Left ventricular diastolic dysfunction is a common finding in critically ill patients. It is characterized by a progressive deterioration of the relaxation and the compliance of the left ventricle. Two-dimensional and Doppler echocardiography is a cornerstone in its diagnosis.
Acute pulmonary edema associated with hypertensive crisis is the most frequent presentation of diastolic dysfunction critically ill patients. Myocardial ischemia, sepsis and weaning failure from mechanical ventilation also may be associated with diastolic dysfunction.
The treatment is based on the reduction of pulmonary congestion and left ventricular filling pressures. Some studies have found a prognostic role of diastolic dysfunction in some diseases such as sepsis.
The present review aims to analyze thoroughly the echocardiographic diagnosis and the most frequent scenarios in critically ill patients in whom diastolic dysfunction plays a key role.
La disfunción diastólica del ventrículo izquierdo es un hallazgo frecuente en pacientes críticos. Se caracteriza por una alteración progresiva de la relajación y la complianza del ventrículo izquierdo. La ecocardiografía bidimensional y doppler juega un papel primordial en su diagnóstico.
El edema agudo de pulmón asociado a una crisis hipertensiva es la presentación más frecuente de la disfunción diastólica en pacientes críticos. La isquemia miocárdica, la sepsis y el fracaso del destete de la ventilación mecánica también pueden asociarse a la disfunción diastólica.
El tratamiento se basa en la reducción de la congestión pulmonar y en disminuir las presiones de llenado del ventrículo izquierdo. Algunos estudios han hallado un papel pronóstico de la disfunción diastólica en algunas afecciones como la sepsis.
La presente revisión procura analizar en profundidad el diagnóstico ecocardiográfico y las enfermedades del paciente crítico en las que la disfunción diastólica juega un papel clave.
Heart failure (HF) is a major public health problem due to the huge economics and social costs involved. Despite improvements in the treatment of cardiovascular diseases over the past years, prevalence, survival and mortality of HF have marginally changed.1
HF can be defined as an abnormality of cardiac structure or function leading to failure of the heart to deliver oxygen according to the requirements of the tissues, despite normal filling pressures, or only at the expense of increased filling pressures.2
Symptoms of HF are non-specific (breathlessness, orthopnoea, paroxysmal nocturnal dyspnea, reduced exercise tolerance, fatigue) and do not help to discriminate between HF and other problems. Signs of HF are also not specific (tachycardia, tachypnea) and many result from sodium and water retention (peripheral edema, pulmonary crepitations, elevated jugular venous pressure, hepatojugular reflux, ascites).
A change has occurred in the clinical–hemodynamic profile of patients with HF in the past decade. HF has classically been associated with impaired systolic function, however is now recognized that both, systolic and diastolic function, play a key role in its pathophysiology.3
The term diastolic heart failure refers to the conjunction of signs and symptoms of HF, preserved left ventricular ejection fraction and diastolic dysfunction, but it is currently replaced by the term HF with preserved ejection fraction.4
Nowadays HF with preserved ejection fraction accounts for as many as 35–50% of all cases of HF. Furthermore readmission and mortality rates are similar to those observed in patients with HF with reduced ejection fraction.5 HF with preserved ejection fraction patients are older and more commonly female, with greater hypertension, obesity, anemia, and atrial fibrillation compared to those with HF with reduced ejection fraction.6
HF is a common feature in intensive care unit (ICU) patients, occurring in about 30% of cases.7 In critically ill patients signs and symptoms of HF are non-specific, therefore the study of cardiac function, invasively or non-invasively, is crucial to the proper treatment of patients. ICU patients have frequently predisposing factors associated with diastolic dysfunction: related to patient's history (advanced age, female sex, hypertension, obesity), diseases (myocardial ischemia, arrhythmia, sepsis) or treatments applied (volume resuscitation, mechanical ventilation).8,9 The purpose of this article is to provide an overview of the diagnosis and role of diastolic dysfunction in ICU patients, condition that is underestimated, mainly because it is underdiagnosed.
PathophysiologyLeft ventricular diastole extends from the closure of the aortic valve to the closure of the mitral valve, and its duration, at rest, is usually two-thirds of the cardiac cycle. The first diastolic phase, after closing the aortic valve to the opening of the mitral valve, is the isovolumetric relaxation time. During this period, the intraventricular pressure decreases rapidly before the ventricular filling begins.
