Severe pneumonia with the Influenza A-H1N1 virus was first reported in Mexico in April 2009,1 causing acute hypoxemic respiratory failure (AHRF), acute respiratory distress syndrome (ARDS), with an associated mortality ranging from 25.1–41% at different sites.2 The World Health Organization estimates that influenza affect 5–10% of adults and up to 20–30% of children, especially in immunosuppressed, at extremes of life, and in persons with comorbidities3 and causes approximately 390,000 deaths annually.
The outbreak of respiratory infection by the novel SARS-CoV-2 started in December 2019, in Wuhan (Hubei Province), China.4 From this city, the outbreak has been spreading to most countries worldwide in a severe pandemic.5 Up to December 3, 2020, the COVID-19 pandemic has given rise to a total of 62 million cases and 1.4 million deaths around the world,5 mainly due to respiratory failure, although a long list of complications in various organs and systems have been described. The COVID-19 disease is associated with severe pneumonia, AHRF, and ARDS, requiring intensive care and ventilatory assistance in up to 5% of cases, and with a reported mortality ranging from 30–60% (average 41%) at different sites.6
We wondered how case-fatality compares between ARDS-COVID-19 and ARDS-Influenza (A-H1N1), adjusting for known prognostic risk factors and obtained clinical chart information from consecutive patients with Influenza H1N1 (October 2019 to February 2020, prior to the COVID-10 outbreak) and patients with COVID-19 (March 2020 to October 2020). All patients had a positive viral RT-PCR test and fulfilled the 2012 Berlin Definition of Acute Respiratory Distress Syndrome. Patients with Influenza received Oseltamivir at 150mg daily for at least 5 days, and those with COVID-19 received various treatments that frequently included corticosteroids. The study was approved by the institutional ethics committee and informed consent was not required. The identity of the patients was protected.
Clinical and laboratory data were obtained upon admission and during the patients’ stay in the unit. High-resolution computed tomography (HRCT) was performed in all patients prior to admission to the respiratory intensive care unit (ICU). We calculated a bedside indicator of wasted ventilation, the ventilatory ratio (VR) as [1-minute ventilation (mL/min)×PaCO2 (mmHg)]/[predicted body weight×100×37.5)7 and the sequential organ failure assessment (SOFA) score, including PaO2/FIO2, platelets, bilirubin, creatinine, mean arterial pressure, and use of vasopressors. Glasgow score was the same as all the patients were sedated.
The information obtained was stored in an electronic database and the main outcome was survival from the ICU. Time to death was evaluated by a Cox proportional risk model, comparing the group with COVID-19 and that of the patients with influenza in non-adjusted models, and adjusting for age, gender, obesity, comorbidities, and biomarkers, and mechanical ventilation parameters.
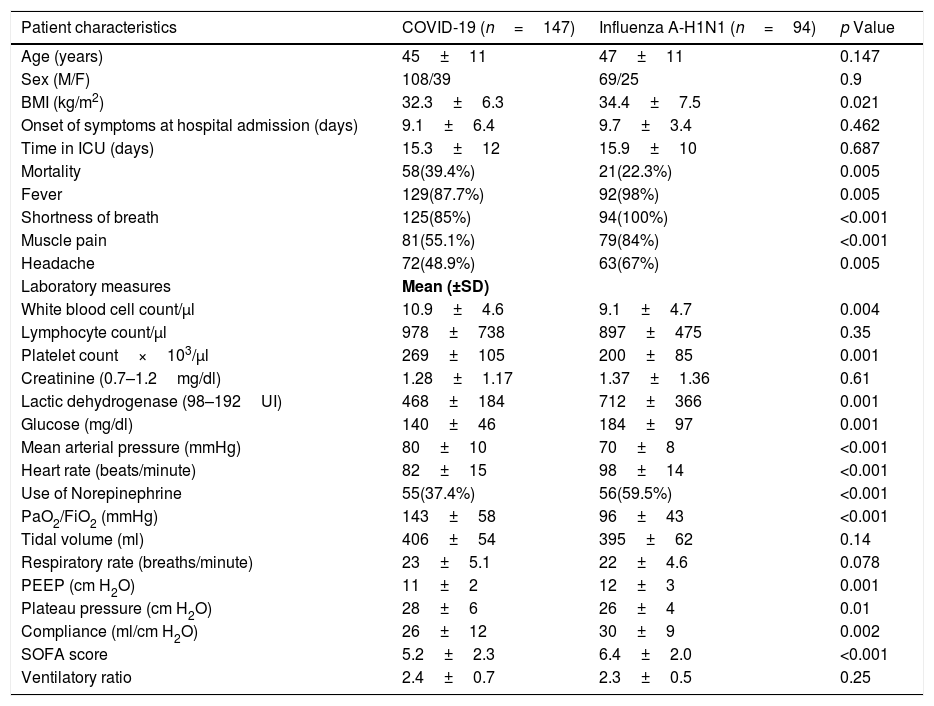
