Adequate ventilatory management of mechanically ventilated patients should be standard of care as it is essential to optimize therapy and minimize the risk of lung injury.1,2 Therefore, not only the fine-tuning of mechanical ventilation settings should be a goal, but also high-quality manual ventilations should be delivered. Manual bag ventilation is a routine intervention in most ICUs,3,4 and its quality is usually assumed to be adequate. However, as this is a provider-dependent non-controlled procedure (in terms of volume and/or pressure delivered) in actual practice, it is possible that current ventilation provided by nurses, when intermittent bagging mechanically ventilated patients, do not achieve the predefined goals.5,6
In our ICU, manual bag ventilation is usually performed before, during and after bronchial secretions aspiration as standard of care in every intubated and mechanically ventilated patient.7 This study aims to compare, in terms of delivered volumes and ventilation rate (VR), standard manual ventilation (SMV) to ventilation guided by a handheld ventilation feedback device (VFD). We hypothesized that blinded SMV deliver volumes and VR out of the standard goals. The use of a VFD would help ICU nurses deliver adequate ventilation, and thus potentially reduce related risks.
We conducted a prospective, randomized, and crossover study in a 10-bed ICU at a University Hospital in northwest Spain in July 2021. Eligible study participants were ICU nurses. Each participant randomly performed one blinded and one guided test during manual bag ventilation before, during, and after bronchial secretions aspiration within routine clinical practice (Supplementary Fig. 1). Each test lasted 1 min. Endotracheally intubated and deeply sedated adult patients without respiratory pathology were eligible for inclusion. Participation was voluntary, written informed consent was obtained from all participants and from patients or from their legal representatives if the clinical situation prevented it. The study was performed in accordance with the amended Declaration of Helsinki. The Research Ethics Committee of Santiago-Lugo approved the study (ref. no. CAEG 2021/233). During the guided test, ICU nurses were provided with real-time feedback on the quality of manual ventilation. Neither training nor written instructions about the VFD was provided to the participants. However, a short oral 1-minute explanation was made to every participant before the tests. To perform the ventilation sequences the VFD (EOlife®, Archeon medical, Besançon, France) was inserted between the bag (Ambu® Mark IV Adult, Ballerup, Denmark) and a heat and moisture exchanger filter (Clear-Therm™, Intersurgical Ltd, Wokingham, UK) before the endotracheal tube (Supplementary Fig. 2). Data on ventilation parameters were recorded with EOlife® software (Archeon medical, Besançon, France). For each test mean tidal volume (VT), minute ventilation (V̇e), and mean VR were recorded. We considered VT from 6 to 8 mL/kg of predicted body weight (PBW) and VR between 8 and 13 min−1 to be acceptable for these patients.1,2 Correct ventilation performance was defined by both VT and VR within the target range. Once both tests were completed, demographic characteristics of the participants were also recorded.
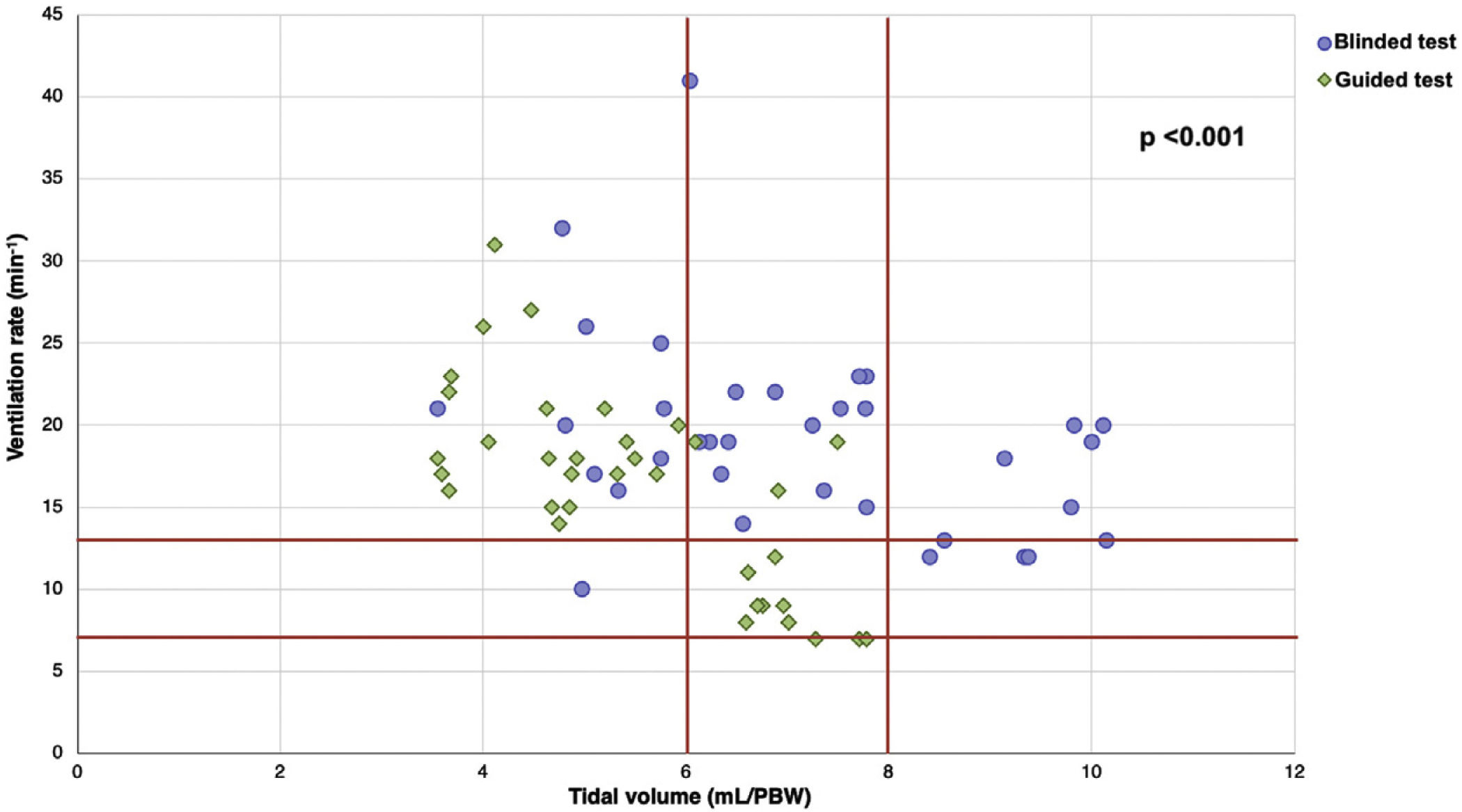
Thirty-five ICU nurses were enrolled into this study. Twenty-eight were women (80.0%). Mean participants’ age was 38.0 ± 9.6 years and their average working experience in ICU was 7.6 ± 7.7 years (Supplementary Table 1). We recorded 35 blinded SMV sequences and 35 manual ventilation sequences guided with a VFD. VT and V̇e were significantly lower during guided ventilation test. There were no significant differences in mean VR between groups (Table 1). By analyzing the performance of the 1-min ventilation sequences, we found a significant improvement of ventilation performance with the use of a VFD. Ventilation sequences with both VT and VR within the target range were only achieved during guided tests (Fig. 1).
