The standard method for cardiac output measuring is thermodilution although it is an invasive technique. Transesophageal Echocardiography (TEE) offers a dynamic and functional alternative to thermodilution.
ObjectiveAnalyze concordance between two TEE methods and thermodilution for cardiac output assessment.
MethodsObservational concordance study in cardiovascular surgery patients that required pulmonary artery catheter. TEE cardiac output measurement at both mitral annulus (MA) and left ventricle outflow tract (LVOT) were performed. Results were compared with thermodilution. Correlation was evaluated by Lin's concordance correlation coefficient and Bland–Altman analysis. Statistical analysis was undertaken in STATA 13.0.
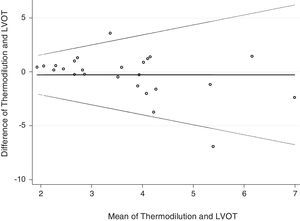
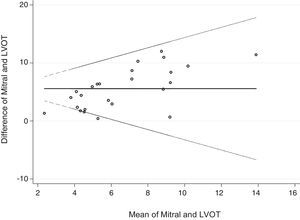
ResultsTwenty-five patients were enrolled. Fifty two percent of patients were male, median age and ejection fraction was 63 years and 35% respectively. Median thermodilution, LVOT and MA -measured cardiac output was 3.25 L/min, 3.46 L/min and 8.4 L/min respectively. Different values between thermodilution and MA measurements were found (Lin concordance=0.071; Confidence Interval 95%=−0.009 to 0.151; Spearman's correlation=0.22) as values between thermodilution and LVOT (Lin concordance=0.232; Confidence Interval 95%=−0.12 a 0.537; Spearman's correlation 0.28). Bland–Altman analysis showed greater difference between MA measurements and thermodilution (DM=−0.408; Bland–Altman Limits=−0.809 to −0.007), than the other echocardiographic findings (DM=0.007; Bland–Altman Limits=−0.441 to 0.428).
ConclusionResults from cardiac output measurement by doppler and 2D-TEE on both MA and LVOT do not correlate with those obtained by thermodilution.
El cálculo del gasto cardiaco se realiza por termodilución, y su principal desventaja es el carácter invasivo. La ecocardiografía transesofágica (ETE) representa una alternativa dinámica y funcional a la termodilución.
ObjetivoAnalizar la concordancia entre dos métodos de ETE y termodilución para la evaluación del gasto cardiaco.
MétodosEstudio observacional de concordancia en pacientes de cirugía cardiovascular con requerimiento de catéter de arteria pulmonar. Se realizó medición de gasto cardiaco por ETE en anillo mitral (AM) y en el tracto de salida del ventrículo izquierdo (TSVI). Los resultados se compararon con la termodilución. La concordancia fue evaluada por el coeficiente de correlación concordancia de Lin y analizada por el método de Bland-Altman. Los análisis estadísticos se realizaron en STATA 13.0.
ResultadosSe incluyeron 25 pacientes. El 52% fueron hombres, con mediana de edad de 63años y fracción de eyección del 35%. La mediana de gasto cardiaco por termodilución, AM y TSVI fue de 3,25, de 3,46 y de 8,4L/min, respectivamente. Se encontraron diferentes valores entre termodilución y AM (concordancia de Lin=0,071; IC95%: −0,009 a 0,151), así como entre termodilución y TSVI (concordancia de Lin=0,232; IC95%: −0,12 a 0,537). El análisis de Bland-Altman muestra una diferencia entre la medición por AM y termodilución importante (DM=−0,408; Bland-Altman Limits=−0,809 a −0,007), así como entre las dos medidas por ETE (DM=0,007; Bland-Altman Limits=−0,441 a 0,428).
ConclusiónLos resultados en la medición del gasto cardiaco por doppler y ETE bidimensional tanto a nivel del anillo mitral como del TSVI no son concordantes con la termodilución.