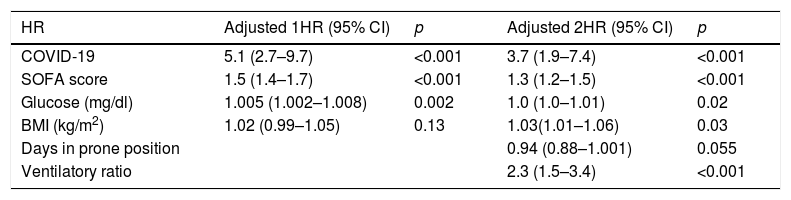
Statistical analysis was performed with SPSS (version 21) and with STATA (version13.0) statistical software packages. Two-sided p values of <0.05 were considered statistically significant. Table 1 presents the main characteristics of patients with influenza (n=94) and with COVID-19 (n=147). Patients with influenza had a slightly higher body mass index (BMI), lactic dehydrogenase glucose, and SOFA score, and a higher proportion of individuals with obesity, fever, shortness of breath, muscle pain, and headache, with lower neutrophils. Patients with influenza arrived for care in a worse situation (Table 1), they were more hypotense, hypoxemic, requiring vasopressors more frequently, with a higher SOFA score. Those with COVID-19 had a higher crude ICU mortality (39% vs. 22%; Fisher exact test; p=0.007; log-rank test, p=0.01), lower respiratory compliance, and spent more days in the prone position. Table 2 analyzes a multivariate Cox proportional risk model, having as a dependent variable time to death in the ICU and, as an independent variable, the type of virus (COVID-19 vs. influenza) adjusted by age, sex, comorbidities, symptoms, laboratory results, and ventilatory parameters: COVID-19 patients had nearly 4 times more risk for death (OR=3.7; 95% CI=1.9–7.4) than patients with influenza (see figure in supplement). Additional variables associated with predicting mortality were the ventilatory ratio, the SOFA score, and BMI, whereas the number of days in prone ventilation was associated with reduced mortality with borderline statistical significance (p=0.055).
Demographic and clinical biomarkers and radiologic characteristics of the patients.
| Patient characteristics | COVID-19 (n=147) | Influenza A-H1N1 (n=94) | p Value |
|---|---|---|---|
| Age (years) | 45±11 | 47±11 | 0.147 |
| Sex (M/F) | 108/39 | 69/25 | 0.9 |
| BMI (kg/m2) | 32.3±6.3 | 34.4±7.5 | 0.021 |
| Onset of symptoms at hospital admission (days) | 9.1±6.4 | 9.7±3.4 | 0.462 |
| Time in ICU (days) | 15.3±12 | 15.9±10 | 0.687 |
| Mortality | 58(39.4%) | 21(22.3%) | 0.005 |
| Fever | 129(87.7%) | 92(98%) | 0.005 |
| Shortness of breath | 125(85%) | 94(100%) | <0.001 |
| Muscle pain | 81(55.1%) | 79(84%) | <0.001 |
| Headache | 72(48.9%) | 63(67%) | 0.005 |
| Laboratory measures | Mean (±SD) | ||
| White blood cell count/μl | 10.9±4.6 | 9.1±4.7 | 0.004 |
| Lymphocyte count/μl | 978±738 | 897±475 | 0.35 |
| Platelet count×103/μl | 269±105 | 200±85 | 0.001 |
| Creatinine (0.7–1.2mg/dl) | 1.28±1.17 | 1.37±1.36 | 0.61 |
| Lactic dehydrogenase (98–192UI) | 468±184 | 712±366 | 0.001 |
| Glucose (mg/dl) | 140±46 | 184±97 | 0.001 |
| Mean arterial pressure (mmHg) | 80±10 | 70±8 | <0.001 |
| Heart rate (beats/minute) | 82±15 | 98±14 | <0.001 |
| Use of Norepinephrine | 55(37.4%) | 56(59.5%) | <0.001 |
| PaO2/FiO2 (mmHg) | 143±58 | 96±43 | <0.001 |
| Tidal volume (ml) | 406±54 | 395±62 | 0.14 |
| Respiratory rate (breaths/minute) | 23±5.1 | 22±4.6 | 0.078 |
| PEEP (cm H2O) | 11±2 | 12±3 | 0.001 |
