Community-acquired bacterial meningitis (CABM) remains an important health problem due to its morbidity and mortality, specially in critical care units (CCU) where the severity of the disease increases mortality from 15 up to 47%.1
Streptococcus pneumoniae is the most frequent aetiology for CABM in adults, reaching to 75–80% of all bacterial meningitis cases,2 but despite a high mortality, guidelines keep on recommending the same empirical antibiotic pattern since 2004.
Recently, ceftaroline, a fifth-generation cephalosporine with an approved indication for community-acquired bacterial pneumonia, has shown potential benefits for meningitis, opening the possibility for its use in CABM. The objective of our study was to evaluate the effectiveness of cetaroline in critically ill patients with CABM.
A retrospective, observational study including patients admitted to our CCU because of S. pneumoniae CABM from 2014–2019 was conducted. Participants received ceftaroline or standard therapy according to medical criteria. Primary outcome was 30-day mortality. Secondary outcomes were clinical response (if all signs and symptoms present at the time of diagnosis had improved or disappeared), need for invasive mechanical ventilation (IMV), length of stay and meningitis complications.
The quantitative variables were obtained as median (IQR), the qualitative as percentages. For the comparison, chi-square or Fisher's exact test was used for categorical variables and Student t-test or Mann–Whitney U for continuous variables. The hospital's ethic committee approved the project; informed consent was waived due to the retrospective nature of the study.
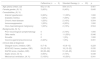
Twenty-five patients were included, five received ceftaroline, twenty were treated with other drugs. The demographical date are depicted in Table 1. Ceftaroline patients presented in a more severe condition by APACHE II (24 [22–33] vs. 18 [13–22], p=0.035) and SAPS III scores (82 [60–88] vs. 51 [43–65], p=0.024), septic shock rate at CABM diagnosis (60% vs. 10%, p=0.038) and need for IMV (100% vs. 50%, p=0.041). Biochemical and microbiological results from cerebrospinal fluid (CSF) and blood at diagnosis were similar in both groups, except for serum procalcitonin which was significantly higher in the ceftaroline group (21.16 [16.81–25.50] vs. 2.80 [1.84–7.25] ng/mL, p=0.039).
Patient's demographic and clinical characteristics.
| Ceftaroline (n=5) | Standard therapy (n=20) | p | |
|---|---|---|---|
| Age (years) (mean, sd) | 65.2 (11.8) | 59.4 (15.7) | 0.451 |
| Female gender, (N, %) | 3 (60%) | 9 (45%) | 0.645 |
| Comorbidities, (N, %) | |||
| Arterial hypertension | 3 (60%) | 11 (55%) | 1.000 |
| Diabetes mellitus | 1 (20%) | 7 (35%) | 1.000 |
| Chronic heart disease | 1 (20%) | 2 (10%) | 0.504 |
| Immunosuppression | 1 (20%) | 4 (20%) | 1.000 |
| Onco-haematological malignancy | 1 (20%) | 2 (10%) | 0.504 |
| Backgrounds, (N, %) | |||
| Prior neuorological symptomatology | 0 | 2 (10%) | 1.000 |
| Otitis media | 0 | 11 (55%) | 0.046 |
| Sinusitis | 0 | 1 (5%) | 1.000 |
| Vaccine against pneumococcus | 2 (40%) | 1 (5%) | 0.091 |
| Clinical data at diagnosis | |||
| Glasgow score, (median, IQR) | 8 (7–8) | 10 (8–12) | 0.229 |
| APACHE II score, (median, IQR) | 24 (22–33) | 18 (13–22) | 0.035 |
| SAPS3 score, (median, IQR) | 82 (60–88) | 51 (43–65) | 0.024 |
| Septic shock, (N, %) | 3 (60%) | 2 (10%) | 0.038 |
| Mechanical ventilation, (N, %) | 5 (100%) | 10 (50%) | 0.041 |
All patients received appropriate empirical treatment. In the standard group, 19 (95%) patients received ceftriaxone (2g/12h) for a median of 14 days [9–20.5], in combination with linezolid (600mg/12h) for a median of 5 days [3–13] in 13 patients (65%) or vancomycin (15mg/kg/day) for a median of 4 days [2–14] in 7 patients (35%). In 5 patients (25%) ampicillin (2g/6h) was added to the combination. One patient was treated with clindamycin, linezolid and levofloxacin due to beta-lactam allergy. All Streptococcus pneumoniae isolated in microbiological culture were susceptible to ceftriaxone (CMI≤0.25mg/L) or cefotaxime (CMI≤1mg/L). Nineteen patients (95%) were also treated with steroids for a median of 4 days [3–5.5].
All patients treated with ceftaroline had previously received standard empiric antibiotic treatment. Most of these patients were treated after less than 24h in the hospital because of S. pneumoniae aetiology confirmation. Only in one patient treatment was switched to ceftaroline due to a lack of response to standard treatment. In this patient, the ceftaroline CMI was 0.047mg/L. All patients were treated for a median of 11 [8–15] days, in combination with linezolid (600mg/12h) for a median of 6 [6–7] days and with steroids for 4 days, except for one patient who received steroids during all CCU stay.
