Resuscitators often face serious difficulties in making decisions when dealing with cardiac arrest (CA) victims. In general, cardiopulmonary resuscitation (CPR) is started and subsequently suspended if the patient shows evidence of a poor prior condition. However, in the absence of such evidence, and after some time has elapsed, we face the dilemma of whether to continue the maneuvers in an attempt to achieve patient recovery, or whether continuation is futile and should be suspended.
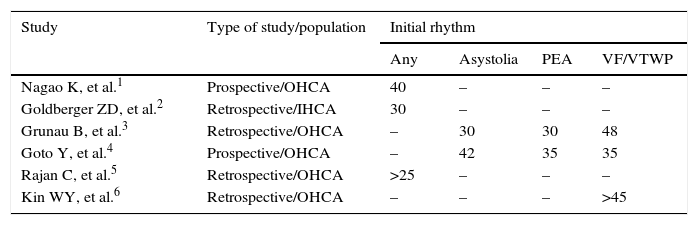
The interest of this subject has been evidenced by a number of studies that have attempted to establish the most appropriate duration of CPR1–6 (Table 1). We conduct an analysis of different aspects relating to prolonged CPR and to elements that seem to be necessary in this context.
Recommendations on the duration (min) of cardiopulmonary resuscitation in different studies.
| Study | Type of study/population | Initial rhythm | |||
|---|---|---|---|---|---|
| Any | Asystolia | PEA | VF/VTWP | ||
| Nagao K, et al.1 | Prospective/OHCA | 40 | – | – | – |
| Goldberger ZD, et al.2 | Retrospective/IHCA | 30 | – | – | – |
| Grunau B, et al.3 | Retrospective/OHCA | – | 30 | 30 | 48 |
| Goto Y, et al.4 | Prospective/OHCA | – | 42 | 35 | 35 |
| Rajan C, et al.5 | Retrospective/OHCA | >25 | – | – | – |
| Kin WY, et al.6 | Retrospective/OHCA | – | – | – | >45 |
PEA: pulseless electrical activity; VF: ventricular fibrillation; OHCA: out-hospital cardiac arrest; IHCA: in-hospital cardiac arrest; CPR: cardiopulmonary resuscitation; VTWP: ventricular tachycardia without pulse.
The 2015 ethical recommendations of the European Resuscitation Council (ERC) specify a maximum of 20min of CPR in the case of non-defibrillable rhythms in which the recovery of spontaneous circulation (ROSC) has not been achieved in any moment—though they also underscore the need to identify cases of refractory CA that might benefit from more prolonged interventions. The advances in resuscitation may change the established limits of the duration of CPR, modifying “established concepts”.
On the other hand, we must consider elements involved in CPR such as the feedback devices used to control resuscitation quality, mechanical chest compression, extracorporeal life support (ECLS) techniques,7 echocardiography to discard reversible processes, and “pseudo-CA” situations in patients presenting pulseless electrical activity (PEA),8 as well as transfer to hospital of some patients with ongoing CPR.
The monitoring of physiological parameters during CPR appears to be relevant to decision making. Endotracheal CO2 values of <10mmHg after 20min of maneuvering advise CPR cessation, while cases of survival have been reported with prolonged CPR maintaining values beyond those mentioned.9 The effectiveness of CPR and the possibilities for satisfactory patient recovery have also been associated to sustained brain oximetry readings of over 60%.10
The need to prolong CPR should be estimated based on the capacity of the abovementioned procedures to identify patients with a greater chance for survival, in which continuation of the resuscitation efforts would be indicated.
Although it has been reported that 90% of the cases recovered under good neurological conditions reach ROSC within a maximum of 16min,11 the optimum duration of CPR for incrementing survival has not been established. A very recent prospective study1 of 1617 patients with out-hospital CA (OHCA), evaluating the relationship between survival and the Cerebral Performance Category at discharge, versus the time from CPR onset to ROSC, has concluded that effort should be continued for 45min, whether CPR has been performed by witnesses or not, and regardless of whether the rhythm is defibrillable or not.
