To describe the case-mix of patients admitted to intensive care units (ICUs) in Spain during the period 2006–2011 and to assess changes in ICU mortality according to severity level.
DesignSecondary analysis of data obtained from the ENVN-HELICS registry. Observational prospective study.
SettingSpanish ICU.
PatientsPatients admitted for over 24h.
InterventionsNone.
VariablesData for each of the participating hospitals and ICUs were recorded, as well as data that allowed to knowing the case-mix and the individual outcome of each patient. The study period was divided into two intervals, from 2006 to 2008 (period 1) and from 2009 to 2011 (period 2). Multilevel and multivariate models were used for the analysis of mortality and were performed in each stratum of severity level.
ResultsThe study population included 142,859 patients admitted to 188 adult ICUs. There was an increase in the mean age of the patients and in the percentage of patients >79 years (11.2% vs. 12.7%, P<0.001). Also, the mean APACHE II score increased from 14.35±8.29 to 14.72±8.43 (P<0.001). The crude overall intra-UCI mortality remained unchanged (11.4%) but adjusted mortality rate in patients with APACHE II score between 11 and 25 decreased modestly in recent years (12.3% vs. 11.6%, odds ratio=0.931, 95% CI 0.883–0.982; P=0.008).
ConclusionThis study provides observational longitudinal data on case-mix of patients admitted to Spanish ICUs. A slight reduction in ICU mortality rate was observed among patients with intermediate severity level.
Describir el case-mix de los pacientes admitidos en las unidades de cuidados intensivos (UCI) españolas durante el periodo 2006-2011 y evaluar los cambios en la mortalidad en UCI según el nivel de gravedad.
DiseñoEstudio prospectivo y observacional. Análisis secundario procedente del registro ENVIN-HELICS.
ÁmbitoICU españolas.
PacientesPacientes ingresados más de 24h.
IntervenciónNinguna.
VariablesSe registraron los datos de cada UCI participante, así como aquellos que permiten conocer el case-mix y el estado al alta de cada paciente. El periodo de estudio se dividió en 2 intervalos, de 2006 a 2008 (periodo 1) y de 2009 a 2011 (periodo 2). Para el análisis de la mortalidad y en cada estrato de nivel de gravedad se realizó un estudio multivariante y multinivel.
ResultadosLa población estudiada incluye 142.859 pacientes ingresados en 188 UCI de adultos. Se apreció un incremento en la media de edad de los pacientes, así como en el porcentaje de los que eran mayores de 79 años (11,2 vs. 12,7%; p<0,001). La media de APACHE II se incrementó de 14,35±8,29 a 14,72±8,43 (p<0,001). La mortalidad bruta no varió (11,4%), pero la mortalidad ajustada en pacientes con APACHE II entre 11 y 25 disminuyó modestamente en los últimos años (12,3 vs. 11,6%, odds ratio=0,931, IC 95% 0,883-0,982; p=0,008).
ConclusionesEste estudio proporciona datos observacionales del case-mix de los pacientes ingresados en las UCI de España. Se observa una ligera reducción de la mortalidad en los pacientes con un grado intermedio en la escala de gravedad.
Knowledge of the general characteristics of patients (case-mix) admitted to Intensive Care Units (ICUs) and assessment of case-mix changes over time allow a more adequate provision of resources, the comparison of crude data among the different units and the design of hospital policies tailored to each ICU setting. This knowledge can be obtained from specific studies for certain diseases.1–4 These studies, however, do not give information about general characteristics of ICU patients not affected by these disorders.
Best case-mix descriptions of unselected critically ill patients are obtained from databases aimed to develop prognostic scales or from scales designed to measure workloads.5–9 Also, a number of multicentre studies with pooled data from the participating countries have been reported.10–15 Most of these studies referred to patients admitted to the ICU more than decade ago. Some more recent non-European studies16 or focused on specific aspects, such as sepsis17,18 have reported a decrease in mortality during the last years. The use of administrative databases19 does not allow the assessment of particular aspects that may influence upon the selection of resources ascribed to a particular unit. Data can also be obtained from prospective registries of different diseases in which all patients admitted to the ICU at risk to develop these diseases are included. Since 1994, an ongoing registry of ICU-acquired infections in critically ill patients has been developed in Spain. The ENVIN-HELICS registry20 (National Surveillance Study of Nosocomial Infection in the ICU – Hospital in Europe Link for Infection Control through Surveillance) includes data from all patients admitted to the participating ICUs for more than 24h. In our environment, updated studies of the global case-mix are lacking. This situation justifies the use of data collected from a specific registry.
Taking advantage of the ENVIN-HELICS registry, the following study was designed with two objectives: (a) to assess secular trends of case-mix of patients included in the registry between 2006 and 2011, and (b) to examine changes in ICU-related mortality in relation to variations in severity levels according to APACHE II scores during the study period.
Materials and methodsThe ENVIN-HELICS registry is an observational, prospective, multicentre and nationwide study, where data of all patients admitted to the participating ICUs for at least 24h are recorded. The aim of this registry is to collect the rates of nosocomial infections reported by participating ICUs all over the country. A multimodal intervention for the prevention of nosocomial infections was launched in 2009.21 The registry was started in 1994 and it is currently going on. For the present analysis, cases of patients admitted between 2006 and 2011 (inclusive) and whose data was complete were selected. A total of 188 ICUs for adults from 163 different hospitals provided data for this registry. All participating hospitals registered data during 3 months a year (from April 1st to June 30th). In addition, 32 of these ICUs registered data interruptedly over the whole year. A total of 105 ICUs have participated with the registration of data throughout the 6 years of the present analysis, 33 ICUs participated only during 5 years and a progressively lower number of ICUs in a decreasingly number of years. The present study was approved by the Clinical Research and Ethics Committee of Euskadi. Collected data were entered in the database, encrypted and anonymized. Because of the encryption process and the observational nature of the study, the patient's informed consent was not required.
The term “case-mix” was used to refer an interrelated set of patients’ characteristics. Patients were followed from the time of admission to the ICU till their discharge from the unit. The ICU and hospital in which patients were hospitalized were recorded as well as the admission source. Patients were classified according to the reason of admission into categories: elective surgery, urgent surgery and non-surgical medical illness; as well as according to the underlying disease: coronary, surgical, medical and trauma patients. Urgent surgery during the patient's stay in the ICU was also considered. The main diagnosis responsible for the ICU admission, including admission after solid organ transplantation (registered from 2009), was recorded. Other gathered data were comorbid conditions, presence of multi-resistant pathogens (colonization or infection), instrumentalization techniques and other procedures that patients underwent during their ICU stay, length of stay, clinical status on ICU discharge (measured by ICU-related crude mortality) and, in some cases (it is not compulsory to provide it while filling in the registry), date and clinical status at discharge from the hospital. Severity of illness was evaluated by means of APACHE II score.5 Changes in intra-ICU mortality were assessed according to the level of severity. Definitions of the terms used in the study have been previously reported.20,22
Patients were classified according to the reason of ICU admission into: (a) elective surgery when patients were admitted for the postoperative control of an elective surgical procedure; (b) urgent surgery when patients were admitted during the postoperative period of a surgical procedure that was performed within less than 24h of the surgical indication; and (c) medical when the reason of admission was none of the aforementioned. According to the underlying disease, patients were classified into coronary, surgical, trauma and medical.
Coronary patients included those admitted to the ICU because of an acute or chronic coronary syndrome, with or without ST-segment elevation in the electrocardiogram. Trauma patients were those whose reason of admission was an injury-related lesion, whether it was surgical or not. Surgical patients were those admitted in the immediate postoperative period after a surgical procedure (elective or urgent), and medical patients were those not included in the categories mentioned above, who suffered from diseases that did not require surgical treatment. Once the patient was admitted to ICU, urgent surgery was also considered. The main diagnosis that leaded to the ICU admission, including admission immediate after solid organ transplantation postoperative control (registered from 2009) was recorded.
The patients’ comorbid diseases, instrumentations and techniques performed during their ICU stay were registered, as well as days of stay in the ICU, status on ICU discharge (measured by the ICU crude mortality) and, in some cases (not compulsory for the ENVIN-HELICS registry), the time and clinical status at discharge from the hospital. The following comorbid conditions were evaluated: neutropenia, immunosuppression and immunodepression defined as follows, neutropenia as absolute neutrophil count <500cells/mm3, immunosuppression, patients who received treatments that reduced the resistance to infection (e.g. chemotherapy, radiation therapy, prolonged use of steroids, high doses of steroids or advanced diseases) and immunodepression when the patients were diagnosed with HIV infection or other acquired or congenital immunodeficiency disease.
The presence of colonization or previous infection by multi-resistant pathogens was evaluated, including methicillin-resistant Staphylococcus aureus, imipenem-resistant Acinetobacter baumannii, extended spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae or Gram-negative pathogens resistant to three or more antibiotic families and vacomycin-resistant Enterococcus. The starting and finishing dates of the following techniques were recorded: invasive mechanical ventilation, non-invasive mechanical ventilation, tracheostomy, central venous catheter, central arterial catheter, urinary catheter, renal replacement therapies, ventricular derivation techniques, parenteral nutrition, enteral nutrition, nasogastric tube insertion and reintubation (24h after extubation).
Severity of illness was assessed with the APACHE II scale and a corresponding value was calculated by subtracting the score corresponding to the patient's age. The presence of community-acquired or hospital-acquired (extra ICU) infections prior to ICU admission was evaluated together with nosocomial infections controlled in the ENVIN-HELICS registry. For this analysis, the presence or absence of infection was considered, independently of the infection focus and infection severity. The use of antimicrobials for the treatment of community-acquired, hospital-acquired and ICU-acquired infections was globally considered. The use of antibiotics following protocols of surgical prophylaxis or other type of prophylaxis (mechanical ventilation-associated pneumonia, pancreatitis, etc.) was also recorded.
Statistical analysisData were collected using the ENVIN-HELICS software application located in a web-based server available through Internet (http://hws.vhebron.net/envin-helics). The program is supplemented by safety systems that force to enter data of variables defined as basic and to prevent from entering illogical values, as well as by self-analyses systems, which allow obtaining real-time information for each ICU in particular and for a national data set. Periodic audits23 are established as a quality control of the reliability of data registered in the database.