Ventricular filling includes three phases in patients with sinus rhythm. The early filling phase begins with the opening of the mitral valve due to the reduction of intraventricular pressure below the atrial pressure. During the second phase, or equilibrium phase, the ventricular volume remains constant due to the equalization of the atrio-ventricular pressure. Finally, the late filling phase depends on the increase in atrial pressure due to the atrial contraction.
Several physiological parameters interact during ventricular diastole.10 Among these, the most fundamental are ventricular relaxation characteristics, compliance, and atrial contraction.11,12
Relaxation of cardiac muscle fibers is an active property that uses energy as adenosine triphosphate (ATP). This energy is required to transfer the cytoplasmic calcium back to the sarcoplasmic reticulum, reactivating the inhibitory effect of troponin-tropomyosin complex and allowing the dissociation of actin and myosin filaments. Relaxation not only depends on the availability of energy, but also on the abundance of calcium in the cytoplasm. The effect of the relaxation of the cardiac muscle fibers is a sudden drop in left ventricular pressure. The rate at which pressure decreases during the isovolumetric relaxation period directly reflects the rate of muscle fibers relaxation. This velocity can be measured with invasive techniques and is often defined as the maximum descent velocity (−) dP/dt or the time constant of isovolumetric relaxation (tau).13
Compliance depends on the relationship between the stretching of the myocardial fiber and stress (force applied by surface). This association is affected by active relaxation of the sarcomeres and the relative content of elastic and collagen fibers in the connective tissue. These fibers determine the size and the anatomical shape of the left ventricle, and configure the matrix that convert the shortening and lengthening of muscle fibers in pressure changes.14 The force required to stretch the fibers is initially low, but increases geometrically as the fibers are stretched. This phenomenon explains that, even in normal subjects, excessive volume overload can result in heart failure.15
Left atrial function depends on its preload, afterload and contractility.16 In patients with abnormal ventricular relaxation atrial preload is increased, leading to a greater atrial ejection volume. This mechanism allows to maintain cardiac output in patients with impaired ventricular relaxation. The development of atrial fibrillation can lead to a decrease in cardiac output and the onset of congestive symptoms in these subjects. Atrial contraction is ineffective when ventricular compliance is reduced, since the volume of the atrial ejection pass in retrograde direction in the absence of valves in pulmonary veins.
The combination of active relaxation and passive myocardial compliance allow to maintain a stroke volume and cardiac output adequate with normal filling pressure. In diastolic dysfunction one or both of these properties are altered and left atrial pressure should be increased to maintain an adequate cardiac output.17
Diagnosis of diastolic dysfunctionSigns and symptoms are the same in case of systolic or diastolic dysfunction, so it is necessary tools like cardiac catheterization, echocardiography and natriuretic peptides to diagnose diastolic dysfunction.
Cardiac catheterization remains the gold standard for the diagnosis of diastolic dysfunction,9 but we cannot underestimate the consequences of its invasiveness and the risk to use it as a routine tool.18,19
EchocardiographyAdvances in echocardiography, its noninvasive, safe and easy use, have allowed Doppler echocardiography to become a cornerstone for the diagnosis of diastolic dysfunction in clinical practice.20 Nowadays the use of cardiac catheterization is indicated in case when Doppler echocardiography has not been sufficient to establish the diagnosis or additional information will be needed to guide treatment.3
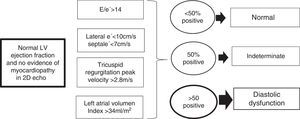
The most important points to make the echocardiographic diagnosis of diastolic dysfunction are (Fig. 1 and video in electronic supplementary material)21:
- 1.
2-D echocardiography.
- A)
Left atrial size and volume: a left atrial maximum volume index >34mL/m2 supports the presence of elevated left ventricular filling pressures. A normal left atrial volume is present in the earliest stage of diastolic dysfunction and in case of acute increase of left ventricular filling pressures.21
- B)
Left ventricular and interventricular septum size. Ventricular hypertrophy is not always present, the absence of hypertrophy do not exclude the diastolic dysfunction.20
- C)
Left ventricular ejection fraction and left ventricular wall motion abnormalities.22
- A)
- 2.
