The incidence of diaphragmatic rupture secondary to blunt trauma (TDR) is estimated to be approximately 5% in patients with polytrauma. In this group, the ratio of laceration of the left side to the right is 20:1. TDR is typically considered a marker of severe trauma because of the high rate of associated injuries. Due to the multiplicity of injuries associated with the right hemidiaphragm and the rarity of its occurrence, it is often undiagnosed during initial hospitalisation.1,2 Diagnosis involves imaging techniques including chest radiography, computed tomography (CT), magnetic resonance imaging, and ultrasonography.3 Moreover, open surgical exploration has been introduced to diagnose highly suspicious cases based on equivocal imaging findings.
Hemidiaphragmatic rupture causes alterations in diaphragmatic function, which can be assessed using advanced mechanical ventilation monitoring in intubated patients. The occluded inspiratory airway pressure (Pocc), also known as the expiratory occlusion pressure, is the drop in airway pressure during inspiration against an occluded airway. Pocc is a non-invasive manoeuvre that is not influenced by respiratory mechanics. It ensures all intrathoracic pressures are equivalent,4,5 which allows it to assess the respiratory drive and inspiratory effort.5–7 Furthermore, the integrity of the diaphragm is necessary to establish a pressure gradient that separates the thoracic and abdominal cavities.
Herein, we present a previously unrecognised finding pertaining to Pocc in a patient with right TDR, which was explained by a diaphragmatic defect. In this study, Pocc revealed a loss of integrity of the diaphragmatic barrier between the thoracic and abdominal cavities and a reduction in the overall diaphragmatic contraction force. We aimed to describe the pathophysiological mechanism and usefulness of Pocc in diagnosing TDR to prevent delayed surgical repair and further complications such as herniation of abdominal contents and respiratory complications.
The clinical observation was made in a 43-year-old female patient admitted to our intensive care unit (ICU) after falling from a height. Her Glasgow Coma Scale was E1V1M4, and her vital signs were temperature of 35.9 °C, pulse rate of 135/min, respiratory rate of 32/min, and blood pressure of 91/50 mmHg. Physical examination revealed contusions in the left thoracic and abdominal region. Radiographic examinations revealed multiple right rib and pelvic bone fractures. Furthermore, CT of the chest and abdomen revealed elevation of the right hemidiaphragm, with a portion of the liver transposed into the right hemidiaphragm, emphasising a diaphragmatic defect (Fig. 1A). Cranial CT revealed no brain lesions.
(A) A preoperative computed tomography (coronal slice) scan of the chest and upper abdomen confirmed a right hemidiaphragmatic hernia, showing a liver in the right chest. (B) Image during repair surgery. A wide diaphragmatic defect showed protrusion of the liver through it. (C) Postoperative chest radiograph after surgical repair. (D) The surgical suture appreciated the width of the diaphragmatic tear.
Upon admission to the ICU, she required endotracheal intubation for respiratory failure.
Subsequently, the patient underwent a right posterolateral thoracotomy, and herniation of the liver and complete anteroposterior rupture of the diaphragm were observed in the thoracic cavity (Fig. 1B). After liver reduction, the diaphragmatic defect was repaired. The postoperative course was uneventful, and the patient was discharged 37 days later.
Prior to the surgical repair, pressure support ventilation (PSV) was selected using Servo-u® (Getinge, Sweden) ventilator with the following signal monitoring: Flow, airway opening pressure (Paw), oesophageal pressure (Pes), gastric pressure (Pgas), and tracheal pressure (Ptra). All traces were sampled at 1126 Hz, processed on a dedicated personal data acquisition system, and recorded for 60 min to 2–3 airway occlusions lasting 2–3 s at baseline and were repeated every 120 s. A double-balloon nasogastric catheter (Nutrivent; Sidam, Italy) was used. The transdiaphragmatic pressure was computed as ‘Pgas – Pes’. Signal analyses for the current study were performed using personal software and Excel 2019 (Microsoft, USA). Respiratory mechanics, particularly elastance of the respiratory system (Ers) and total resistance (Rrs), were obtained during passive ventilation using multiple linear regression.