Categorical variables are expressed as the percentages of distribution in each category. Quantitative variables are expressed as mean and 95% confidence interval (CI) or median and interquartile range (IQR) (25th–75th percentile) according to the normal or non-normal distribution of data. The APACHE II score was categorized into three levels according to the clinical criteria as low (score 0–10), intermediate (score 11–25) and high (score >25). Categorical data were compared with the Chi-square (χ2) and it is expressed as odds ratio (OR). Non-parametric continuous variables were compared with the Mann–Whitney U test or the Kruskal–Wallis test when appropriate. To assess the secular trends of categorical variables, two periods of time were selected, from 2006 to 2008 (period 1) and from 2009 to 2011 (period 2). This choice was made because of the implementation of interventions to reduce device-related infections began in 2009.21 Potential predictors of mortality with a P<0.20 in the univariate analysis were included in a multivariate analysis using hierarchical linear models, with mortality as the independent variable. For this analysis, random intercepts were considered. Patient was set at the level 1 unit and the ICU as the level 2 unit. This was performed for the overall sample and for each APACHE II severity group. Given that not all ICUs participated during the entire study period, the multilevel analysis allowed to control the influence on mortality of ICUs considered individually.
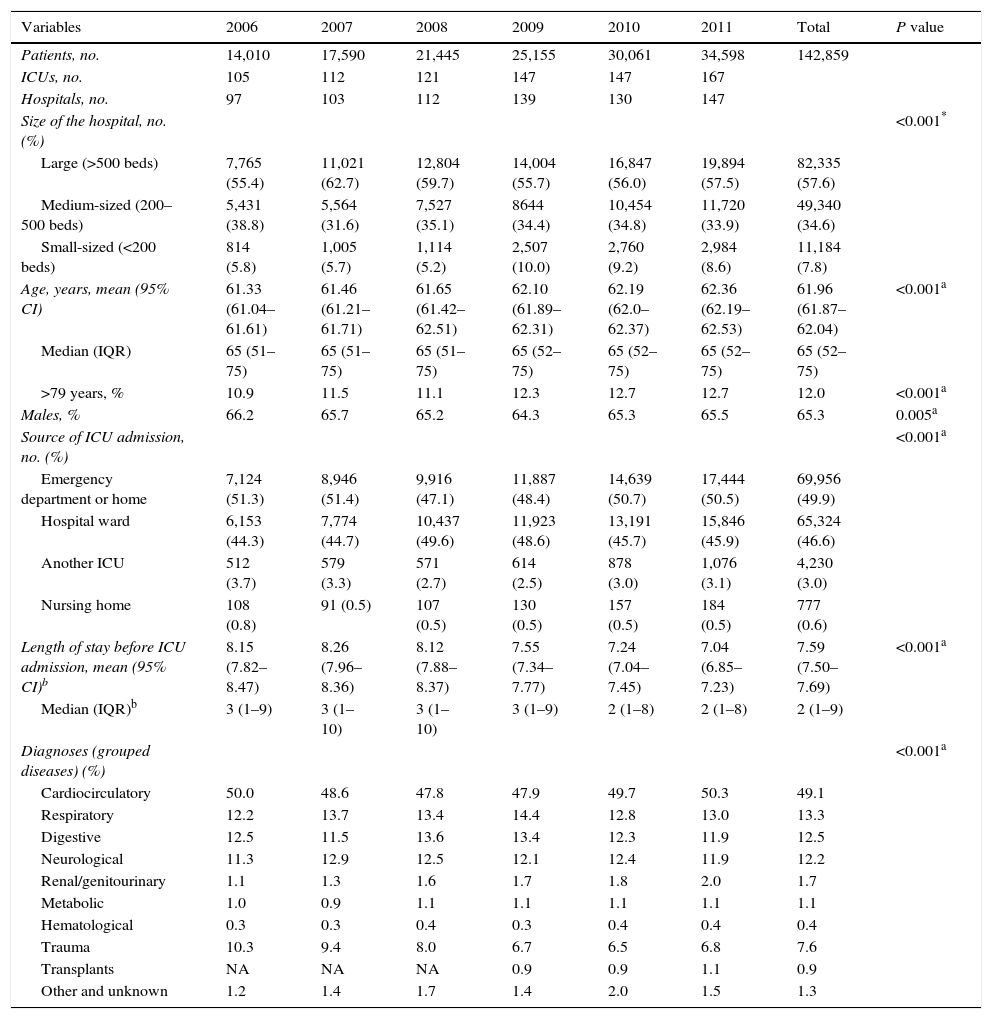
ResultsData of 142,859 were registered, with an increasing number of participating ICUs (Table 1), from 14,010 patients (9.8% of the total sample) in 2006 to 34,598 (24.2%) in 2011. The number of beds of the participating hospitals ranged between 90 and 1465. In relation to the size of the hospital, 57.6% of the patients were admitted to large hospitals (>500 beds), 34.6% to medium-sized (200–500 beds) and 7.8% to small-sized hospitals (<200 beds). The size of the participating ICUs varied between 4 and 48 beds, and most of the units (87.1%) were polyvalent medical-surgical ICUs.
General characteristics of patients and participating ICUs during the study period.
| Variables | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total | P value |
|---|---|---|---|---|---|---|---|---|
| Patients, no. | 14,010 | 17,590 | 21,445 | 25,155 | 30,061 | 34,598 | 142,859 | |
| ICUs, no. | 105 | 112 | 121 | 147 | 147 | 167 | ||
| Hospitals, no. | 97 | 103 | 112 | 139 | 130 | 147 | ||
| Size of the hospital, no. (%) | <0.001* | |||||||
| Large (>500 beds) | 7,765 (55.4) | 11,021 (62.7) | 12,804 (59.7) | 14,004 (55.7) | 16,847 (56.0) | 19,894 (57.5) | 82,335 (57.6) | |
| Medium-sized (200–500 beds) | 5,431 (38.8) | 5,564 (31.6) | 7,527 (35.1) | 8644 (34.4) | 10,454 (34.8) | 11,720 (33.9) | 49,340 (34.6) | |
| Small-sized (<200 beds) | 814 (5.8) | 1,005 (5.7) | 1,114 (5.2) | 2,507 (10.0) | 2,760 (9.2) | 2,984 (8.6) | 11,184 (7.8) | |
| Age, years, mean (95% CI) | 61.33 (61.04–61.61) | 61.46 (61.21–61.71) | 61.65 (61.42–62.51) | 62.10 (61.89–62.31) | 62.19 (62.0–62.37) | 62.36 (62.19–62.53) | 61.96 (61.87–62.04) | <0.001a |
| Median (IQR) | 65 (51–75) | 65 (51–75) | 65 (51–75) | 65 (52–75) | 65 (52–75) | 65 (52–75) | 65 (52–75) | |
| >79 years, % | 10.9 | 11.5 | 11.1 | 12.3 | 12.7 | 12.7 | 12.0 | <0.001a |
| Males, % | 66.2 | 65.7 | 65.2 | 64.3 | 65.3 | 65.5 | 65.3 | 0.005a |
| Source of ICU admission, no. (%) | <0.001a | |||||||
| Emergency department or home | 7,124 (51.3) | 8,946 (51.4) | 9,916 (47.1) | 11,887 (48.4) | 14,639 (50.7) | 17,444 (50.5) | 69,956 (49.9) | |
| Hospital ward | 6,153 (44.3) | 7,774 (44.7) | 10,437 (49.6) | 11,923 (48.6) | 13,191 (45.7) | 15,846 (45.9) | 65,324 (46.6) | |
| Another ICU | 512 (3.7) | 579 (3.3) | 571 (2.7) | 614 (2.5) | 878 (3.0) | 1,076 (3.1) | 4,230 (3.0) | |
| Nursing home | 108 (0.8) | 91 (0.5) | 107 (0.5) | 130 (0.5) | 157 (0.5) | 184 (0.5) | 777 (0.6) | |
| Length of stay before ICU admission, mean (95% CI)b | 8.15 (7.82–8.47) | 8.26 (7.96–8.36) | 8.12 (7.88–8.37) | 7.55 (7.34–7.77) | 7.24 (7.04–7.45) | 7.04 (6.85–7.23) | 7.59 (7.50–7.69) | <0.001a |
| Median (IQR)b | 3 (1–9) | 3 (1–10) | 3 (1–10) | 3 (1–9) | 2 (1–8) | 2 (1–8) | 2 (1–9) | |
| Diagnoses (grouped diseases) (%) | <0.001a | |||||||
| Cardiocirculatory | 50.0 | 48.6 | 47.8 | 47.9 | 49.7 | 50.3 | 49.1 | |
| Respiratory | 12.2 | 13.7 | 13.4 | 14.4 | 12.8 | 13.0 | 13.3 | |
| Digestive | 12.5 | 11.5 | 13.6 | 13.4 | 12.3 | 11.9 | 12.5 | |
| Neurological | 11.3 | 12.9 | 12.5 | 12.1 | 12.4 | 11.9 | 12.2 | |
| Renal/genitourinary | 1.1 | 1.3 | 1.6 | 1.7 | 1.8 | 2.0 | 1.7 | |
| Metabolic | 1.0 | 0.9 | 1.1 | 1.1 | 1.1 | 1.1 | 1.1 | |
| Hematological | 0.3 | 0.3 | 0.4 | 0.3 | 0.4 | 0.4 | 0.4 | |
| Trauma | 10.3 | 9.4 | 8.0 | 6.7 | 6.5 | 6.8 | 7.6 | |
| Transplants | NA | NA | NA | 0.9 | 0.9 | 1.1 | 0.9 | |
| Other and unknown | 1.2 | 1.4 | 1.7 | 1.4 | 2.0 | 1.5 | 1.3 |
NA: not available.
An increase in the mean age of patients was observed, with a progressive increase in the percentage of patients aged 80 years or more. The median (IQR) age was 65 (52–75) years. In about 50% of patients, the ICU admission source was the community. Among patients previously admitted to the hospital (n=63,484), the median (IQR) length of hospitalization before transfer to the ICU was 21–9 days, with a decreasing trend in 2010 and 2011 (Table 1). The most frequently used diagnoses were cardio-circulatory diseases (49.1%), which included coronary heart diseases, followed by respiratory (13.3%), digestive (12.5%) and neurological (12.2%) diseases.