Historically, cardiac output calculation for adults has been measured through thermodilution using a pulmonary artery catheter. This became the standard measurement method around 1970, and so it remained for more than ten years, until a high frequency of complications and/or misinterpreted data were associated to high mortality rates related to this technique.1,2
The first alternative to replace thermodilution was suggested by Dr. Parisi, who measured ventricle volume and ejection fraction using a two-dimensional transesophageal echocardiography (TEE).1,3 Other methods have been proposed (e.g. arterial wave contour analysis, PiCCO, transpulmonar thermodilution, transpulmonary lithium dilution),4 although they have shown questionable benefit during open-heart cardiovascular surgery.
A recent promising possibility is TEE, which allows both cardiac structure and function evaluation during perioperative open-heart surgery. However, it requires training and certain skills to be learned by the operator in order to allow him or her to interpret different results adequately, and using them to guide management and improve care for a critically ill patient.5–7
Currently, TEE cardiac output monitoring is most commonly performed through a deep transgastric long axis view and aortic ring measurement (LVOT),1 procedure that requires skills, and could be associated with gastrointestinal, bleeding and mortality risk, besides of increased costs.8,9
Considering potential risk and cost associated with aortic ring measurement, we propose an alternative method through TEE four chamber view, measuring flow across mitral annulus (MA).
The main objective of this study is to evaluate concordance among three different cardiac output measurement methods including LVOT, MA and thermodilution.
MethodsThis is a concordance observational study, approved by the ethics committee. Enrolled patients were told before surgery about postoperative TEE hemodynamic data analysis study and gave informed consent. Twenty-five patients programmed to undergo cardiovascular procedures (myocardial revascularization, atrial septal defect closure, aortic or mitral valve replacement) in the Hospital Cardiovascular de Cundinamarca are included in the study. Cardiac output, systolic function and pulmonary pressure were measured immediately in the postoperative period. Those patients with esophageal diseases, prosthetic mitral or aortic valve insufficiency and those with atrial fibrillation history were excluded from the study.
Perioperative managementThe following are simply monitored by means of a visuscope: pulse oximetry, capnography, invasive arterial blood pressure, esophageal thermometer, central catheter if the patient's condition warrants it, and pulmonary artery catheter to measure the cardiac output by thermodilution using the bolus thermodilution cold saline solution technique, and using the B650 and G Caresscape monitors from the 37B650-01 series. Transesophageal echocardiography probe was gently moved, and the following equipment was used: the Philips Sonos 7500 live 3D Echo and 5.0 and 6.5 MZ Omni-Plane Transducer, a one-meter long Hewlett Packard probe M-mode, two dimensional, color-flow Doppler echocardiography, pulsed wave and continuous Doppler, and harmonic imaging. The anesthetic technique and the use vasoconstrictors/inotropes were decided by the anesthesiologist in charge of the case.
One cardiovascular anesthesiologist with training in TEE certified by the European Association of Cardiothoracic Anaesthesiologists (EACTA) performed all TEE cardiac output measurements during the immediate postoperative period (sternal closure), avoiding inotropic or vasopressor support during the study.
Measurement of cardiac output on the mitral annulus/left ventricle outflow tractAll postoperative TEE cardiac output measures were done using the following formula; regardless the type of surgery performed considering clinical practice standards:
The following formula was used for cardiac output measurement.
where Cardiac Output (CO)=Stroke Volume×Heart rate; Ejection fraction or Stroke volume (SV) or Flow=AT×VTI; Cross sectional area (AT)=D2×0.785 (cm2); D2=mitral annulus or left ventricle outflow tract; VTI=velocity time integral (cm).Mitral annulusThe probe is inserted at a depth of 28 – 30cm and the mid esophageal four chamber window at zero degrees measures the cross-section of the mitral annulus, which was the result of measuring the diameter from edge to edge during the diastole at the moment when the mitral valves or prosthesis was at their maximum aperture. The probe's second speed was then used and it was multiplied by 0.785, which is a quarter of Pi (3.1416). This is undertaken on the assumption that the mitral annulus is circular and the cross section is constantly in diastole. The cardiac output was the product of the VTI for the diastolic mitral flow and this was measured with pulsed wave Doppler on the coaptation surface of the valve; color-flow images were used to keep the ultrasonic beam parallel to the mitral flow. The correction for the angle of incidence was taken into consideration for all the measurements and was less or equal to 20°. Three measurements were made consecutively, tracing was done manually, and the average was multiplied by the cross section of the mitral annulus: this gives the stroke volume that is subsequently multiplied by the heart rate.