| Plateau pressure (cm H2O) | 28±6 | 26±4 | 0.01 |
| Compliance (ml/cm H2O) | 26±12 | 30±9 | 0.002 |
| SOFA score | 5.2±2.3 | 6.4±2.0 | <0.001 |
| Ventilatory ratio | 2.4±0.7 | 2.3±0.5 | 0.25 |
Comorbidities were similar in both groups, except for chronic renal failure. All patients had lung opacities in a CT scanning of the thorax.
VR, ventilatory ratio. SOFA is the sequential organ failure assessment score (see text).
Adjusted multivariate Cox proportional hazard models.
| HR | Adjusted 1HR (95% CI) | p | Adjusted 2HR (95% CI) | p |
|---|---|---|---|---|
| COVID-19 | 5.1 (2.7–9.7) | <0.001 | 3.7 (1.9–7.4) | <0.001 |
| SOFA score | 1.5 (1.4–1.7) | <0.001 | 1.3 (1.2–1.5) | <0.001 |
| Glucose (mg/dl) | 1.005 (1.002–1.008) | 0.002 | 1.0 (1.0–1.01) | 0.02 |
| BMI (kg/m2) | 1.02 (0.99–1.05) | 0.13 | 1.03(1.01–1.06) | 0.03 |
| Days in prone position | 0.94 (0.88–1.001) | 0.055 | ||
| Ventilatory ratio | 2.3 (1.5–3.4) | <0.001 |
BMI, body mass index; VR, ventilatory ratio; HR, Hazard Ratio. SOFA is the sequential organ failure assessment score (see text). For the crude model (only COVID-19). Log likelihood -371, AIC 744, and BIC 748.
Patients with COVID-19 had a substantially higher lethality than those with influenza, despite both being in respiratory failure, both with ARDS, and after considering various predictors of death such as age, sex, some laboratory measurements, and ventilatory parameters, indicating in COVID-19 more severe lung damage and fewer possibilities of recovery. Influenza and COVID-19 may cause severe damage to the lungs, to other organs, and may cause death, and it is unknown whether this may be attributed to direct viral injury, to an exaggerated inflammatory reaction, or to the often mentioned cytokine storm8 in addition to personal susceptibility. Patients with COVID-19 have been compared with those with influenza and lacked a difference in cytokine levels.8 The findings of CT scanning overlap in the two infections,9 but patients with COVID-19 manifested vascular inflammation, and immunothrombosis10 to a higher degree than those with influenza. In addition, all of our patients received Oseltamivir, and an influenza vaccine of variable affectivity is available, although only a small proportion of our patients were vaccinated (5% of those arriving at the ICU). Most of our patients with COVID-19 received systemic corticosteroids, but an antiviral treatment and a vaccine were not yet available.
Our study shows limitations such as a small cohort of patients coming from a single high specialty center. However, it is prospective, and both cohorts were studied with few weeks of difference.
In conclusion, patients with respiratory failure and ARDS from COVID-19 treated in an ICU entertain a substantially increased risk of death compared with similar patients with Influenza A-H1N1, even adjusting for SOFA score and other relevant risk factors for mortality.
Author contributionsAuthors 1 and 4 concept; Authors 2 and 3 data collection; Authors 2 and 4 statistical analysis; Autors1, 2 and 4 elaboration of the manuscript.