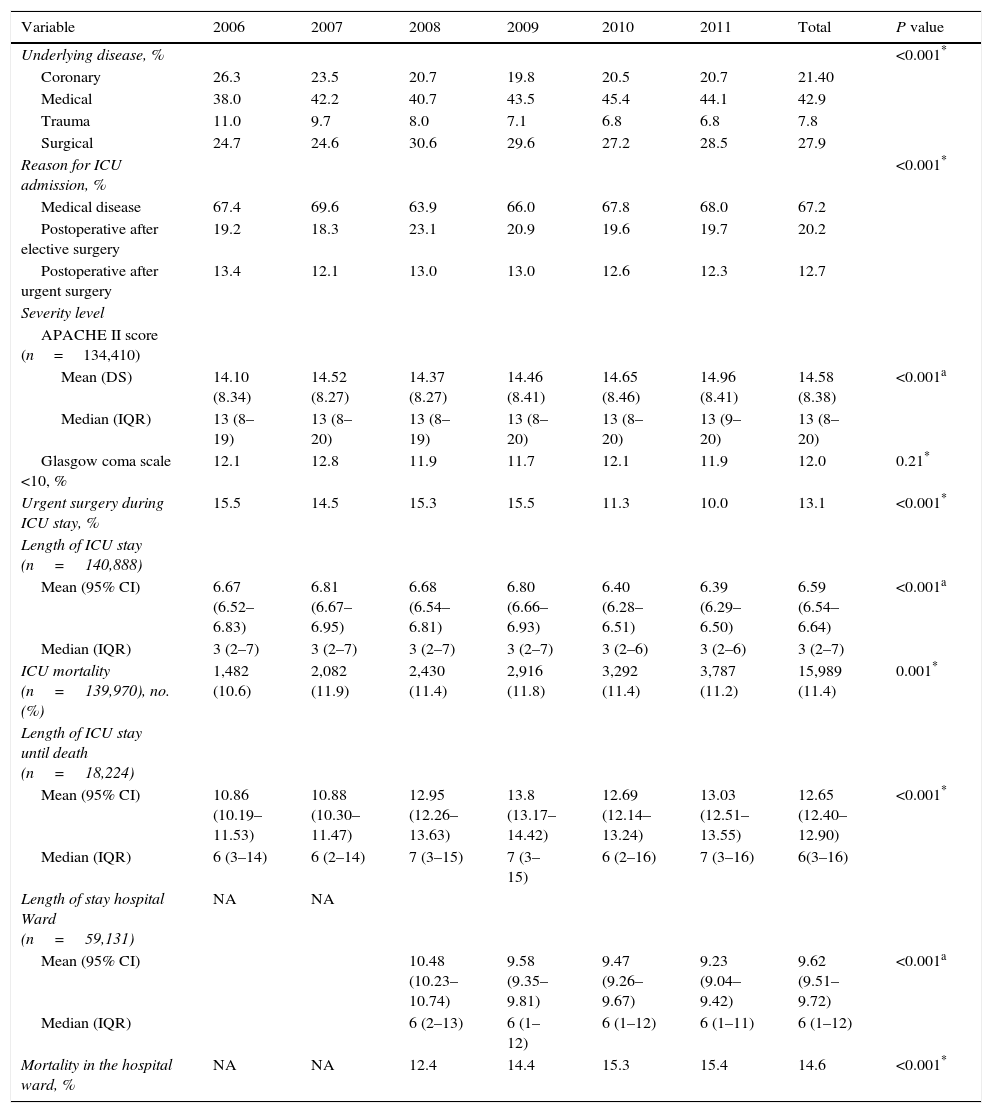
As shown in Table 2, medical diseases accounted for 42.9% of the underlying illnesses and predominated over coronary heart diseases, surgical diseases or traumatisms. There was a progressive decrease of trauma patients (11% in 2006 vs. 6.8% in 2011). The reason of ICU admission was surveillance after an elective surgical procedure in 20.2% of cases and urgent surgery in 12.7%, whereas most patients (67.2%) were admitted because of medical reasons. A total of 13.1% of patients required urgent surgery during their ICU stay. The median (IQR) length of ICU stay was 32–7 days. The ICU mortality rate was 11.4% after a median stay of 63–16 days. The hospital mortality rate was 14.6%, with a median (IQR) hospital stay after discharge from the ICU of 61–12 days.
Underlying diseases, reasons for ICU admission, severity of illness and mortality.
| Variable | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total | P value |
|---|---|---|---|---|---|---|---|---|
| Underlying disease, % | <0.001* | |||||||
| Coronary | 26.3 | 23.5 | 20.7 | 19.8 | 20.5 | 20.7 | 21.40 | |
| Medical | 38.0 | 42.2 | 40.7 | 43.5 | 45.4 | 44.1 | 42.9 | |
| Trauma | 11.0 | 9.7 | 8.0 | 7.1 | 6.8 | 6.8 | 7.8 | |
| Surgical | 24.7 | 24.6 | 30.6 | 29.6 | 27.2 | 28.5 | 27.9 | |
| Reason for ICU admission, % | <0.001* | |||||||
| Medical disease | 67.4 | 69.6 | 63.9 | 66.0 | 67.8 | 68.0 | 67.2 | |
| Postoperative after elective surgery | 19.2 | 18.3 | 23.1 | 20.9 | 19.6 | 19.7 | 20.2 | |
| Postoperative after urgent surgery | 13.4 | 12.1 | 13.0 | 13.0 | 12.6 | 12.3 | 12.7 | |
| Severity level | ||||||||
| APACHE II score (n=134,410) | ||||||||
| Mean (DS) | 14.10 (8.34) | 14.52 (8.27) | 14.37 (8.27) | 14.46 (8.41) | 14.65 (8.46) | 14.96 (8.41) | 14.58 (8.38) | <0.001a |
| Median (IQR) | 13 (8–19) | 13 (8–20) | 13 (8–19) | 13 (8–20) | 13 (8–20) | 13 (9–20) | 13 (8–20) | |
| Glasgow coma scale <10, % | 12.1 | 12.8 | 11.9 | 11.7 | 12.1 | 11.9 | 12.0 | 0.21* |
| Urgent surgery during ICU stay, % | 15.5 | 14.5 | 15.3 | 15.5 | 11.3 | 10.0 | 13.1 | <0.001* |
| Length of ICU stay (n=140,888) | ||||||||
| Mean (95% CI) | 6.67 (6.52–6.83) | 6.81 (6.67–6.95) | 6.68 (6.54–6.81) | 6.80 (6.66–6.93) | 6.40 (6.28–6.51) | 6.39 (6.29–6.50) | 6.59 (6.54–6.64) | <0.001a |
| Median (IQR) | 3 (2–7) | 3 (2–7) | 3 (2–7) | 3 (2–7) | 3 (2–6) | 3 (2–6) | 3 (2–7) | |
| ICU mortality (n=139,970), no. (%) | 1,482 (10.6) | 2,082 (11.9) | 2,430 (11.4) | 2,916 (11.8) | 3,292 (11.4) | 3,787 (11.2) | 15,989 (11.4) | 0.001* |
| Length of ICU stay until death (n=18,224) | ||||||||
| Mean (95% CI) | 10.86 (10.19–11.53) | 10.88 (10.30–11.47) | 12.95 (12.26–13.63) | 13.8 (13.17–14.42) | 12.69 (12.14–13.24) | 13.03 (12.51–13.55) | 12.65 (12.40–12.90) | <0.001* |
| Median (IQR) | 6 (3–14) | 6 (2–14) | 7 (3–15) | 7 (3–15) | 6 (2–16) | 7 (3–16) | 6(3–16) | |
| Length of stay hospital Ward (n=59,131) | NA | NA | ||||||
| Mean (95% CI) | 10.48 (10.23–10.74) | 9.58 (9.35–9.81) | 9.47 (9.26–9.67) | 9.23 (9.04–9.42) | 9.62 (9.51–9.72) | <0.001a | ||
| Median (IQR) | 6 (2–13) | 6 (1–12) | 6 (1–12) | 6 (1–11) | 6 (1–12) | |||
| Mortality in the hospital ward, % | NA | NA | 12.4 | 14.4 | 15.3 | 15.4 | 14.6 | <0.001* |
NA: not available.
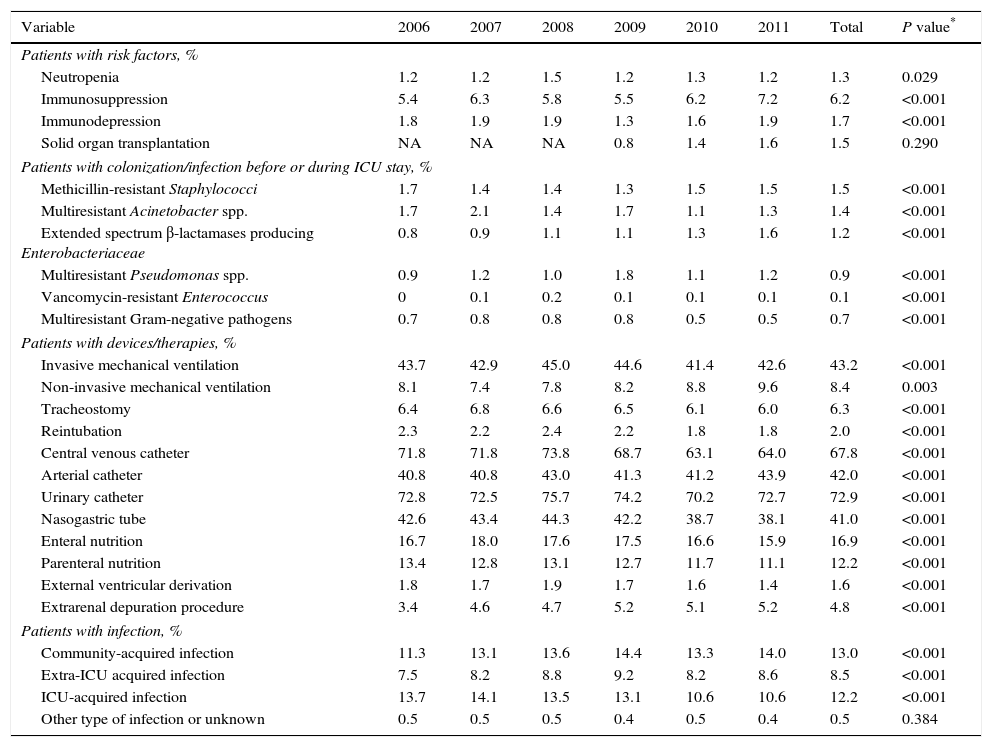
In relation to risk factors, type of infections and antibiotic treatment (Table 3), the comparison of most of the variables was statistically significant. There was an increasing trend in patients with immunosuppression or requiring renal replacement therapies. Also, the percentage of patients treated with non-invasive mechanical ventilation increased notably in the past 5 years in association with a decrease in the use of invasive mechanical ventilation. On the other hand, a decreasing trend in the use of other devices was also observed.