Manual ventilation variables according to study group.
| Variable | Blinded test (n = 35) | Guided test (n = 35) | p-value |
|---|---|---|---|
| Ventilation rate, min−1 | 19.00 (15.00–21.00) | 17.00 (11.00–19.00) | 0.168 |
| Tidal volume, mL | 475.00 (397.00–590.00) | 367.00 (309.00–466.00) | 0.001 |
| Tidal volume, mL/kg PBW | 6.88 (5.754–8.551) | 5.32 (4.478–6.754) | 0.001 |
| Minute ventilation, L/min | 8.42 (7.446–10.899) | 5.70 (4.216–7.106) | <0.001 |
Abbreviations: PBW = predicted body weight.
Data are expressed as median (interquartile range). p-values calculated by by Wilcoxon signed-rank test. Statistically significant difference between groups: p < 0.05.
Our clinical impression that blinded SMV deliver volumes and VR clearly out of the goals motivated this study. Although this is a preliminary pilot study, to our knowledge, it is the first to evaluate the quality of usual care manual bag ventilation, in terms of delivered volumes and VR, performed by ICU nurses on real-life patient using a VFD. Our results are somewhat concerning. When delivered blinded SMV, experienced ICU nurses did not perform ventilations correctly, basically VR was out of the target range. In addition, although there was a significant improvement of ventilation performance with the use of a VFD, most participants did not achieve the predefined ventilation goals.
Every intervention to be done in critically ill patients should be trained and measure to minimize potential related risks and to ensure patient safety.8,9 In this sense, our findings suggest that ICU nurses should be trained and retrained in how to perform quality manual bag ventilations. We consider that the potential usefulness of modern portable VFD should be better explored as these could be helpful to train ICU staff in manual bag ventilations and to deliver adequate manual ventilatory support.
Our study has some limitations. First, this is a preliminary study, a proof of concept, which may limit its generalizability. However, our findings justify further studies on how to improve manual ventilation to reduce potential related risks. Second, airway pressure is another important parameter when bagging a patient. Unfortunately, the VFD used in this study does not measure the pressure generated in the respiratory system. Blinded and uncontrolled SMV could generate very high airway pressures, even higher when ventilating severely obstructed or restricted lungs. Third, some participants could alter their behavior in response to their awareness of being observed (Hawthorne effect). Finally, the measurements were recorded while manually ventilating a patient without respiratory pathology. It is possible that in case of patients with lung diseases (pneumonia, acute respiratory distress syndrome, asthma, etc.) the results would be different. Though it is easy to assume that in that situation, the quality of manual ventilations would be even worse.
In conclusion, ICU nurses seem not to be able to deliver adequate ventilations when perform usual care SMV in mechanically ventilated patients. A VFD helps to improve the performance of manual bag ventilation. Therefore, VFD should be considered at least in training of healthcare professionals to learn how to perform manual bag ventilation correctly.
Authors contributionERR, SMA, and MCI wrote and prepared the manuscript. AEG performed statistical analysis. ARN supervised and approved the final version of the manuscript.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval and consent to participateThe study was performed in accordance with the amended Declaration of Helsinki. The Research Ethics Committee of Santiago-Lugo approved the study (ref. no. CAEG 2021/233). Participation was voluntary, written informed consent was obtained from all participants and from patients or from their legal representatives if the clinical situation prevented it.
Conflict of interestThe authors have no conflict of interest to declare regarding this article.
The authors acknowledge all the ICU nurses who has participated in this study.