Although not statistically significant, 30-day mortality was higher in the standard group (40% vs. 0%, p=0.116) in similar way to clinical response at the end of treatment (100% vs. 60%, p=0.086). CCU length of stay was longer for ceftaroline group (18 [14–28] vs. 4 [3–13] days, p=0.040). Other complications related to CABM are depicted in Table 2.
Clinical response and complications.
| Ceftaroline (n=5) | Standard therapy (n=20) | p | |
|---|---|---|---|
| Mechanical ventilation, (N, %) | 5 (100%) | 10 (50%) | 0.041 |
| Glasgow score (72h), median (IQR) | 7 (3–8) | 14 (13–15) | 0.015 |
| Clinical response (72h), (N, %) | 2 (40%) | 12 (60%) | 0.623 |
| Symptoms resolution end of treatment (N, %) | 5 (100%) | 12 (60%) | 0.140 |
| Cerebral abcess, (N, %) | 2 (40%) | 1 (5%) | 0.091 |
| Cerebritis, (N, %) | 1 (20%) | 3 (15%) | 1.000 |
| Epilepsy, (N, %) | 1 (20%) | 3 (15%) | 1.000 |
| Cerebral ischaemia, (N, %) | 3 (60%) | 4 (20%) | 0.113 |
| Cerebral edema, (N, %) | 0 (0%) | 2 (10%) | 1.000 |
| Cerebral death, (N, %) | 0 (0%) | 1 (5%) | 1.000 |
| Death, (N, %) | 0 (0%) | 8 (40%) | 0.140 |
Ceftaroline was approved for community-acquired pneumonia treatment, after the results of FOCUS I and II clinical trials.3,4 The potential efficacy in meningitis has been studied in animal models. Ceftaroline showed higher bacterial killing rate in rabbit models than the comparator (cefepime or ceftriaxone). For S. pneumoniae meningitis model the change in bacterial load was -0.71±0.06 log10 vs. −0.59±0.11 log10 every hour in favour of ceftaroline (p<0.009).5 Besides this, they observed a good ceftaroline CSF penetration achieving enough antibiotic concentration to be effective.
Despite these promising results, clinical experience in S. pneumoniae CABM is scarce. Sakoulas et al. reported four patients treated with ceftaroline; all cases responded successfully except one who received an insufficient dossage (600mg every 12h instead of 600mg every 8h).6 In a population-based epidemiologic study performed in the USA, 18 of 764 patients treated with ceftaroline corresponded to meningitis, with a mortality rate of 6% and a 22% rate of CCU admission.7
All our patients received 600mg/8h of ceftaroline except one who received 300mg/12h because of renal failure. Pharmacokinetic characteristics in the critically ill patients suggest to use higher or different dosage regimens in various antibiotics. Specifically in central nervous infections, a one-dose pharmacokinetic study of ceftaroline for patients with an external ventricular drainage showed a CSF ceftaroline exposure of 9% of systemic exposure. Therefore, as ceftaroline is a time-dependent antibiotic, maximum dose and extended infusions seems to be the most advisable management.8
Our study presents a complex S. pneumoniae CABM cohort. Mortality rate for CABM has been identified to be 14–17%, but for those admitted to the CCU, it can reach up to 47%.1 In this line, our 30-day mortality was 40%, but surprisingly, despite a higher severity score indexes and a higher rates of septic shock presentation and need for invasive mechanical ventilation, none of the patients treated with ceftaroline died.
There are some limitations in this scientific letter. It is a retrospective study with a short number of cases, mainly in the ceftaroline group. We have been able to present an entire cohort and, therefore, collect data from two treatment groups, however, ceftaroline initiation was a microbiological decision (S. pneumoniae identification) in most of the cases without a clinical justification. Finally, although the used doses of ceftriaxone were appropriate according to the recommendations of the IDSA9 and ESCMID10 guidelines, it is true that French guidelines for meningitis promote higher ceftriaxone doses (75–100mg/kg/day).11
Nevertheless, given the tenuous prognosis of S. pneumoniae CABM admitted to CCU, we believe that our results could pioneer the use of ceftaroline for these patients and set the basis for the design of a proper study to demonstrate the efficacy and safety of ceftaroline in S. pneumoniae CABM.
In summary, treatment with ceftaroline seems to be a promising therapeutic option for CABM caused by S. pneumoniae.
Authors’ contributionsAll authors contributed to the conception of the study, interpretation of findings or writing of the manuscript. Ramírez has participated in the conception and design of the study and in the critical review of intellectual content. Martín-Cerezuela has participated in the design of the study and the acquisition, statistical analysis and interpretation of the data and has made the draft of the article. Frasquet has participated in the acquisition of microbiologic data. Padrón, Palacios and Barrios performed the initial data extraction and have participated in the acquisition of data and analysis and interpretation of data. All authors read and approved the final manuscript.