Risk factors, type of infections and antibiotic treatment.
| Variable | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total | P value* |
|---|---|---|---|---|---|---|---|---|
| Patients with risk factors, % | ||||||||
| Neutropenia | 1.2 | 1.2 | 1.5 | 1.2 | 1.3 | 1.2 | 1.3 | 0.029 |
| Immunosuppression | 5.4 | 6.3 | 5.8 | 5.5 | 6.2 | 7.2 | 6.2 | <0.001 |
| Immunodepression | 1.8 | 1.9 | 1.9 | 1.3 | 1.6 | 1.9 | 1.7 | <0.001 |
| Solid organ transplantation | NA | NA | NA | 0.8 | 1.4 | 1.6 | 1.5 | 0.290 |
| Patients with colonization/infection before or during ICU stay, % | ||||||||
| Methicillin-resistant Staphylococci | 1.7 | 1.4 | 1.4 | 1.3 | 1.5 | 1.5 | 1.5 | <0.001 |
| Multiresistant Acinetobacter spp. | 1.7 | 2.1 | 1.4 | 1.7 | 1.1 | 1.3 | 1.4 | <0.001 |
| Extended spectrum β-lactamases producing Enterobacteriaceae | 0.8 | 0.9 | 1.1 | 1.1 | 1.3 | 1.6 | 1.2 | <0.001 |
| Multiresistant Pseudomonas spp. | 0.9 | 1.2 | 1.0 | 1.8 | 1.1 | 1.2 | 0.9 | <0.001 |
| Vancomycin-resistant Enterococcus | 0 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | <0.001 |
| Multiresistant Gram-negative pathogens | 0.7 | 0.8 | 0.8 | 0.8 | 0.5 | 0.5 | 0.7 | <0.001 |
| Patients with devices/therapies, % | ||||||||
| Invasive mechanical ventilation | 43.7 | 42.9 | 45.0 | 44.6 | 41.4 | 42.6 | 43.2 | <0.001 |
| Non-invasive mechanical ventilation | 8.1 | 7.4 | 7.8 | 8.2 | 8.8 | 9.6 | 8.4 | 0.003 |
| Tracheostomy | 6.4 | 6.8 | 6.6 | 6.5 | 6.1 | 6.0 | 6.3 | <0.001 |
| Reintubation | 2.3 | 2.2 | 2.4 | 2.2 | 1.8 | 1.8 | 2.0 | <0.001 |
| Central venous catheter | 71.8 | 71.8 | 73.8 | 68.7 | 63.1 | 64.0 | 67.8 | <0.001 |
| Arterial catheter | 40.8 | 40.8 | 43.0 | 41.3 | 41.2 | 43.9 | 42.0 | <0.001 |
| Urinary catheter | 72.8 | 72.5 | 75.7 | 74.2 | 70.2 | 72.7 | 72.9 | <0.001 |
| Nasogastric tube | 42.6 | 43.4 | 44.3 | 42.2 | 38.7 | 38.1 | 41.0 | <0.001 |
| Enteral nutrition | 16.7 | 18.0 | 17.6 | 17.5 | 16.6 | 15.9 | 16.9 | <0.001 |
| Parenteral nutrition | 13.4 | 12.8 | 13.1 | 12.7 | 11.7 | 11.1 | 12.2 | <0.001 |
| External ventricular derivation | 1.8 | 1.7 | 1.9 | 1.7 | 1.6 | 1.4 | 1.6 | <0.001 |
| Extrarenal depuration procedure | 3.4 | 4.6 | 4.7 | 5.2 | 5.1 | 5.2 | 4.8 | <0.001 |
| Patients with infection, % | ||||||||
| Community-acquired infection | 11.3 | 13.1 | 13.6 | 14.4 | 13.3 | 14.0 | 13.0 | <0.001 |
| Extra-ICU acquired infection | 7.5 | 8.2 | 8.8 | 9.2 | 8.2 | 8.6 | 8.5 | <0.001 |
| ICU-acquired infection | 13.7 | 14.1 | 13.5 | 13.1 | 10.6 | 10.6 | 12.2 | <0.001 |
| Other type of infection or unknown | 0.5 | 0.5 | 0.5 | 0.4 | 0.5 | 0.4 | 0.5 | 0.384 |
NA: not available.
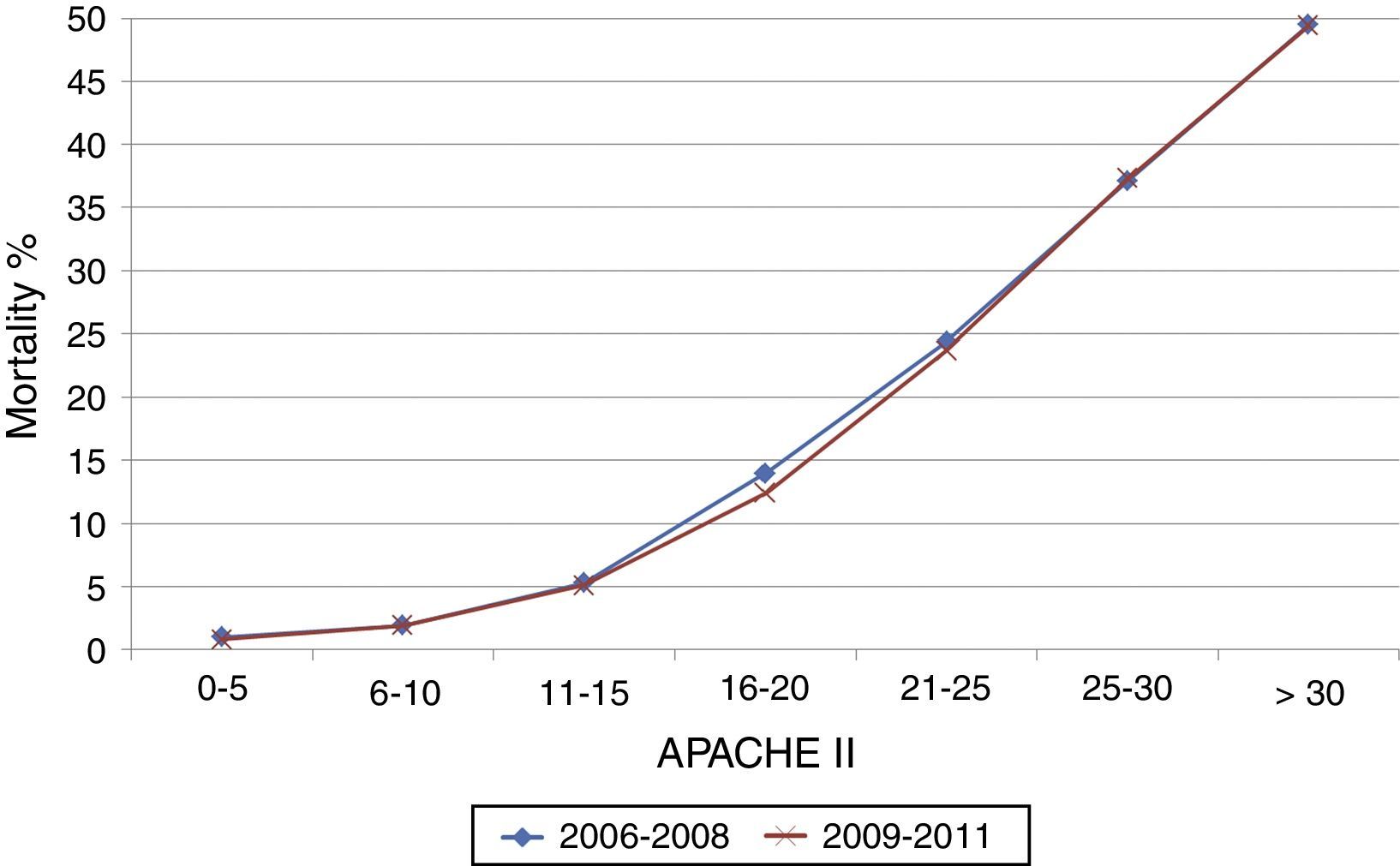
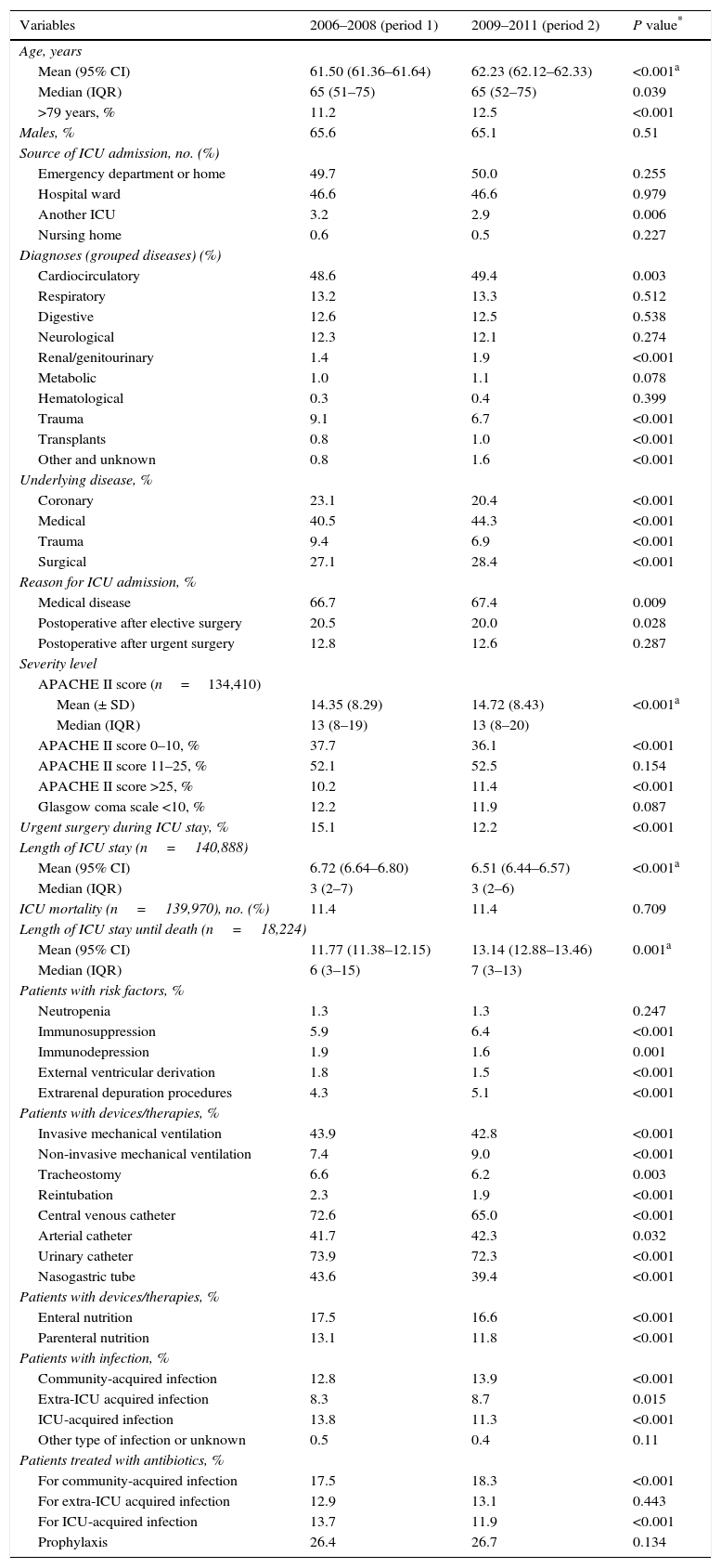
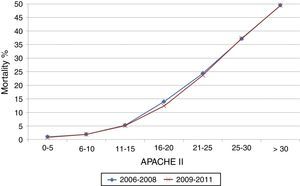
The comparison of the general characteristics of ICU patients between the two time periods (2006–2008 and 2009–2011) is shown in Table 4. Patients admitted in the last 3 years showed a higher percentage of older subjects (>79 years), higher APACHE II score on ICU admission due to an increase in the number of patients with APACHE II score >25. Also, there was an increase in patients with community-acquired infections and a decrease in ICU-acquired infections, as well as the corresponding variations in the use of antibiotics. The overall crude mortality rate was 11.4% in both periods. Fig. 1 shows the mortality rates stratified by severity level according to the APACHE II score. Table 5 shows the univariate analysis of the differences in mortality according to the study period.