Pulse wave Doppler (PW): PW Doppler measures the velocity of intracardiac blood flow generated by the pressure gradient between two chambers, and it is usually expressed in cm/s. Transmitral PW Doppler at the tip of the mitral valve, in sinus rhythm, identifies two waves during left ventricular filling. First wave (E) corresponds to the early diastolic passive filling of the left ventricle. Second wave (A) corresponds to the atrial contraction. In normal diastolic function, passive ventricular filling component has a greater importance than the atrial contraction, so echocardiography shows an E wave maximal velocity higher than the A wave.21 However isolated transmitral PW Doppler parameters are not recommended to diagnose diastolic dysfunction, as E wave maximal velocity is highly dependent on volume status, reflecting not only the left ventricular diastolic function but the cardiac filling condition too.23
- 3.
Tissue Doppler Imaging (TDI): TDI is performed in apical view. The sample volume should be positioned within the septal and lateral insertion sites of the mitral leaflets and adjusted to cover the longitudinal excursion of the mitral annulus in both systole and diastole. TDI measures the velocity of change in myocardial length, and it is usually expressed in cm/s. In normal patients TDI allows to acquire the systolic (S), the early diastolic (e′) and the late diastolic velocities (a′). The e′ wave is considered to be indicative of left ventricular relaxation since it is less sensitive to loading conditions than PW Doppler.21
- 4.
Peak velocity of tricuspid regurgitation measured by continuous Doppler: During development of diastolic dysfunction, the left ventricular impaired relaxation can be transmitted to right chambers, resulting in a pulmonary arterial hypertension. Pulmonary arterial pressure significantly increased for each step-up in diastolic dysfunction grade.24 Peak velocity of tricuspid regurgitation more than 2.8m/s is associated to diastolic dysfunction and elevated left atrial pressure, once primary lung diseases have been ruled out.21 The sample volume should be positioned in correct angulation respect to the tricuspid regurgitation jet. Additionally right atrium pressure must be estimated assessing inferior vena cava size and response to breathe.24
New recommendations for the evaluation of left ventricular diastolic function by echocardiography have been recently published.21 The new guidelines recommend the use of several and more specific measures to diagnose diastolic dysfunction in patients without evidence of myocardial disease in 2-D echocardiography and preserved left ventricular ejection fraction (Fig. 2). While in the past guidelines17 the presence of a simple lateral e′ could be sufficient to diagnose diastolic dysfunction, the new guidelines recommend to take into account the following four variables when determining whether left ventricular diastolic function is normal or abnormal in absence of myocardial disease in 2-D echocardiography.21
- -
Annular e′ velocity (septal e′<7cm/s, lateral e′<10cm/s), E/e′ ratio (average>14, septal >15, lateral>13)
- -
LA maximum volume index>34mL/m2, and
- -
Peak velocity of tricuspid regurgitation>2.8m/s.
- -
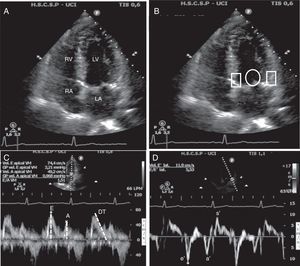
Echocardiographic assessment of left ventricular diastolic function. (A) Apical four-chamber view. In this view must check the left atrium volume and size and the left ventricle and septum size. (B) Apical four-chamber view, circle shows position where pulse wave Doppler has to be placed to measure transmitral flow, whereas rectangles show position where tissue Doppler must be placed to measure the velocity of change in myocardial length. (C) Pulse wave mitral Doppler at the tip of the mitral valve showing a normal diastolic pattern with a biphasic velocity profile E and A waves. Measurement of E wave deceleration time. (D) Tissue Doppler measurement at the lateral insertion site of the mitral leaflets shows the diastolic e′ and a′ waves and systolic s′ wave. LA, left atria; RA, right atria; LV, left ventricle; RV, right ventricle; DT, deceleration time.
In patients without evidence of myocardial disease in 2-D echocardiography and preserved left ventricular ejection fraction, left ventricular diastolic function is normal if more than half of the available variables do not meet the cutoff values for identifying abnormal function. LV diastolic dysfunction is present if more than half of the available parameters meet these cutoff values. The study is inconclusive if half of the parameters do not meet the cutoff values.21
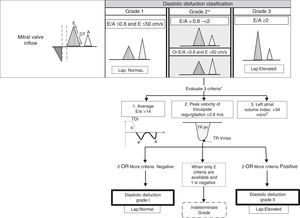
E wave along with e′ (E/e′ ratio) has been used to estimate left ventricular filling pressures, E/e′ ratio lower than 8 predicts a normal left ventricular filling pressures.25 An E/e′ above 15 in spontaneously breathing patients25 and 12 in mechanically ventilated patients26 correlates well with elevated filling pressures. When E/e′ is between 8 and 12 other echocardiographic indices should be used to estimate left ventricular filling pressures as left atrial enlargement or pulmonary venous flow. Recent studies however have questioned the E/e′ accuracy, particularly in patients with preserved left ventricular ejection fraction.27 Furthermore the new guidelines have changed the proposed algorithm for the estimation of left ventricular filling pressures (Fig. 3), emphasizing the measurement of the ratio E/A.