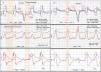
During the Pocc manoeuvre, the pressurisation baseline should recover after the relaxation of the inspiratory effort. However, in our case, a remarkable finding was observed noting a lack of recovery from the initial pressurisation, as shown by the drop in all intrathoracic pressures monitored in the absence of an air leak, indicated by the flow signal. This drop in pressurisation was proportional and parallel to the Paw and Pes (Fig. 2A). As previously described,8 the Pgas and Pdi signals showed reduced amplitude and biphasic morphology, revealing a reduced diaphragmatic contraction force due to hemidiaphragmatic dysfunction. After surgical repair of the diaphragm, the previous findings disappeared, with intrathoracic pressurisation recovering during the occlusion manoeuvre and normalisation of the amplitude and morphology of the Pgas and Pdi signals (Fig. 2B).
Traces of airway pressure (Paw), tracheal pressure (Ptra), oesophageal pressure (Pes), gastric pressure (Pgas), transdiaphragmatic pressure (Pdi), flow, and volume. Panel A, before surgery. During the expiratory occlusion manoeuvre, Paw and Ptra signals showed inability to maintain the PEEP set, as indicated by the descending step image, as the thorax and abdomen fused into a single compartment due to the diaphragmatic defect. Biphasic Pgas due to unilateral diaphragmatic injury and reduced Pdi. Note that Pes reflects the cyclic changes of Pgas—including expiratory muscle activation—and shares the same basal pressurization. Panel B, after the plication of the injured right diaphragm. The normalization of the signal during occlusion can be seen, as can the relationship between Pgas and Pes during inspiratory effort. Ers, Elastance respiratory system. Rrs, Total resistances respiratory system.
To our knowledge, this is the first description of the impact of a diaphragmatic defect on occlusion pressure shown by these findings: (1) an inability to recover baseline intrathoracic pressure after the patient's inspiratory effort; (2) a simultaneous, proportional, and parallel decrease in Paw with respect to Pes; and (3) confirmation of diaphragmatic repair by pressure normalisation.
Under static conditions during the Pocc manoeuvre, there is no airflow and no temporary gas acceleration; therefore, Paw = Palv (alveolar pressure). Considering that Palv = elastic recoil pressure (Pel) + pleural pressure (Ppl), a decrease in Ppl results in an equivalent reduction in Palv and is therefore reflected in PEEP and shown in Paw during Pocc.9
Loss of the diaphragmatic barrier can explain the decrease in Ppl because it unifies the thoracic and abdominal compartments. During inspiratory efforts against airway occlusion, Ppl is attenuated by the abdominal contents, which is reflected in the total decrease in Pes in the end-expiratory phase. One remarkable finding may help us understand this phenomenon: Pes reflects cyclic changes of Pgas, including expiratory muscle activation, and shares the same basal pressurisation (Fig. 2A).
Although we have used advanced monitoring of respiratory and abdominal signals, a simple occlusion manoeuvre during PSV, which is possible with most ventilators, can provide relevant findings in the Paw signal of diaphragmatic defects. This procedure highlights a high index of suspicion for diaphragmatic injury, therefore facilitating diagnosis and avoiding delays in surgical repair, particularly in the right hemidiaphragm, which is associated with multiple injuries. This study was conducted on a single patient, which is the main limitation, so further studies are needed. However, we have observed similar findings in other diaphragmatic dysfunctions (Electronic Supplementary Material).
CRediT authorship contribution statementJM SS designed and conducted the study, collected and analyzed the patient data, interpreted all data, and wrote the manuscript. NMP collected and interpreted the patient data and revised the manuscript. MVM interpreted the data and revised the manuscript. CBR interpreted the data and revised the manuscript. JFCMI revised the manuscript. ARC revised the manuscript. All authors commented on drafts of the manuscript and read and approved the final manuscript.
Ethics approval and consent to participateThe study procedures and data collected for this report were approved by the institution's local ethics committee of University Hospital, Reina Sofia, Cordoba, Spain, for inclusion in a research project (Refer.: Musc-Txp23). In addition, specific acceptance for this case report is provided (Ref.: SICEIA-2025-000989). The patient executed the permission to publish the patient information, was informed about the study with enough detail that the patient was admitted, understood the entire procedure, and signed a written informed consent form before inclusion in the study. All methods were performed according to the guidelines and regulations of the Declaration of Helsinki.
Declaration of Generative AI and AI-assisted technologies in the writing processNone.
FundingNone.
None.
The writers thank Dr. Jose Castaño Perez for their critical advice, encouragement, and corrections to this manuscript.