Differences in the study variables between 2006–2008 (period 1) and 2009–2011 (period 2).
| Variables | 2006–2008 (period 1) | 2009–2011 (period 2) | P value* |
|---|---|---|---|
| Age, years | |||
| Mean (95% CI) | 61.50 (61.36–61.64) | 62.23 (62.12–62.33) | <0.001a |
| Median (IQR) | 65 (51–75) | 65 (52–75) | 0.039 |
| >79 years, % | 11.2 | 12.5 | <0.001 |
| Males, % | 65.6 | 65.1 | 0.51 |
| Source of ICU admission, no. (%) | |||
| Emergency department or home | 49.7 | 50.0 | 0.255 |
| Hospital ward | 46.6 | 46.6 | 0.979 |
| Another ICU | 3.2 | 2.9 | 0.006 |
| Nursing home | 0.6 | 0.5 | 0.227 |
| Diagnoses (grouped diseases) (%) | |||
| Cardiocirculatory | 48.6 | 49.4 | 0.003 |
| Respiratory | 13.2 | 13.3 | 0.512 |
| Digestive | 12.6 | 12.5 | 0.538 |
| Neurological | 12.3 | 12.1 | 0.274 |
| Renal/genitourinary | 1.4 | 1.9 | <0.001 |
| Metabolic | 1.0 | 1.1 | 0.078 |
| Hematological | 0.3 | 0.4 | 0.399 |
| Trauma | 9.1 | 6.7 | <0.001 |
| Transplants | 0.8 | 1.0 | <0.001 |
| Other and unknown | 0.8 | 1.6 | <0.001 |
| Underlying disease, % | |||
| Coronary | 23.1 | 20.4 | <0.001 |
| Medical | 40.5 | 44.3 | <0.001 |
| Trauma | 9.4 | 6.9 | <0.001 |
| Surgical | 27.1 | 28.4 | <0.001 |
| Reason for ICU admission, % | |||
| Medical disease | 66.7 | 67.4 | 0.009 |
| Postoperative after elective surgery | 20.5 | 20.0 | 0.028 |
| Postoperative after urgent surgery | 12.8 | 12.6 | 0.287 |
| Severity level | |||
| APACHE II score (n=134,410) | |||
| Mean (± SD) | 14.35 (8.29) | 14.72 (8.43) | <0.001a |
| Median (IQR) | 13 (8–19) | 13 (8–20) | |
| APACHE II score 0–10, % | 37.7 | 36.1 | <0.001 |
| APACHE II score 11–25, % | 52.1 | 52.5 | 0.154 |
| APACHE II score >25, % | 10.2 | 11.4 | <0.001 |
| Glasgow coma scale <10, % | 12.2 | 11.9 | 0.087 |
| Urgent surgery during ICU stay, % | 15.1 | 12.2 | <0.001 |
| Length of ICU stay (n=140,888) | |||
| Mean (95% CI) | 6.72 (6.64–6.80) | 6.51 (6.44–6.57) | <0.001a |
| Median (IQR) | 3 (2–7) | 3 (2–6) | |
| ICU mortality (n=139,970), no. (%) | 11.4 | 11.4 | 0.709 |
| Length of ICU stay until death (n=18,224) | |||
| Mean (95% CI) | 11.77 (11.38–12.15) | 13.14 (12.88–13.46) | 0.001a |
| Median (IQR) | 6 (3–15) | 7 (3–13) | |
| Patients with risk factors, % | |||
| Neutropenia | 1.3 | 1.3 | 0.247 |
| Immunosuppression | 5.9 | 6.4 | <0.001 |
| Immunodepression | 1.9 | 1.6 | 0.001 |
| External ventricular derivation | 1.8 | 1.5 | <0.001 |
| Extrarenal depuration procedures | 4.3 | 5.1 | <0.001 |
| Patients with devices/therapies, % | |||
| Invasive mechanical ventilation | 43.9 | 42.8 | <0.001 |
| Non-invasive mechanical ventilation | 7.4 | 9.0 | <0.001 |
| Tracheostomy | 6.6 | 6.2 | 0.003 |
| Reintubation | 2.3 | 1.9 | <0.001 |
| Central venous catheter | 72.6 | 65.0 | <0.001 |
| Arterial catheter | 41.7 | 42.3 | 0.032 |
| Urinary catheter | 73.9 | 72.3 | <0.001 |
| Nasogastric tube | 43.6 | 39.4 | <0.001 |
| Patients with devices/therapies, % | |||
| Enteral nutrition | 17.5 | 16.6 | <0.001 |
| Parenteral nutrition | 13.1 | 11.8 | <0.001 |
| Patients with infection, % | |||
| Community-acquired infection | 12.8 | 13.9 | <0.001 |
| Extra-ICU acquired infection | 8.3 | 8.7 | 0.015 |
| ICU-acquired infection | 13.8 | 11.3 | <0.001 |
| Other type of infection or unknown | 0.5 | 0.4 | 0.11 |
| Patients treated with antibiotics, % | |||
| For community-acquired infection | 17.5 | 18.3 | <0.001 |
| For extra-ICU acquired infection | 12.9 | 13.1 | 0.443 |
| For ICU-acquired infection | 13.7 | 11.9 | <0.001 |
| Prophylaxis | 26.4 | 26.7 | 0.134 |
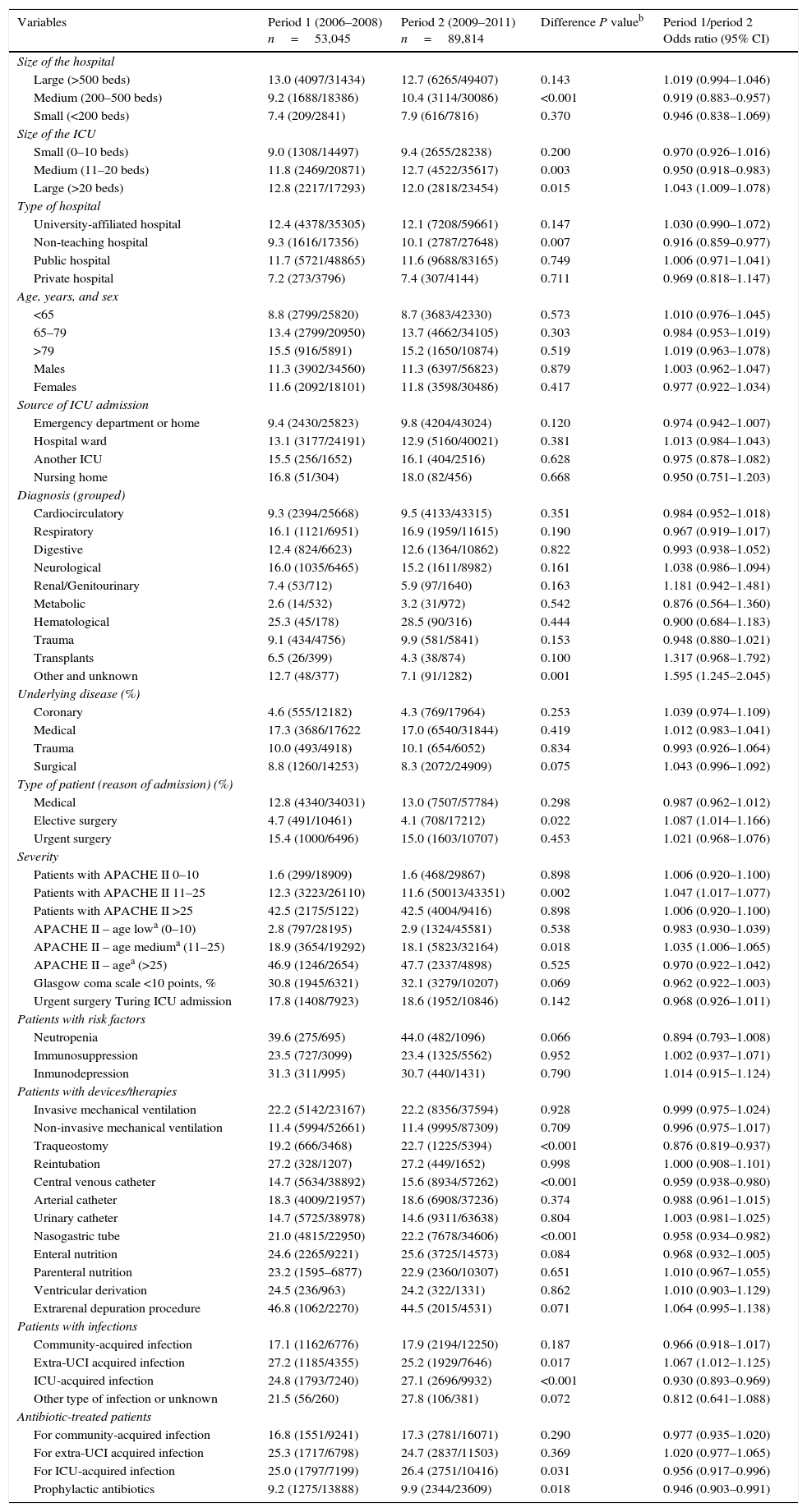
Univariate analysis of the differences in mortality according to the study period (2006–2008 vs. 2009–2011).