A study of 64,339 patients pertaining to the American in-hospital CA (IHCA) registry2 found longer CPR to be associated to higher percentages of ROSC and greater survival at discharge, suggesting that longer CPR could improve survival, and recommending at least 30min of maneuvering under any type of rhythm.
On the other hand, a retrospective study of OHCA cases has demonstrated an independent correlation between shorter CPR to ROSC and patient survival – the latter being less than 1% when CPR is prolonged up to 48min in defibrillable rhythms and 15min in non-defibrillable rhythms. The authors suggest that beneficial effects could be obtained by transferring patients with ongoing CPR to hospital for the application of more advanced techniques, and finally recommend maintaining CPR for 48minutes in young patients, with a defibrillable rhythm and witnessed CA, versus at least 30minutes in non-defibrillable rhythms.3
A retrospective study of 17,238 patients with OHCA recorded the time from CA onset to ROSC, and documented a survival rate with good neurological status of 21.8%. Over 99% of the patients with a good outcome had undergone CPR during 35min. In relation to the initial rhythm, ROSC was achieved after 35min in defibrillable rhythms and PEA, and after 42min in asystolia. The authors concluded that CPR should be prolonged for at least these time periods, depending on the type of rhythm.4
More recently, a retrospective study of 1316 cases of OHCA evaluating outcomes according to the CPR times to ROSC has demonstrated a correlation between greater percentage ROSC and shorter CPR times – though a CPR duration of over 25min was also seen to be associated to a percentage ROSC of over 20% and to acceptable percentage survival figures. The authors concluded that prolonged CPR should not be regarded as futile.5
Lastly, a retrospective study6 of 858 patients recovered after OHCA analyzed the influence of the time from CA to ROSC upon patient survival with good neurological status. Favorable outcomes were recorded in 22.2% of the cases with CPR times of over 20min (7.1% with CPR times of >60min).
In conclusion:
- 1.
Although the duration of CPR is an independent predictor of poorer survival and neurological status, recent publications suggest that maneuvering should continue for over 20min, reaching even 40min, with application of the new procedures referred to CPR quality and the use of diagnostic tools based on physiological parameters that can contribute to detect reversible cases and offer help in decision making.12
- 2.
In the case of IHCA, where we can know the patient history, most cases of ROSC occur in the first 30min. The recommendation could be to continue CPR in cases of defibrillable rhythms, for as long as these rhythms are maintained, while in the case of asystolia CPR should not be continued beyond 30min if no response has been elicited, after discarding reversible causes. If the hospital has the required resources, and with due case selection, ECLS measures or coronary intervention techniques could be decided with ongoing CPR.
- 3.
In the case of OHCA it is more difficult to establish the optimum duration of CPR, for in general we have less information about the patient. The recommendation would be to not continue CPR for more than 30min in the case of asystolia and the absence of reversible causes. Patient transfer to hospital with ongoing CPR should be evaluated in cases of CA witnessed by the emergency care team, ROSC in some moment, an initial defibrillable rhythm and possible reversible causes, where ECLS measures and coronary intervention even with ongoing CPR might be indicated. In this context, a strategy of patient transfer to a useful center (OHCA code)13 should be contemplated, depending on the characteristics and condition of the patient, and the hospital resources.
- 4.
Continuous monitoring of the quality of CPR is a necessary element for resuscitation teams at both in- and out-hospital level.
- 5.
The availability of mechanical chest compression is essential for maintaining the quality of CPR when resuscitation needs to be prolonged. It is necessary for the transfer of patients subjected to ongoing CPR with either recovery intent or for inclusion in non-heart beating donation programs.
- 6.
Continuous monitoring of endotracheal CO2 should be used by all resuscitation teams. Such monitoring is available in the great majority of emergency care settings, though not so at hospital level, where a recent survey found that 70% of the teams lacked this option.
- 7.
The availability of ultrasound for use during CPR is essential, since it helps in deciding the prolongation of CPR, discarding reversible causes or assessing situations with greater chances of recovery.
The author declares that he has no conflicts of interest.
Please cite this article as: López-Messa JB. ¿Cuál debe ser la duración apropiada de los intentos de resucitación cardiopulmonar? Med Intensiva. 2017;41:188–190.