that the parenteral administration of Cu and Se, and the enteral and parenteral administration of Zn combined shortened hospital stays. However, the actual evidence on the effect that providing antioxidant micronutrients has on the antioxidant status of critically ill burned patient is still controversial. In this sense, recently, Raposio et al.,57 in a small RCT (n=20), showed that the enteral administration of squalene 100mg, vitamin C 30mg, coenzyme Q10 10mg, Zn 5mg, β-carotene 3.6mg, bioflavonoid 30mg and Se 55μg for two (2) weeks did not improve the plasma antioxidant capabilities. The duration of antioxidant therapy depends on the TBSAB; indeed 20–40% of the TBSAB requires a 7–8-day course of therapy. Two (2) weeks are not advisable with 40–60% of the TBSAB, and over 60% of the TBSAB requires a 30-day course of treatment.57
VitaminsVitamin C has a known endothelial protective effect by preventing occludin phosphorylation and tight junction damage, which in turn reduces capillary hyperpermeability and improves the microcirculation blood flow.58 Based on what we know today, we would need one daily dose of 3g/d (30 times the recommended daily dose) for 3–6 days in order to re-establish the levels of vitamin C in the period following the thermal aggression. In the year 2000, Tanaka et al.59 showed that high doses of vitamin C administered through parenteral route during the early phase of resuscitation (0.66mg/kg/h every 24h) minimized the need for fluid, tissue swelling, body weight gains, and days on mechanical ventilation. Back in 2012, in a retrospective review of 40 critically ill burned patients with over 20% of their TBSAB, Khan et al.60 showed that, in these patients, the administration of high doses of vitamin C reduced the need for fluids and increased the urinary output. Similarly, these authors showed that the use of huge doses of vitamin C was safe and would not elevate the risk of renal failure.60
The standard nutritional therapy seems to be insufficient if we want to correct the levels of 25 dihydroxyvitamin D in critically ill burned patients, which is why higher doses should be considered here as suggested by Mayes et al.61 However, few RCTs have been conducted so far assessing supplements with high doses of vitamin D through oral, enteral, and parenteral routes in critically ill burned patients. In 2016, 2 systematic and meta analytical reviews were conducted in order to assess vitamin D supplements in the ICU setting (Putzu et al.62 and Weng et al.63; in the present year Langlois et al.64 after adding 6 RCTs [n=695]) and they did not find any differences in the mortality rate, ICU or hospital stays, or days spent on mechanical ventilation. The subgroup analysis showed that the use of doses >300,000IU/d could have something to do with a tendency toward reduced mortality rates (p=0.12) and shorter ICU stays (p=0.12).64
In burned adult patients the administration of vitamin D3 and calcium happened outside the critical phase of the disease. In this sense, Rousseau et al.65 found that, in these patients, hypovitaminosis D and osteopenia were common, and the administration of high doses of vitamin D after ICU discharge was associated with improved muscle strength of the quadriceps. This year, Ebid et al.66 showed that, in 48 burned children, the co-administration of vitamin D3 plus a training plan improved muscle strength, lean body mass, and the serum levels of vitamin D.
Probiotics and synbioticsThe critical condition is characterized by overgrown pathogenic bacteria with concomitant reduction of the so-called “health-promoting bacteria” (Lactobacillus and Bifidobacterium) of the microbiome—a phenomenon known as dysbiosis.67 In an attempt to re-establish the bioecological intestinal balance, the supply of probiotics and synbiotics has been a strategy approved in several populations of critically-ill patients. Recently, Manzanares et al.,68 after adding 30 RCTs in adult critically ill non-burned patients showed that the use of probiotics reduced the incidence of ICU-acquired infections (RR: 0.80; 95% CI: 0.68–0.95, p=0.009) and mechanical ventilation-related pneumonia (RR: 0.74; 95% CI: 0.61–0.90, p=0.002). However, in burned patients the use of probiotics has not been very well studied; thus, in 2015, Mayes et al.69 administered Lactobacillus gorbach goldin vs placebo at a daily dose of 2×105UFC/ml within the 10 days following the ICU admission to 20 critically burned kids. The study results did not show any clinical benefits in terms of less infections, use of antibiotics, or digestive tolerance.69
For all these reasons, the actual evidence on probiotics does not come from studies conducted in critically ill burned patients. Similarly, the actual recommendations do not say when to start the therapy or what type of probiotic should be used, with the only exception of Saccharomyces boulardii.67 In this sense, 40% of invasive infections (fungemia and infective endocarditis) due to Saccharomyces have been reported in patients where Saccharomyces boulardii has been administered as a probiotic,70 and cases of fungemia have been reported in burned patients as a complication derived from its use.71 Therefore, Saccharomyces boulardii is not considered a probiotic in critically ill patients and, therefore, should not be administered in severely burned patients.