| Variables | Period 1 (2006–2008) n=53,045 | Period 2 (2009–2011) n=89,814 | Difference P valueb | Period 1/period 2 Odds ratio (95% CI) |
|---|---|---|---|---|
| Size of the hospital | ||||
| Large (>500 beds) | 13.0 (4097/31434) | 12.7 (6265/49407) | 0.143 | 1.019 (0.994–1.046) |
| Medium (200–500 beds) | 9.2 (1688/18386) | 10.4 (3114/30086) | <0.001 | 0.919 (0.883–0.957) |
| Small (<200 beds) | 7.4 (209/2841) | 7.9 (616/7816) | 0.370 | 0.946 (0.838–1.069) |
| Size of the ICU | ||||
| Small (0–10 beds) | 9.0 (1308/14497) | 9.4 (2655/28238) | 0.200 | 0.970 (0.926–1.016) |
| Medium (11–20 beds) | 11.8 (2469/20871) | 12.7 (4522/35617) | 0.003 | 0.950 (0.918–0.983) |
| Large (>20 beds) | 12.8 (2217/17293) | 12.0 (2818/23454) | 0.015 | 1.043 (1.009–1.078) |
| Type of hospital | ||||
| University-affiliated hospital | 12.4 (4378/35305) | 12.1 (7208/59661) | 0.147 | 1.030 (0.990–1.072) |
| Non-teaching hospital | 9.3 (1616/17356) | 10.1 (2787/27648) | 0.007 | 0.916 (0.859–0.977) |
| Public hospital | 11.7 (5721/48865) | 11.6 (9688/83165) | 0.749 | 1.006 (0.971–1.041) |
| Private hospital | 7.2 (273/3796) | 7.4 (307/4144) | 0.711 | 0.969 (0.818–1.147) |
| Age, years, and sex | ||||
| <65 | 8.8 (2799/25820) | 8.7 (3683/42330) | 0.573 | 1.010 (0.976–1.045) |
| 65–79 | 13.4 (2799/20950) | 13.7 (4662/34105) | 0.303 | 0.984 (0.953–1.019) |
| >79 | 15.5 (916/5891) | 15.2 (1650/10874) | 0.519 | 1.019 (0.963–1.078) |
| Males | 11.3 (3902/34560) | 11.3 (6397/56823) | 0.879 | 1.003 (0.962–1.047) |
| Females | 11.6 (2092/18101) | 11.8 (3598/30486) | 0.417 | 0.977 (0.922–1.034) |
| Source of ICU admission | ||||
| Emergency department or home | 9.4 (2430/25823) | 9.8 (4204/43024) | 0.120 | 0.974 (0.942–1.007) |
| Hospital ward | 13.1 (3177/24191) | 12.9 (5160/40021) | 0.381 | 1.013 (0.984–1.043) |
| Another ICU | 15.5 (256/1652) | 16.1 (404/2516) | 0.628 | 0.975 (0.878–1.082) |
| Nursing home | 16.8 (51/304) | 18.0 (82/456) | 0.668 | 0.950 (0.751–1.203) |
| Diagnosis (grouped) | ||||
| Cardiocirculatory | 9.3 (2394/25668) | 9.5 (4133/43315) | 0.351 | 0.984 (0.952–1.018) |
| Respiratory | 16.1 (1121/6951) | 16.9 (1959/11615) | 0.190 | 0.967 (0.919–1.017) |
| Digestive | 12.4 (824/6623) | 12.6 (1364/10862) | 0.822 | 0.993 (0.938–1.052) |
| Neurological | 16.0 (1035/6465) | 15.2 (1611/8982) | 0.161 | 1.038 (0.986–1.094) |
| Renal/Genitourinary | 7.4 (53/712) | 5.9 (97/1640) | 0.163 | 1.181 (0.942–1.481) |
| Metabolic | 2.6 (14/532) | 3.2 (31/972) | 0.542 | 0.876 (0.564–1.360) |
| Hematological | 25.3 (45/178) | 28.5 (90/316) | 0.444 | 0.900 (0.684–1.183) |
| Trauma | 9.1 (434/4756) | 9.9 (581/5841) | 0.153 | 0.948 (0.880–1.021) |
| Transplants | 6.5 (26/399) | 4.3 (38/874) | 0.100 | 1.317 (0.968–1.792) |
| Other and unknown | 12.7 (48/377) | 7.1 (91/1282) | 0.001 | 1.595 (1.245–2.045) |
| Underlying disease (%) | ||||
| Coronary | 4.6 (555/12182) | 4.3 (769/17964) | 0.253 | 1.039 (0.974–1.109) |
| Medical | 17.3 (3686/17622 | 17.0 (6540/31844) | 0.419 | 1.012 (0.983–1.041) |
| Trauma | 10.0 (493/4918) | 10.1 (654/6052) | 0.834 | 0.993 (0.926–1.064) |
| Surgical | 8.8 (1260/14253) | 8.3 (2072/24909) | 0.075 | 1.043 (0.996–1.092) |
| Type of patient (reason of admission) (%) | ||||
| Medical | 12.8 (4340/34031) | 13.0 (7507/57784) | 0.298 | 0.987 (0.962–1.012) |
| Elective surgery | 4.7 (491/10461) | 4.1 (708/17212) | 0.022 | 1.087 (1.014–1.166) |
| Urgent surgery | 15.4 (1000/6496) | 15.0 (1603/10707) | 0.453 | 1.021 (0.968–1.076) |
| Severity | ||||
| Patients with APACHE II 0–10 | 1.6 (299/18909) | 1.6 (468/29867) | 0.898 | 1.006 (0.920–1.100) |
| Patients with APACHE II 11–25 | 12.3 (3223/26110) | 11.6 (50013/43351) | 0.002 | 1.047 (1.017–1.077) |
| Patients with APACHE II >25 | 42.5 (2175/5122) | 42.5 (4004/9416) | 0.898 | 1.006 (0.920–1.100) |
| APACHE II – age lowa (0–10) | 2.8 (797/28195) | 2.9 (1324/45581) | 0.538 | 0.983 (0.930–1.039) |
| APACHE II – age mediuma (11–25) | 18.9 (3654/19292) | 18.1 (5823/32164) | 0.018 | 1.035 (1.006–1.065) |
| APACHE II – agea (>25) | 46.9 (1246/2654) | 47.7 (2337/4898) | 0.525 | 0.970 (0.922–1.042) |
| Glasgow coma scale <10 points, % | 30.8 (1945/6321) | 32.1 (3279/10207) | 0.069 | 0.962 (0.922–1.003) |
| Urgent surgery Turing ICU admission | 17.8 (1408/7923) | 18.6 (1952/10846) | 0.142 | 0.968 (0.926–1.011) |
| Patients with risk factors | ||||
| Neutropenia | 39.6 (275/695) | 44.0 (482/1096) | 0.066 | 0.894 (0.793–1.008) |
| Immunosuppression | 23.5 (727/3099) | 23.4 (1325/5562) | 0.952 | 1.002 (0.937–1.071) |
| Inmunodepression | 31.3 (311/995) | 30.7 (440/1431) | 0.790 | 1.014 (0.915–1.124) |
| Patients with devices/therapies | ||||
| Invasive mechanical ventilation | 22.2 (5142/23167) | 22.2 (8356/37594) | 0.928 | 0.999 (0.975–1.024) |
| Non-invasive mechanical ventilation | 11.4 (5994/52661) | 11.4 (9995/87309) | 0.709 | 0.996 (0.975–1.017) |
| Traqueostomy | 19.2 (666/3468) | 22.7 (1225/5394) | <0.001 | 0.876 (0.819–0.937) |
| Reintubation | 27.2 (328/1207) | 27.2 (449/1652) | 0.998 | 1.000 (0.908–1.101) |
| Central venous catheter | 14.7 (5634/38892) | 15.6 (8934/57262) | <0.001 | 0.959 (0.938–0.980) |
| Arterial catheter | 18.3 (4009/21957) | 18.6 (6908/37236) | 0.374 | 0.988 (0.961–1.015) |
| Urinary catheter | 14.7 (5725/38978) | 14.6 (9311/63638) | 0.804 | 1.003 (0.981–1.025) |
| Nasogastric tube | 21.0 (4815/22950) | 22.2 (7678/34606) | <0.001 | 0.958 (0.934–0.982) |
| Enteral nutrition | 24.6 (2265/9221) | 25.6 (3725/14573) | 0.084 | 0.968 (0.932–1.005) |
| Parenteral nutrition | 23.2 (1595–6877) | 22.9 (2360/10307) | 0.651 | 1.010 (0.967–1.055) |
| Ventricular derivation | 24.5 (236/963) | 24.2 (322/1331) | 0.862 | 1.010 (0.903–1.129) |
| Extrarenal depuration procedure | 46.8 (1062/2270) | 44.5 (2015/4531) | 0.071 | 1.064 (0.995–1.138) |
| Patients with infections | ||||
| Community-acquired infection | 17.1 (1162/6776) | 17.9 (2194/12250) | 0.187 | 0.966 (0.918–1.017) |
| Extra-UCI acquired infection | 27.2 (1185/4355) | 25.2 (1929/7646) | 0.017 | 1.067 (1.012–1.125) |
| ICU-acquired infection | 24.8 (1793/7240) | 27.1 (2696/9932) | <0.001 | 0.930 (0.893–0.969) |
| Other type of infection or unknown | 21.5 (56/260) | 27.8 (106/381) | 0.072 | 0.812 (0.641–1.088) |
| Antibiotic-treated patients | ||||
| For community-acquired infection | 16.8 (1551/9241) | 17.3 (2781/16071) | 0.290 | 0.977 (0.935–1.020) |
| For extra-UCI acquired infection | 25.3 (1717/6798) | 24.7 (2837/11503) | 0.369 | 1.020 (0.977–1.065) |
| For ICU-acquired infection | 25.0 (1797/7199) | 26.4 (2751/10416) | 0.031 | 0.956 (0.917–0.996) |
| Prophylactic antibiotics | 9.2 (1275/13888) | 9.9 (2344/23609) | 0.018 | 0.946 (0.903–0.991) |
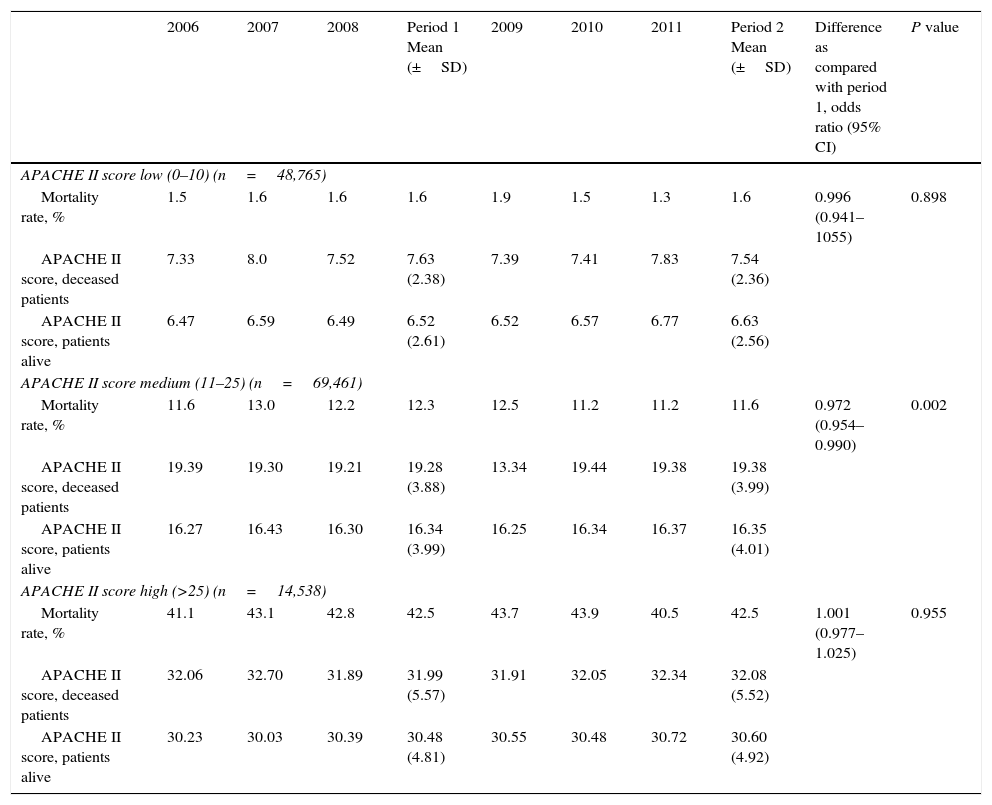
The mean values of the APACHE II score for each stratum of severity level for patients who died and patients who were discharged alive are shown in Table 6. Statistically significant differences in mortality rates between periods 1 and 2 were only found among those patients with APACHE II scores between 11 and 25 (mortality rate 12.3% vs. 11.6%, OR=0.972, 95% CI 0.954–0.990, P=0.002). In the multivariate analysis, predictors of mortality were the size of the ICU, source of the patient, reason for ICU admission, underlying illness, urgent surgery during ICU stay and ICU-acquired infection. When the three APACHE II strata were applied to the model, including the study period as a further independent variable, patients with APACHE II score between 11 and 25 had a lower mortality rate in period 2 as compared to period 1 (OR=0.931, 95% CI 0.883–0.982, P=0.008).