Left ventricle outflow tract (LVOT)The cross section of the LVOT was measured in the mid-esophagus in the window on the aortic valve level on the longitudinal axis from 130 - 135°. LVOT was identified between 5mm and 10mm of the aortic ring and the diameter was measured from edge to edge during the diastole at the moment when the mitral valves or prosthesis was at its maximum aperture. The probe's second speed was then used and it was multiplied by 0.785, which is a quarter of Pi (3.1416).
To measure the VTI, the probe was inserted between 45–50cm and located in the deep transgastric window at zero degrees from the LVOT. Color-flow Doppler was used to keep the ultrasound beam parallel to the flow, the wave flow Doppler was positioned directly on the LVOT, 5mm – 10mm from the aortic ring, and the velocity time integral was manually traced. Three different samples were gathered and the average of the results was taken. This was then multiplied by the second speed of the cross section and then by 0.785, which corresponds to a quarter of Pi (3.1416). This result was in turn multiplied by the heart rate that could be measured at that particular moment.
ThermodilutionWith a maximum lapse of five minutes between echocardiographic measurements, the cardiac output measurement was taken by thermodilution using CVP from a pulmonary artery catheter, using the bolus thermodilution technique injecting 10 cc of cold saline solution. Three samples were taken and then a mean of the results was calculated, excluding those that were extreme (very high or very low). A second observer undertook this procedure who was not aware of the previous echocardiographic measurements.
All the data from TEE and thermodilution measurements was registered along with demographic features, procedure type and EuroSCORE II.
Statistical analysis took into consideration patients’ demographic and clinical characteristics, which were summarized with their frequencies, central tendencies, and dispersion. To calculate the correlation between two cardiac output measuring methods, Lin's concordance correlation coefficient was used, as was the Bland–Altman limits of agreement after logarithmic transformation considering the possibility of scarcity of data and great variation of differences. The statistical analysis of the information was undertaken using Stata13.
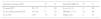
ResultsThe demographic characteristics of the 25 patients are outlined in Table 1. The median age was 63 years (predominant age group: 51–64, 44%). The median ejection fraction was 35%; males were the prominent sex in the study (52%). The cardiac output measurement median by thermodilution was 3.25 liters/minute, while the cardiac output measurement median on the left ventricle outflow tract was 3.46 liters/minute, and on the mitral ring was 8.4 liters/minute (Fig. 1). The most common procedure undertaken was the valve replacement (48%). The majority of patients were in the group with the lowest ejection fraction that was less than 35% (Table 2).
Demographic characteristics of the included patients.
| Patients’ characteristics | Range | Median | P25–P75 |
|---|---|---|---|
| Age (years) | 20–79 | 63 | 56–69 |
| Ejection fraction (%) | 20–65 | 35 | 30–60 |
| C.O. thermodilution (L/min) | 1.93–6.87 | 3.25 | 2.58–4.46 |
| C.O. mitral annulus (L/min) | 3.01–19.6 | 8.4 | 5.81–12.52 |
| C.O. LVOT (L/min) | 1.58–8.85 | 3.46 | 2.17–5.07 |
| Surface area (m2) | 1.32–2 | 1.58 | 1.44–1.66 |
| EuroSCORE II | 1.22–19.2 | 4.8 | 3.5–8.19 |
| Heart rate (beats/min) | 55–109 | 80 | 70–85 |
Note: C.O=cardiac output; LVOT=left ventricle outflow tract; L/Min=liters/minute.