Estimation of left ventricular filling pressures and grades of diastolic dysfunction according to findings in Doppler echocardiography in patients with depressed left ventricular ejection fraction and patients with myocardial disease and normal left ventricular ejection fraction. DT, deceleration time; TDI, Tissue Doppler imaging; TR, tricuspid regurgitation; LAP, left atrial pressure.
Another important issue is to grade the severity of diastolic dysfunction. Although the grading scale remains unchanged, the new guidelines have changed the proposed practical approach to grade diastolic dysfunction (Table 1 and Fig. 3). The grading scale is mild or grade I (impaired relaxation pattern), moderate or grade II (pseudonormal), and severe or grade III (restrictive filling). This graduation correlates with of all-cause mortality. Even in asymptomatic patients with grade I diastolic dysfunction a 5-fold higher mortality was seen compared with normal diastolic function patients.17 To grade diastolic dysfunction should take into account mainly E/A ratio, mitral E wave peak velocity, E/e′ ratio, tricuspid regurgitation peak velocity and left atrial volume index.
Echocardiographic findings according to diastolic dysfunction grade.
| Normal | Grade I | Grade II | Grade III | |
|---|---|---|---|---|
| Mitral E/A ratio | ≥0.8 | ≤0.8 | >0.8 to <2 | >2 |
| Average E/e′ ratio | <10 | <10 | 10–14 | >14 |
| Peak TR velocity (m/s) | <2.8 | <2.8 | >2.8 | >2.8 |
| LA volume index | Normal | Normal or increased | Increased | Increased |
| LV relaxation | Normal | Impaired | Impaired | Impaired |
| LAP | Normal | Low or normal | Elevated | Elevated |
TR: tricuspid regurgitation, LA: left atria, LV: left ventricle, LAP: left atrial pressure.
In patients with grade I diastolic dysfunction, there is a left ventricular impaired relaxation, but normal left ventricular filling pressures, there is no rapid left ventricular diastolic suction, left atria emptying depends on left atrial contraction.21 Grade II represents impaired myocardial relaxation with mild to moderate elevation of left ventricular filling pressures. There is left ventricular relaxation impairment (large E wave) and mildly elevated left atrial pressure (smaller A wave). With valsalva manoeuver, that increases intrathoracic pressure, resulting in a decrease in left ventricular preload and left atrial pressure, improves artificially the relaxation, resulting in a change in E/A ratio, from E>A to the E<A (Fig. 3).21 Severe diastolic dysfunction (grade III) presents with elevated left ventricular filling pressure, the mitral valve is forced to open early due to high left atrial pressure, but there is a rapid equilibration with the high resting left ventricular diastolic pressure resulting in a rapid deceleration time of E.22 Left ventricular filling pattern may revert to impaired relaxation with successful therapy in some patients (grade IIIa), whereas in others, left ventricular filling remains restrictive (grade IIIb). This is an ominous finding and predicts a high risk for cardiac morbidity and mortality.17 Left atrial volume is increased in grades II and III of diastolic dysfunction, but can be within normal limits in grade I.
Supplementary echocardiographic methods that can help to evaluate diastolic dysfunction include:
- 1.
Transmitral color Doppler flow propagation velocity: in 2-D echocardiography apical four-chamber views, use the transmitral PW at the tip of the mitral valve with Color Doppler m-mode imaging. It shows a semi-quantitate velocity and rate of blood flow from the mitral valve annulus to the left ventricular apex (early diastolic color m-mode wave). The slope of this wave (Vp) is normally vertical. When diastolic dysfunction is worsening this slope become flatter because the increasingly impaired left ventricular relaxation.22
- 2.