Secular trends of ICU crude mortality and APACHE II score stratified by severity level.
| 2006 | 2007 | 2008 | Period 1 Mean (±SD) | 2009 | 2010 | 2011 | Period 2 Mean (±SD) | Difference as compared with period 1, odds ratio (95% CI) | P value | |
|---|---|---|---|---|---|---|---|---|---|---|
| APACHE II score low (0–10) (n=48,765) | ||||||||||
| Mortality rate, % | 1.5 | 1.6 | 1.6 | 1.6 | 1.9 | 1.5 | 1.3 | 1.6 | 0.996 (0.941–1055) | 0.898 |
| APACHE II score, deceased patients | 7.33 | 8.0 | 7.52 | 7.63 (2.38) | 7.39 | 7.41 | 7.83 | 7.54 (2.36) | ||
| APACHE II score, patients alive | 6.47 | 6.59 | 6.49 | 6.52 (2.61) | 6.52 | 6.57 | 6.77 | 6.63 (2.56) | ||
| APACHE II score medium (11–25) (n=69,461) | ||||||||||
| Mortality rate, % | 11.6 | 13.0 | 12.2 | 12.3 | 12.5 | 11.2 | 11.2 | 11.6 | 0.972 (0.954–0.990) | 0.002 |
| APACHE II score, deceased patients | 19.39 | 19.30 | 19.21 | 19.28 (3.88) | 13.34 | 19.44 | 19.38 | 19.38 (3.99) | ||
| APACHE II score, patients alive | 16.27 | 16.43 | 16.30 | 16.34 (3.99) | 16.25 | 16.34 | 16.37 | 16.35 (4.01) | ||
| APACHE II score high (>25) (n=14,538) | ||||||||||
| Mortality rate, % | 41.1 | 43.1 | 42.8 | 42.5 | 43.7 | 43.9 | 40.5 | 42.5 | 1.001 (0.977–1.025) | 0.955 |
| APACHE II score, deceased patients | 32.06 | 32.70 | 31.89 | 31.99 (5.57) | 31.91 | 32.05 | 32.34 | 32.08 (5.52) | ||
| APACHE II score, patients alive | 30.23 | 30.03 | 30.39 | 30.48 (4.81) | 30.55 | 30.48 | 30.72 | 30.60 (4.92) | ||
The main contribution of the study is to provide information on the general characteristics of patients admitted to Spanish ICUs during a 6-year period. Also, a modest reduction in mortality according to severity levels of the APACHE II scale in non-selected patients was assessed. An updated case-mix analysis of patients admitted to Spanish ICUs with the extension here reported cannot be obtained from any of the registries currently running in our country. The lack of important variations in mortality could reflect the counterbalance between different facts: on one hand a higher age of the population along with a higher severity of the illness; and on the other hand, a potential improvement in their care mostly remarkable in the decrease of the rate of nosocomial infections. This consequence seems to be more relevant in patients with intermediate level of severity in whom prophylactic actions have probably a greater effect. Due to the big size of the sample the described differences are statistically significant, although they might not have any clinical relevance.
As far as we are aware, previous studies in large sample of ICU patients assessing case-mix in non-selected patients have not been previously published. Moreover, considering that the 188 participating ICUs account for near 60% of all beds available for critically ill patients in our country,24 the present information truly reflects the type of patients currently attended in the ICU setting. The predominance of patients referred from the emergency services (49.9%) determines the case-mix of ICU patients. In this respect, patients are more similar to those admitted to the ICU in countries from the European Union than those admitted in the United States,2,14,25–27 although the mean APACHE II score (close to 15) is more similar to USA. Different admission policies among ICUs and the existence of intermediate level care units in some hospitals, such as Stroke Care Units or Respiratory Intermediate Care Units, probably influenced on the type and severity of patients admitted to the ICUs of such centers. Descriptions of the case-mix in non-selected ICU patients from Southern European countries are lacking.
It should be noted the progressive increase in the mean age of the patients (61.3 years in 2006 vs. 62.4 years in 2011) at the expense of an increase in patients 80 years of age and older (10.9% in 2006 vs. 12.7% in 2011). This finding reflects modifications in the Spanish pyramid population, in which aging of the population of 1.5 years per decade has been documented, despite the arrival of immigrants, which is in general a younger population (data of the National Institute of Statistics, http://www.ine.es/prensa/np756.pdf). This may also indicate a more permissive admission of older patients as reported in other studies.28–31
Only 32.9% of patients were admitted for the postoperative control of an elective or urgent surgical procedure, which shows the load represented by postsurgical conditions in ICUs participating in the ENVIN-HELICS registry. It is also interesting the increase in transplant recipients admitted in the immediate postoperative period after transplantation or because of complications of the procedure. The mean length of ICU stay has been shortened slightly (6.72 vs. 6.51 days) and seems to be unrelated to the patients’ severity, as previously demonstrated,13 so this decrease may be due to the influence of several factors (care pressure, better care facilities in the wards, saving policies or adequacy of life sustaining measures). The use of devices also changed, with a reduction in the use of more invasive techniques, such as invasive mechanical ventilation or parenteral nutrition, in the benefit of less invasive techniques, which agrees with expert recommendations.32 It is remarkable the increasing use of the non-invasive mechanical ventilation through the years.
Intra-ICU mortality rate has apparently remained unchanged. However, a reduction in mortality may be expected by advances in the patient's care and diagnostic/therapeutic techniques and, particularly, as a result of a marked reduction nosocomial infections related to the implementation of projects to prevent catheter-related bloodstream infection21 and mechanical ventilation-associated pneumonia. In fact, the percentage of patients with ICU-acquired infections decreased from 13.7% to 11.9%. By contrast, the increase in patient's age and especially in the severity of illness as measured by the APACHE II score would have been accompanied by an increase in mortality. However, when patients were stratified by the APACHE II scores and adjusted by other confounding variables, mortality was significantly lower (comparing period 1 to period 2) only in the group of APACHE II score between 11 and 25, with an absolute and relative reductions of mortality of 0.7% and 5.7%, respectively. That is, patients with lower severity continued to have a low mortality rate and those with higher severity a high mortality rate. The mortality variation in the intermediate group could not have a big clinical relevance, but it also could mean that the resources aimed to treat this group could be the most beneficial. This analysis has not been designed specifically to study the relationship between the decline in mortality and the implementation of measures for the prevention of nosocomial infections, but the results suggest that there might be a direct relationship.
Other authors have reported decreases in mortality in specific groups of critically ill patients.11,16–18,33,34 Zimmerman et al.16 reported a relative reduction of 35% of hospital mortality in critically patients admitted to hospitals in the United States between 1988 and 2012, although this decrease was mainly attributable to reductions of mortality between 1998 and 2003, whereas it was much more modest and less relevant (0.6%) between 2004 and 2012. Changes in mortality according to severity levels were not analyzed.
The limitations of the study are inherent to the voluntary participation and multicentric characteristics of the registry, which is designed to assess nosocomial infection rates rather than case-mix. Therefore, we are presenting a secondary analysis and the conclusions should be interpreted cautiously. Life Support Withholding and Withdrawing policies were not considered, as well as the discharge to Intermediate Care Units, which may have affected both the percentage of patients who died and the length of stay in the ICU.35 Although mean APACHE II scores were annually assessed, we assumed that other factors that may influence upon mortality in critically ill patients,36 such as the number of patients with malignancies or septic complications (septic shock or adult respiratory distress syndrome) did not vary during the study period, although this aspect was not examined. It is also assumed that during the 6-year study period, important changes in the overall care of critically ill patients did not occur, although mortality in some particular groups of patients may have decreased as a consequence of changes in clinical practice. In the ENVIN-HELICS registry only patients admitted for over 24h are registered. The lack of information about those deceased in less than 24h might condition a non-evaluated workload
The potential effect of the inclusion of new ICUs in the ENVIN-HELICS registry on the case-mix was controlled by a multilevel analysis as well as the importance of each individual on mortality.37 The use of the APACHE II score is justified because these severity scores are routinely used in our country. Data on length of stay and hospital ward-related mortality should be considered with caution due to a possible selection bias. On the other hand, the extremely high number of hospitals, units and patients included in the registry is the main strength of the study, which in turn is a faithfully reflection of the current status of intensive care medicine in our environment, minimizing the limitations of the study as well as between-subject variability of observations.38 The quality of the registered data has been confirmed.23
ConclusionThis study provides observational longitudinal data on a case-mix of patients admitted to Spanish ICUs over a 6-year period (2006–2011). In recent years, patients were somewhat older, with a higher severity level and submitted to less invasive procedures. A modest reduction in ICU mortality rate was observed among patients with APACHE II scores between 11 and 25 (intermediate severity level), without variations of mortality in the low (APACHE II score <11) or high (APACHE II score >25) levels.