Ejection fraction and EuroSCORE index II by ranges.
| Ejection fraction (EF) | N° | % | EuroSCORE II | N° | % | |
|---|---|---|---|---|---|---|
| Normal EF | 50–75 | 7 | 28 | Low (0–2) | 5 | 20 |
| Lower than normal EF | 36–49 | 5 | 20 | Middle (3–5) | 12 | 48 |
| Low EF | <35 | 13 | 52 | High (>6) | 8 | 32 |
Relation between ejection fraction and EuroSCORE II.10
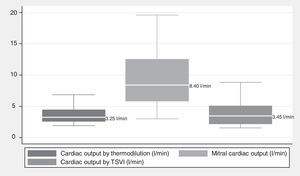
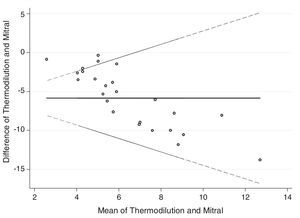
On evaluating the concordance between the three measurements by means of Lin's concordance-correlation coefficient, we found that there was no concordance between the three measurements. Specifically, the thermodilution values differ from the values obtained from the mitral ring flow rate (Lin concordancev0.071; Confidence Interval 95%=−0.009 to 0.151; Spearman's correlation=0.22) (Table 3). In addition, the values that were obtained from the LVOT showed important discrepancies with those obtained by thermodilution (Lin concordance=0.232; Confidence Interval 95%=−0.12 a 0.537; Spearman's correlation 0.28) (Table 3). Due to scarcity of data and great variation of the differences, a logarithmic transformation of data was used to estimate the Bland–Altman limits of agreement. The average differences between the cardiac output values are more importantly marked in the comparison between thermodilution versus mitral annulus (DM=−0.408; Bland–Altman Limits=−0.809 to −0.007) (Fig. 2) than the other echocardiographic findings (DM=0.007; Bland–Altman Limits=−0.441 to 0.428) (Figs. 3–4).
Concordance coefficients in the three cardiac output measurements.
| Lin's concordance correlation coefficient | Confidence intervala | Spearmans's Correlation | Differences in measurements (standard deviation)c | Bland–Altman Limitsb | |
|---|---|---|---|---|---|
| Thermodilution vs. LVOT | 0.232 | −0.127 to 0.537 | 0.28 | −0.007 (0.222) | −0.441 to 0.428 |
| Thermodilution vs. mitral valve | 0.071 | −0.009 to 0.151 | 0.22 | −0.408 (0.205) | −0.809 to −0.007 |
| Mitral valve vs. LVOT | 0.147 | 0.017 to 0.270 | 0.37 | 0.401 (0.210) | −0.011 to 0.813 |
Note: LVOT=left ventricle outflow tract.
Cardiac output calculation is routinely carried out by thermodilution, which presents widely disseminated and evaluated parameters.1,8,11,12 Its invasiveness and related complications led the searching for alternative techniques with lower mortality and adverse events.
Transesophageal echocardiography cardiac output measurement is an alternative in hemodynamic monitoring allowing guidance during these patients management according to cardiac output, stroke volume, preload, cardiac structure and function evaluation.7 Measurement can be taken through different routes, including pulmonary ring, aortic ring, mitral ring level, and on the LVOT with pulsed wave and continuous Doppler.8,13–15 However, differences can be found among measured routes. LVOT correlates with thermodilution,16 although its technical difficulty to align the transducer parallel in a deep transgastric window and the anteflexion that requires, is associated to increased mortality rate.1,17,18
Our study deals with this problem, obtaining an image by TEE on a window level with four chambers via the mid-esophagus at zero degrees on the mitral ring level, where the ultrasonic beam is aligned in parallel measuring the transmitral flow, calculating ring area diameter.
However, the information obtained from 25 patients did not show concordance among three cardiac output measurements (thermodilution, MA and LVOT). Of the three measurements estimated, the closest were those that came from thermodilution with the flow through TSVI, showing a concordance between them but without being consistent for all the patients
From our results, we cannot recommend thermodilution replacement by any of the other measurements derived from TEE. We can only suggest to monitor trends based on the initial value and during subsequent measurements, taking advantage of the complementary information that the TEE offers, which thermodilution alone does not.