Spectral Doppler pulmonary venous flow: it shows the impairment of rapid flow through the pulmonary veins into the left atria when there is an elevation of left ventricular filling pressures.22
In case of atrial fibrillation the assessment of diastolic dysfunction could be challenging due to the elevated heart rate, irregular R-R intervals and loss of atrial contraction (A wave of PW Doppler). Measurements from at least 5 cardiac cycles are mandatory. Septal e′<8cm/s, E mitral wave deceleration time less than 150ms, E/e′> 11, peak velocity of tricuspid regurgitation>2.8m/s and lack of E wave velocity variations despite varying R-R intervals, are all echocardiographic signs of elevated left atrial pressure in the setting of atrial fibrillation.21
BiomarkersCardiac biomarkers like brain natriuretic peptide (BNP) and N-terminal proBNP (NTproBNP) are used for the serologic diagnosis of HF in outpatients, especially in the non-acute setting or when echocardiography is not immediately available.
Natriuretic peptides (BNP and NTproNBP) are secreted in response to volume overload and increased cardiac wall stretch.28 In case of HF with preserved ejection fraction BNP levels can be lower or normal compared with patients with systolic HF.3 In non-critically ill patients with clinical or suspected HF with preserved ejection fraction, elevated BNP or NTpro-BNP levels unequivocally confirm the diagnosis and predict a worse outcome similarly than in patients with HF with reduced ejection fraction.29 Natriuretic peptide concentrations could be affected by confounding factors that may weaken their diagnostic utility in HF. Among them, atrial fibrillation, age and renal failure are the most important factors that may increase natriuretic peptide levels.30 On the other hand, natriuretic peptide concentrations may be disproportionally low in obese patients.31
Our group has demonstrated that both, BNP and NTproBNP, are useful screening tools to detect the existence of advanced degrees of diastolic dysfunction and, overall, to rule out elevated filling pressures in ICU patients.32
New promising biomarkers in HF are constantly emerging. Galectin-3 is secreted by activated macrophages and stimulates myofibroblast proliferation, macrophage migration, myocardial fibrosis, inflammation, cardiac remodeling and left ventricular dysfunction.33 Galectin-3 concentrations are increased in patients with HF with preserved ejection fraction. Increased concentrations are associated with poor prognosis and are well correlated with echocardiographic parameters of diastolic dysfunction and seem to be non-inferior to NTproBNP.34
Copeptin, a pre-provasopressin precursor, has been found to be elevated in patients with HF.35 Elevated plasma copeptin in HF has been associated with adverse outcomes such as increased mortality, risk of hospitalization and correlates with the severity of HF.36 Nevertheless, copeptin plasma concentration is not correlated with echocardiographic parameters of diastolic dysfunction.37 There is still no definite evidence to recommend the new biomarkers (e.g. galectin-3, copeptin, adrenomedullin, ST2) for clinical practice.38
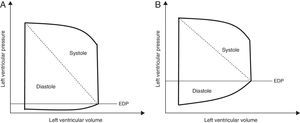
Clinical usefulness of the evaluation of diastolic function in critically ill patientsThe incidence of diastolic dysfunction in selected populations of critically ill patients is estimated to vary between 40 and 80%32,39–44 (Table 2). Compared with normal diastolic function, patients with diastolic dysfunction have a deviation in the left ventricle pressure–volume curve leading to exaggerated increases and decreases in left ventricular pressure for the same change in afterload and preload (Fig. 4). This results in hypertensive crisis and acute pulmonary edema when an increase in preload or afterload occurs, or hypotension and azotaemia when there is a decrease in pre or afterload. There are several clinical situations where diastolic dysfunction could play a key role in ICU patients, worsening the evolution and prognosis of these patients. Among them are: acute pulmonary edema, cardiac ischemia, severe sepsis and weaning from mechanical ventilation.
Incidence of diastolic dysfunction in critically ill patients.