The present study emphasizes the next three points: (a) the need to adjust the resources to treat older patients; (b) the benefit of focusing therapeutic efforts on moderately ill patients in order to achieve better outcomes; and (c) the convenience of encouraging the use of non-invasive therapeutic methods.
Conflict of interestThe authors declare that they have no conflict of interest. Annual reporting and statistical analyses were supported by Sanofi-Aventis (years 2006 and 2007), the Ministry of Health, Social Services and Equality (year 2008), Novartis (years 2009 and 2010) and Pfizer (year 2011) but none of these pharmaceutical companies and the governmental body participated in the any phases of the study or interpretation of the results.
The authors are grateful to all Intensive Care Unit physicians who have collaborated in the project entering information in the database of the ENVIN-HELICS registry, to J.J. Otal, MD, from the Service of Epidemiology and Preventive Medicine of Hospital Universitari Vall d’Hebron, Barcelona, who validated the information included in the registry, analyzed the data and served as the technical secretariat of the registry, to Urko Aguirre Larracoechea of the Research Unit of Galdakao-Usansolo hospital and Health Services Research on Chronic Patients Network (REDISSEC) for his contribution to the statistical analysis, and to the Quality Agency of the Ministry of Health, Social Policy and Equality and Aventis, Novartis and Pfizer for financial support for website and server database maintenance as well as publication of the annual reports. We thank Marta Pulido, MD, for editing the manuscript and editorial assistance.
ANDALUCIA: Hospital de Traumatología Virgen del Rocío; Clínica Santa Isabel; Hospital de Valme.; Hospital Virgen de la Macarena; Hospital San Juan de Dios de Aljarafe, Hospital General Carlos Haya. Hospital Comarcal de la Axarquía; Hospital Universitario Virgen de la Victoria. Hospital Universitario Médico Quirúrgico de Jaén; Hospital San Juan de la Cruz. Hospital San Agustín; Hospital Neurotraumatológico de Jaén; Hospital Clínico San Cecilio; Hospital Médico Quirúrgico Virgen de las Nieves; Centro Rehabilitación y Traumatología Virgen de las Nieves. Hospital General Básico de Baza. Hospital General Básico Santa Ana de Motril; Hospital Médico Quirúrgico Virgen de las Nieves; Hospital Universitario Puerta del Mar; Hospital de Jerez; Hospital Universitario de Puerto Real; Hospital de Antequera; Hospital Reina Sofía; Hospital Valle de los Pedroches; Hospital Infanta Margarita; Hospital General Juan Ramón Jiménez; Hospital Infanta Elena; Hospital de Riotinto; Hospital Torrecárdenas. Hospital de Poniente; Hospital Comarcal La Inmaculada. ARAGON: Hospital General Miguel Servet. Hospital Clínico Universitario Lozano Blesa de Zaragoza (U. Quirurgica); Hospital Clínico Universitario Lozano Blesa (UCI médica); Hospital Clínico Universitario Lozano Blesa (U. Central); Hospital Royo Villanova; Hospital General San Jorge; Hospital de Barbastro; Hospital Obispo Polanco. ASTURIAS: Hospital Central de Asturias; Hospital General de Asturias. Hospital Central de Asturias (INS); Hospital de Cabueñes; Hospital de San Agustín; Hospital Valle del Nalón. IllES BALEARS: Hospital on Espases; Clínica Palmaplanes; Hospital Son Llàtzer; Fundación Hospital de Manacor; Clínica Rotger; Hospital Can Misses; Hospital Verge del Toro. ISLAS CANARIAS: Hospital Universitario Insular de Gran Canaria; Hospital Universitario de Gran Canaria Doctor Negrín (U. Coronaria); Hospital Universitario de Gran Canaria Doctor Negrín (U. Neurotrauma); Hospital Universitario de Gran Canaria Doctor Negrín (U. Polivalente); Hospital General Lanzarote; Hospital Universitario de Canarias; Hospital Ntra. Sra. de Candelaria. CANTABRIA: Hospital Marqués de Valdecilla (UCI 1). Hospital Marqués de Valdecilla (UCI 2 Politrauma); Hospital Marqués de Valdecilla (UCI 3). EUSKADI: Hospital Santiago Apóstol de Vitoria; Hospital de Txagorritxu; Hospital Donostia (Ntra. Sra. de Aranzazu); Hospital de Basurto; Hospital de Galdakao-Usansolo (UCI); Hospital Universitario Cruces; Santa María de la Asunción; Hospital de Galdakao-Usansolo (U. Reanimación). CASTILLA-LA MANCHA: Virgen de la Salud; Hospital Provincial de la Misericordia de Toledo; Hospital Ntra. Sra. del Prado. Talavera; Hospital General de Albacete; Hospital Santa Bárbara; Hospital General de Ciudad Rea; Hospital General Universitario de Guadalajara; Hospital Virgen de la Luz de Cuenca. CASTILLA Y LEON: Hospital del Rio Hortega; Hospital Clínico Universitario de Valladolid; Hospital Virgen de la Vega; Hospital Clínico de Salamanca; Hospital General Santa Bárbara de Soria; Hospital General de Segovia; Hospital General Yagüe; Hospital de León (Reanimación); Hospital de León (UCC); Hospital de León (UCI); Complejo Hospitalario de Palencia (H.G. Río Carrión); Virgen de la Concha. CATALUNYA: Hospital General d’Hospitalet (Unitat Semi-intensivos); Hospital General de Catalunya; Hospital General Vall d’Hebron (UCI); Hospital General Vall d’Hebron (UCC); Hospital de Traumatologia Vall d’Hebron (UCI); Hospital General Vall d’Hebron (UPCC); Hospital Clínic (UCI Quirúrgica); Hospital Asepeyo. Sant Cugat del Vallés; Hospital Santa Creu i Sant Pau (U. Polivalente); Centro Médico Delfos; Hospital del Mar; Hospital Dos de Maig; Hospital Universitari Sagrat Cor; Hospital de Bellvitge (UCI); Hospital de Bellvitge. (UCC); Parc Sanitari Sant Joan de Déu (H. Sant Boi); Hospital de Barcelona (SCIAS); Hospital General d’Hospitalet (Creu Roja); Hospital de Traumatologia Vall d’Hebron (U.Quemados); Hospital Mutua de Terrassa; Hospital de Terrassa; Hospital Parc Taulí de Sabadell; Consorci Sanitari de Mataró; Hospital de Sant Joan Despí Moisès Broggi; Fundación Althaia, Manresa; Hospital Comarcal de Igualada; Hospital General de Granollers; Clínica Girona; Hospital Universitari Doctor Josep Trueta. Hospital Universitario Arnau de Vilanova de Lleida; Hospital Universitari de Sant Joan; Hospital de Tortosa Verge de la Cinta; Hospital de Meritxell. Escaldes-Engordany. Andorra; EXTREMADURA: Hospital Don Benito-Villanueva; Hospital San Pedro de Alcántara. Hospital Virgen del Puerto. Plasencia; GALICIA: Complejo Hospitalario Universitario Juan Canalejo (UCI); Hospital Clínico Universitario de Santiago (UCI Médica); Hospital Arquitecto Marcide; Hospital Cristal Piñor. Compleixo Hospitalario de Ourense; Hospital Sta. Mª Nai. Compleixo Hosp. de Ourense; Hospital Montecelo; Hospital Xeral Cies; Hospital Povisa; Hospital Meixoeiro (UCI); Hospital de Meixoeiro (UCC); Hospital Xeral-Calde. LA RIOJA: Complejo Hospitalario San Millán San Pedro. MADRID: Hospital Clínico Universitario San Carlos (U. Médico-Quirúrgica); Hospital Clínico Universitario San Carlos (U. Neuro-Politrauma); Fundación Jiménez Díaz; Clínica Puerta de Hierro; Hospital Clínico Universitario San Carlos (UCI). Hospital Militar Gómez Ulla; Clínica Moncloa; Hospital Universitario 12 de Octubre (UCI); Hospital Universitario 12 de Octubre. (UCI Trauma); Hospital General de Móstoles; Hospital Severo Ochoa; Hospital del Henares; Hospital de Getafe; Hospital Infanta Cristina; Hospital Universitario 12 de Octubre (UCP); Hospital Sanitas La Moraleja; Hospital de la Princesa (UCI Quirúrgica); Hospital de la Princesa (UCI); Hospital Fuenlabrada; Hospital de Sureste; Hospital del Tajo; Hospital Infanta Sofía; Hospital Infanta Leonor. MURCIA: Hospital Virgen de la Arrixaca; Hospital Morales Meseguer; Hospital Santa Lucía; Hospital Santa María del Rosell; Hospital General Universitario Reina Sofía de Murcia; Hospital Rafael Méndez. MELILLA: Hospital comarcal de Melilla. NAVARRA: Hospital de Navarra; Hospital Virgen del Camino; Hospital de Estella “Garcia Orcoyen”; Clínica San Miguel. PAIS VALENCIÀ: Hospital Universitario La Fe; Hospital Arnau de Vilanova; Hospital Doctor Peset; Hospital de Sagunto; Hospital de la Ribera. Hospital Clínico Universitario de Valencia (U. Reanimación); Hospital de Torrevieja Salud; Hospital Virgen de la Salud de Elda; Hospital General Universitario de Alicante (UCI); Hospital Universitario de Elche; Hospital General Universitario de Alicante (U. Reanimación); Hospital de Sant Joan de Alicante; Hospital Vega Baja; Hospital General de Castellón; Hospital Comarcal de Vinaròs; Hospital de la Plana. Villareal.
Members of the ENVIN-HELICS Study Group at http://hws.vhebron.net/envin-helics/. Participating ICUs and hospitals are listed in the appendix.