Taking this into consideration, ecoimmunonutrition with probiotics and synbiotics in burned patients still cannot be recommended, and newly well-designed clinical trials in this population of critically ill patients are still needed.
Pharmacomodulation strategies of hypermetabolism and hypercatabolismDuring the last few decades several pharmacological strategies (non-nutritional) have been implemented in order to reduce catabolism and/or improve anabolism in the critically ill burned patient.32,34 The drugs studied on this regard have been different anabolic hormones such as growth hormone, insulin, oxandrolone, testosterone, the insulin-like growth factor-1 and associations, the insulin-like growth factor-binding protein 3, and certain drugs such as metformin and propranolol. Among the aforementioned strategies, the beta-adrenergic blocking has been the most studied therapeutic strategy of all and the only one on which there is consensus by the American Burn Association (2013)72 as the most adequate one in the metabolic response control to stress in these patients. This is so because during the burn, there is a significant increase in the tenor of catecholamines with levels up to 10 times higher compared to baseline, which, in part, may explain the increased basal metabolic rate. Propranolol, a non-specific beta blocker agent, is capable of attenuating sympathetic hyperactivity by reducing thermogenesis and EE at rest.73 On the other hand, it reduces peripheral lipolysis and increases the effectiveness of the protein synthesis by promoting better protein kinetics in the skeletal muscle with an improved net protein balance that goes up almost 82%.73 Also, Williams et al.74 showed that, following the burn, propranolol at 4mg/kg/d reduces both the cardiac output and cardiac work without affecting the average blood pressure. In burned kids with over 40% of their TBSAB, Barrow et al.75 found that the administration of propranolol avoided the appearance of hepatomegaly that is due to a reduced hepatic uptake of free fatty acids. Back in 2014, in a very interesting systematic review of medical literature, Núnez-Villaveirán et al.76 identified 15 RCTs that assessed the effects of propranolol in burned patients – mostly pediatric and adolescent patients. The analysis of these clinical trials shows that the dose range used to reduce the initial heart rate value by 15–20% has changed between 4 and 6mg/kg/d administered through oral, enteral o parenteral route.
More recently, Flores et al.77 published the results of a new systematic review and meta-analysis including 10 studies (9 of which were RCTs) including 1062 patients. The most significant findings of this meta-analysis showed that the use of propranolol associates a significant reduction of basal EE (Hedges’ g=−0.64, 95% CI: −0.8 to −0.5; p<0.001), abdominal fat (g=−0.3, 95% IC CI −0.4 to −0.1; p<0.001), and the corresponding increase of peripheral lean mass (g=−0.45; 95% CI: −0.3 to −0.6; p<0.001). The authors saw that the therapy with propranolol that was started between 48h and 12 days after thermal damage, and maintained variably between 10 days and 12 months (average 21 days), turned out to be a safe strategy.77
The use of oxandrolone (0.1mg/kg every 12h during variable time frames from 6 to 12 months) has proven beneficial effects in terms of shorter hospital stays,78 body weight gains, strength, and muscle mass, injury healing, and bone metabolism;79 these effects have been particularly reported in burned patients during the acute and rehab phases.
At present, the study Assessment of the Treatment of Severely Burned With Anabolic Agents on Clinical Outcomes, Recovery and Rehabilitation (NCT00675714),80 developed by the University of Texas Medical Branch, is planning to include 1100 patients in order to assess the early use of propranolol, oxandrolone, recombinant growth hormone, and ketoconazol as a single or combined strategy.
ConclusionsPatients with major burns are a model of acute malnutrition with an intense hypermetabolism and hypercatabolism. The correct assessment of requirements and matching energy and protein supply based on the progression of the disease has achieved better prognoses in these patients. Based on what we know today, an early enteral nutrition is of choice; also, during the resuscitation phase, burned patients should receive high doses of vitamin C, and supplements of antioxidant cocktails through parenteral route that should be administered variably and always based on the TBSAB. Also, supplying enteral glutamine seems to be a safe strategy capable of optimizing the therapeutic management, although more solid evidence is still needed before backing it up. Finally, the use of modulating non-nutritional strategies of hypermetabolism and hypercatabolism, in particular, propranolol and oxandrolone, has proven clinical benefits in the population of severely burned patients.
Conflict of interestsThe authors of this manuscript have declared that they do not hold any conflicts of interest.
Please cite this article as: Moreira E, Burghi G, Manzanares W. Metabolismo y terapia nutricional en el paciente quemado crítico: una revisión actualizada. Med Intensiva. 2018;42:306–316.