| Author | Patients (N) | Characteristics | Incidence | Observations |
|---|---|---|---|---|
| Rolando 201539 | 60 | ICU patients with sepsis and septic shock. | 84% | The E/e′ ratio and SOFA score were independent predictors of mortality. |
| Zapata 201432 | 86 | ICU patients at admission | 58% | 70% had grade I, 12% grade II and 18% grade III. |
| Moschietto 201240 | 68 | ICU patients during weaning from MV | 48% | E/e′ ratio was higher in the failed group (80%) than in the successful group (35%). |
| Landesberg 201242 | 206 | ICU patients with sepsis and septic shock | 40.4% | Reduced mitral annular e′ velocity was the strongest predictor of mortality. |
| Papanikolaou 201143 | 50 | ICU patients during weaning from MV | 54% | 26% had grade I (57%failed SBT) and 74% grade II–III (80% failed SBT) |
| Sturgess 201044 | 21 | ICU patients with sepsis and septic shock | 57% | 25% grade I, 58% grade II and 17% grade III. E/e′ is an independent predictor of hospital survival, better than cardiac biomarkers. Fluid balance and diastolic dysfunction were independent predictors of BNP concentration in septic shock. |
| Bouhemad 200841 | 54 | ICU patients with sepsis and septic shock | 50% | The diastolic dysfunction in survivors was resolved together with normalization of troponin cTnI. |
MV: mechanically ventilation, SBT: spontaneous breathing trial, ICU: intensive care unit.
The diagnosis of acute pulmonary edema due to HF with preserved ejection fraction requires the presence of signs and symptoms of HF, normal systolic function (left ventricular ejection fraction>50% and left ventricular end-diastolic volume index<97mL/m2) and evidence of diastolic dysfunction.45
The deviation in left ventricular pressure–volume curve in diastolic dysfunction may lead to abrupt pulmonary edema secondary to various precipitating factors as volume overload, tachycardia (due to anemia, fever or hypovolemia) rhythm disturbances (due to electrolyte imbalances) or hypertensive crisis.
Hypertensive acute pulmonary edema is the usual presentation in ICU patients.46 Gandhi et al.47 demonstrated isolated variations in diastolic function with no variation in parameters of systolic function in patients presenting with acute pulmonary edema as a consequence of severe arterial hypertension. These findings suggest that diastolic dysfunction was the sole mechanism of decompensation. The 50% of the patients presenting acute pulmonary edema had a preserved ejection fraction.
Myocardial ischemiaMyocardial ischemia, along with hypertensive crisis, is one of the main precipitating mechanisms of diastolic dysfunction.9 Myocardial ischemia and derived arrhythmias may lead to a significant decrease in myocardial relaxation and aggravate the degree of diastolic dysfunction.9 Physiological studies in animal models undergoing induced ischemia have evidenced that diastolic dysfunction was presented before systolic dysfunction. If no severe myocardial injury has been established, the diastolic dysfunction normalized after reperfusion. On the other hand, animals with myocardial infarction and preserved ejection fraction remained in impaired relaxation pattern and those with myocardial infarction and depressed ejection fraction showed a pseudonormal pattern secondary to reduced compliance and increased end-diastolic pressures.48
SepsisMyocardial dysfunction is a common complication in patients with sepsis or septic shock, characterized by deterioration of biventricular contractility and relaxation, thus altering systolic and diastolic function. This is the most complex organ sepsis-induced failure to characterize because of the dynamic evolution due to the adaptation of cardiovascular system to the disease process and resuscitation treatment.
The pathophysiology is complex and multifactorial including systemic, intra and extracellular mechanisms like abnormal distribution of coronary blood flow due to nitric oxide metabolism deregulation, excess of proinflammatory cytokines, calcium metabolism deregulation and hypoxia. These changes finally lead to an impairment in the contractility (systolic dysfunction) and relaxation (diastolic dysfunction) of both ventricles.49
Incidence of diastolic dysfunction related to septic shock is around 20–56%,41,50 and is considered an independent predictor of early mortality.42 Left ventricular diastolic dysfunction can complicate hemodynamic management of patients with severe sepsis or septic shock due to a poor clinical response to fluid challenges.42,51 While fluids are one of the most important therapies to improve hemodynamic in septic shock, in patients with diastolic dysfunction and non-compliant left ventricles the positive fluid balance may aggravate lung congestion and non-cardiogenic pulmonary edema leading to pulmonary hypertension and hypoxemia. Mahjoub et al.52 showed a significant increase in E/e′ after volume expansion in patients with sepsis induced diastolic dysfunction and non-responders to fluid challenge, which translates an increase in left ventricular filling pressures. Whereas patients with diastolic dysfunction and responders to fluid challenges showed an increase in e′ but not in E/e′, suggesting that left ventricular relaxation can be improved in preload dependent patients.