Our results are similar to those presented by Bettex et al. They found that cardiac output evaluation was 9.57 L/min (range of 6.4 – 12.5 L/min) compared with thermodilution.1 Likewise, Muhiudeen's study measured cardiac output by cross section diameter at a pulmonary ring level and found a modest correlation with thermodilution, but no correlation was found at the mitral ring level, as well as an important dispersion of the data close to zero (r=0.24).13 Conversely, Cabrera et al. found a strong correlation between cardiac output measurement on the mitral ring level among Chilean population (Pearson's R=0.92); however, this study measured an area on a transgastric level at zero degrees with a light anteflexion. This provided a transversal view of the mitral valve during ventricular diastole, which is calculated using a planimetric measurement under an elliptical model and not a circular one.11,19,20
Cabrera et al. suggested that mitral stenosis, severe mitral insufficiency or insufficiency in prosthetic valves could be a constraint for the application of this technique, including only patients undergoing myocardial revascularization. However, the authors of this study used a different technique for cross section measurement than they did when they measured the mitral ring by planimetric measurement in the transgastric window with a level of anteflexion, considering that cross section diameter measurement is a primary limitation for the mitral ring as it might overestimate cardiac output.
Study strengths include that all three measurements were done in a similar way, with high quality windows, following the same steps, and with a difference of no more than five minutes between TEE and thermodilution measurements. Other hemodynamic influences were avoided, and similarity in demographic characteristics for ejection fraction and type of surgery were documented. In order to avoid possible bias, TEE results were kept apart from those from thermodilution.
One of the limitations of this study was that the electrocardiogram was not available; therefore, it could not be included with the TEE image during the measurement at the precise moment of the rapid diastolic filling peak. This could generate an estimated variability of up to 12% in the mitral ring area size.11,20 Also, the fact that the probe was not continuously available meant that the size of the sample could not be improved, being a small sample size another limitation of the present study. However, the sample obtained was sufficient to observe differences in concordance among measurement methods. We also note that thermodilution, as the standard practice, is susceptible to errors given that it is not the reference standard to measure cardiac output; It has been quantified that this process can overestimate the output by up to 15%.1,5,6,21 It was, however, necessary to make the comparison with this measuring method, as it is the most commonly used for patients who undergo cardiac surgery.
Studied population had a mean ejection fraction of 39.8% and was predominantly intermediate to high-risk patients according to EuroSCORE II. The former analysis being important, considering that myocardial wall movement abnormalities may alter up to 40% the two-dimensional volume evaluation, and may be related to a high degree of variability in the results.1
According to TEE calculations to estimate cardiac output, heart rate is an important determinant for variation. If tachycardia is present, a TEE-cardiac output measurement overestimation may happen. This consideration should be taken into account in patients with altered heart rate.
Our findings showed that results on a mitral ring level are dispersed respect to thermodilution and LVOT; with a 5.8 L/min difference compared to thermodilution. However, during difficulties for catheter introduction, lack of training or when clinical conditions preclude TEE-transgastric window, MA four chamber method may offer a cardiac output estimation, information about left ventricle inflow related to ejection fraction deterioration and be monitored over time, compared with thermodilution and LVOT.
Transesophageal echocardiography cardiac output measuring methods might be of complementary value during heart surgery, taken into account their limitations, during postoperative monitoring.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Special thanks is given to the Anesthesiology Department led by Dr. Jorge Córdoba, the Cardiology Department, Dr. Álvaro Rodríguez for his unconditional tutoring, to the Department of Epidemiology directed by Dr. Leonardo Cely, and especially to Dr. Leonidas Olaya who is Scientific Director of the Hospital Cardiovascular del Niño de Cundinamarca. He allowed us to undertake the study and offered us the possibility to pioneer many more studies in this institution that wholeheartedly supports the vulnerable population in our country – Colombia.