The presence of diastolic dysfunction is not a contraindication to apply the standard therapy in the early resuscitation of sepsis and septic shock53–55 but its presence should alert the caregiver to have a more delicate approach during the resuscitation, making a continuous assessment of cardiovascular preload and response to volume expansion.56
Weaning from mechanical ventilationMany asymptomatic outpatients with early stages of diastolic dysfunction develop symptoms due to a deterioration of diastolic function during exercise. Similarly spontaneous breathing trial (SBT) with low levels of pressure support or T-tube as a stress test, may cause HF symptoms even in patients with early stages of diastolic dysfunction.
Pulmonary artery catheter remains the gold standard to clearly identify the onset of HF during SBT57,58 since the diagnosis focuses on demonstrate a marked increase in pulmonary artery occluded pressure during the weaning trial. This elevation is related to the increase in venous return secondary to the shift from positive to negative intrathoracic pressure and to increased sympathetic activity, to the reduction in left ventricular compliance, and to the increase in left ventricular afterload.
Advances in echocardiography in critically ill during the past decade have enabled to replace the pulmonary artery catheter in this setting. Lamia et al.59 were the firsts to compare echocardiography with pulmonary artery catheter, and demonstrate that echocardiography was helpful to detect the cardiac origin of weaning failure. Classically weaning induced pulmonary edema has been related to systolic dysfunction. Lamia showed in a selected population of chronic obstructive pulmonary disease patients that systolic function was unchanged in patients that suffered from a weaning induced pulmonary edema, whereas parameters related to diastolic dysfunction, as E/A and E/e′, predicted a pulmonary artery occluded pressure elevation during SBT. The combination of E/A>0.95 and E/e′ 8.5 at the end of SBT was accurate to diagnose a weaning induced pulmonary edema. Similarly data were obtained by Dessap et al.,60 Caille et al.61 and our group62 showing that in patients failing the weaning process due to cardiogenic edema the E/A and E/e′ significantly increase during SBT, pointing out the key role of diastolic dysfunction in weaning failure. In fact the presence of diastolic dysfunction before SBT can predict the weaning failure as showed the study of Papanikolaou43 where the E/e′>7.8 measured at the lateral portion of the mitral annulus before SBT had a high accuracy (88%) to predict the weaning failure. Moschietto et al.40 showed that patients who failed the weaning process had a lower e′, and slightly higher E/e′ before SBT than patients who successfully passed the SBT. Ten minutes after starting the SBT, successful patients where capable to maintain the E/e′ ratio thanks to a proportional increase in both E and e′. On the other hand patients who failed the weaning could not face the increase in E (due to increased venous return) with a proportional increase in e′ (due to a diastolic dysfunction) resulting in an elevated E/e′ suggestive of an increase in left ventricular filling pressures.
A recent published meta-analysis showed that diastolic dysfunction, characterized by an increased E/e′ ratio, before a SBT, is associated with weaning failure. However a cut-off value for E/e′ to predict the weaning outcome has not been identified.63
These findings suggest that echocardiography could be another tool to guide the weaning process, helping to decide the best therapy (diuretics in case of fluid overload, nitrates infusion, beta-blockers) to achieve success.
Management of diastolic dysfunction in ICUNo treatment has yet been shown to reduce morbidity and mortality in patients with HF with preserved ejection fraction.38
Treatment of HF with preserved ejection fraction can be summarized in 2 steps.13
First, treatment should target in symptoms reduction by decreasing cardiac preload. This target will be achieved by lowering left ventricular volume (diuretics, nitrates), blunting neurohormonal activation – which will contribute to decrease afterload – (angiotensin converting enzyme inhibitors, angiotensin receptor blockers, aldosterone antagonist), maintaining the atrial contraction and preventing tachycardia (β-blockers, calcium channel blockers). The use of β-blockers is controversial. The SENIORS trial with Nevibolol showed that its use improves the prognosis of patients older than 70 years independently of the ejection fraction.64 Regarding the angiotensin receptor blockers, only Candesartan has showed to reduce hospital admission due to HF in patients with preserved ejection fraction.65 The SUPPORT trial showed that the combination of angiotensin receptor blockers (Olmesartan), with angiotensin converting enzyme inhibitors, and β-blockers is not recommended due to the increase in mortality and renal dysfunction.66
Second, treatment should target the concomitant cardiovascular disease (hypertension, coronary artery disease, atrial fibrillation) and non-cardiovascular diseases (diabetes, chronic kidney disease, anemia, iron deficiency, chronic obstructive pulmonary disease and obesity),67 as well as the precipitating causes (acute coronary syndrome, hypertensive emergency, rapid arrhythmias or severe bradycardia etc.).38
Positive inotropic agents are generally not used in the treatment of patients with isolated HF with preserved ejection fraction. Moreover positive inotropic agents have the potential to worsen the pathophysiological processes that cause diastolic dysfunction.13 The utility of digitalis in HF with preserved ejection fraction remains unclear. While some data suggest that patients with HF and normal ejection fraction in sinus rhythm may have fewer symptoms and hospitalizations when they are treated with digitalis,68 digoxin may produce an increase in systolic energy demands and an overload of calcium in diastole. These effects, in hemodynamic stress or ischemia situation, may promote diastolic dysfunction.69
In the acute setting of ICU patients no specific studies focused on treatment of decompensated HF with preserved ejection fraction exist. Treatment of decompensated HF due to diastolic dysfunction is still based on a reduction in pulmonary congestion and correction of the precipitating factors. Hypertensive crisis could be managed with high doses of nitrates or calcium antagonists. Hypervolemia may require diuretics or ultrafiltration. Beta-blockers, digoxin or diltiazem may be used in rapid atrial fibrillation or tachycardia.23
Whenever the therapy was applied a close monitorization is needed in these patients in whom a delicate balance between excessive pulmonary congestion and reduced preload exists. Future studies focused in the treatment of diastolic dysfunction in the different settings (sepsis, weaning induced HF) are needed.
Prognosis value of diastolic dysfunctionWhile in the general population the prognostic value of HF with preserved ejection fraction has been extensively studied, in the setting of ICU patients is just beginning to be studied. A meta-analysis has showed that non-ICU patients with HF with preserved ejection fraction have a lower risk of death than HF with reduced ejection fraction.70
Few studies have examined the prognostic value of diastolic dysfunction in general ICU patients. Our group found relationship between advanced degrees of diastolic dysfunction and morbidity (in terms of ICU length of stay and days on mechanical ventilation), but not between dysfunction and mortality.32 Ikonomidi's group found that left ventricular diastolic dysfunction, assessed by TDI, was an independent predictor of mortality in general ICU patients.71
In burn patients a significant correlation between left ventricular diastolic dysfunction and in-hospital mortality exists.72 In these patients inflammatory citokines (IL-6 and TNF-α) may be associated with diastolic dysfunction.
In critically ill patients, the prognostic value of diastolic dysfunction has been widely studied in the setting of sepsis and septic shock, and inconsistent results have been found. Whereas Landesberg et al., Sturgess et al. and Rolando et al.39,42,44 found a higher mortality in case of diastolic dysfunction associated with severe sepsis and septic shock; Pulido et al. and Brown et al.50,73 found no relationship between diastolic dysfunction an prognosis in sepsis. These results may have been given by differences in populations, diagnostic criteria and patients’ age. Recently, a meta-analysis including 636 septic patients has confirmed the association between mortality and diastolic dysfunction with a risk ratio of 1.82.74 However, in this same meta-analysis systolic dysfunction has not been associated with mortality in septic patients (risk ratio 0.93).
Until larger studies clarify the prognostic role of diastolic dysfunction, its presence in a critically ill patient should warn the clinicians for a close hemodynamic monitoring. This is especially relevant since proper pharmacologic treatment often ameliorates the signs and symptoms of diastolic dysfunction.
ConclusionsDiastolic dysfunction is a common feature in ICU patients. Echocardiography plays a key role in the diagnosis of diastolic dysfunction in critically ill patients, because it is easy to use at bedside and can be repeated, is non-invasive and increasingly available in intensive care units. In fact the use of echocardiography to evaluate the diastolic dysfunction is a basic competence to be acquired during training in echocardiography in intensive care medicine.75–77 Others tools like brain natriuretic peptides are useful as screening test. Diastolic dysfunction could be the reason for ICU admission as acute pulmonary edema or stand as a breakthrough complication of another process (myocardial ischemia, sepsis, weaning from mechanical ventilation) worsening the evolution of these patients. Use of routine echocardiography can help to identify early stages of diastolic dysfunction, and repeated echocardiography throughout the ICU stay could help to adjust the therapy, and improve prognosis of our patients. Epidemiologic studies regarding diastolic dysfunction are needed in ICU patients in order to know the magnitude of the problem and to better understand those scenarios were diastolic dysfunction could worsen the patient's outcome.
FundingNone declared.
Conflict of interestThe authors have no conflict of interest to disclose.