Arterial catheterization is a frequent procedure in Intensive Care Units (ICUs). Accidental catheter removal (ACR) can cause severe and potentially life-threatening complications such as severe bleeding and vascular damage. Few data are available on accidental arterial catheter removal, and no studies have been found comparing the incidence of ACR between different arterial catheter sites.
ObjectiveTo compare the incidence of ACR in femoral and radial arterial catheters.
Research designRetrospective study.
SettingA polyvalent ICU.
SubjectsAll consecutive patients subjected to femoral or radial arterial catheterization.
MeasuresThe incidence of ACR per 100 catheter-days between groups was compared using Poisson regression. We considered ACR as the presence of unintended removal produced by the patient or healthcare personnel.
ResultsA total of 2419 radial and 1085 femoral arterial catheters were inserted and remained in situ during 14,742 and 6497 days, respectively. We detected 45 cases of ACR with the femoral access and 162 cases with the radial access. The ACR rate was lower with the femoral access (4.1% vs 6.7% in the case of the radial access; p=0.003). Poisson regression analysis confirmed a lower incidence of ACR with the femoral versus the radial access (0.69 vs 1.10 ACR events per 100 catheter-days; OR 0.6, p=0.006, CI95% 0.01-0.83).
ConclusionsThe incidence of ACR was found to be lower with the femoral than with the radial arterial catheters. In order to improve patient safety, it could be interesting to exhaustively monitor the incidence of ACR and adopt preventive measures, since ACR can give rise to serious complications.
La cateterización arterial es un procedimiento frecuente en los pacientes de las Unidades de Cuidados Intensivos (UCI). La retirada accidental del catéter (ACR) puede conllevar graves complicaciones, potencialmente vitales, como la hemorragia y la lesión vascular. Existen pocos datos sobre la ACR de los catéteres arteriales y no hemos encontrado estudios que hayan comparado la incidencia de ACR entre los diferentes accesos de canalización arterial.
ObjetivoComparar la incidencia de ACR entre los catéteres arteriales localizados en el acceso femoral y radial.
Diseño del estudioEstudio retrospectivo.
LugarUna UCI polivalente.
SujetosTodos los pacientes consecutivos sometidos a canalización de arteria femoral o radial.
MedidasLa incidencia de ACR por 100 días de catéter entre grupos fue comparada mediante la regresión de Poisson. Se consideró ACR cuando se producía la retirada no programada del catéter por parte del propio paciente o por el personal.
ResultadosSe insertaron 2.419 catéteres en arteria radial que permanecieron durante 14.742 días, y 1.085 catéteres en arteria femoral que permanecieron durante 6.497 días. Se detectaron 45 casos de ACR en el sitio femoral y 162 casos en el sitio radial. Hubo una menor tasa de ACR en el sitio femoral que en el radial (4,1% vs 6,7%; p=0,003). La regresión de Poisson mostró una menor incidencia de ACR en el sitio femoral que en el radial (0,69 vs 1,10 eventos de ACR por 100 días de catéter; OR 0,6, p = 0,006, IC95% 0,01-0,83).
ConclusionesEncontramos una menor incidencia de ACR en el sitio femoral que en el radial. Pensamos, que para mejorar la seguridad de los pacientes podría ser interesante monitorizar exhaustivamente la incidencia de ACR e implementar medidas preventivas, debido a que la ACR puede conllevar complicaciones graves.
Critically ill patients frequently are undergoing to arterial catheterization to continuous monitoring of systemic arterial pressure arterial and obtain repetitively blood sampling.1–4 Arterial catheterization involves different risks, such as infection, vascular damage, haemorrhage, thrombosis, or lesion of nerves. Arterial catheter may have an ACR. The importance of ACR lies in that it could cause severe complications, potentially life-threatening, as severe external haemorrhage and vascular damage. However, there are scarce data about accidental removal of arterial catheter.5–9 In addition, we did not find studies comparing the ACR incidence between different arterial catheter sites. Thus, the objective of this study was to compare the incidence of ACR in femoral and radial arterial catheters.
Materials and methodsWe performed a retrospective study over six years of all patients who were undergoing femoral or radial arterial catheters during their stay in the polyvalent ICU of the Hospital Universitario de Canarias, Tenerife, Spain. This is a 24-bed ICU and each box is independent with the possibility to close the door. The study was approved by the institutional review board.
The decision to use the femoral or radial site was taken on the basis of the criterion of the physician responsible for the patient because there was no protocol in the ICU. The catheters used were radiopaque polyurethane catheters (Arrow, Reading, PA). The length of arterial catheters used was of 12cm in femoral and 4.45cm in radial access. Femoral catheters were inserted by Seldinger technique, and radial catheters were inserted over needle. Femoral catheters were fixed by silk suture and radial sites by steri-strip. The catheters were inserted in ICU or surgical room. The percutaneous entry sites were examined daily by the ICU nurse assigned to the patient. Physicians and nurses were advised to be attentive and vigilant in order to reduce this undesirable problem. Sedation was prescribed, when necessary, by physicians.
The following data were collected: age, sex, diabetes mellitus, APACHE-II, diagnosis group, catheter access, catheter insertion and removal dates, and cause of catheter removal (planned or accidental).
We considered ACR as the presence of an unplanned removal produced by the patient or the staff. The ACR can be performed by the patient, either by taking hold of it with their hands or by making voluntary movements that led directly to the removal. The ACR can be performed by the staff as a consequence of inadequate handling. The catheters removed due to obstruction of the catheter were not considered as ACR.
Statistical analyses were performed with SPSS 12.0.1 (SPSS Inc., Chicago, IL), LogXact 4.1 (Cytel Co., Cambridge, MA) and StatXact 5.0.3 (Cytel Co., Cambridge, MA). Continuous variables are reported as medians and percentiles 25th–75th, and were compared using Mann–Whitney test. Categorical variables are reported as frequencies and percentages. We used Kruskal–Wallis test for singly ordered r×c table to compare between femoral and radial groups the proportions of the presence/absence of diabetes, accidental removal. Diagnosis and sex proportions between catheter groups were compared with Chi-square test. The incidence of ACR per 100 catheter-days between groups was compared using Poisson regression. The independent variable was arterial catheter site (femoral vs radial), the dependent variable was ARC and, finally the rate multiplier was time of catheter insertion. The magnitude of the effects is expressed as Odds Ratio (OR) and 95% confidence interval (CI). A p-value less than 0.05 was considered statistically significant.
ResultsWe found 207 events of ACR in 3504 (5.91%) catheters during 21,239 days of catheterization (0.97 events of ACR per 100 days of catheterization). A total of 2419 radial arterial catheters were inserted and remain in situ during 14,742 days. And were inserted 1085 arterial femoral catheters that remain in situ during 6497 days. We detected 45 cases of ACR in femoral site and 162 cases in radial arterial site.
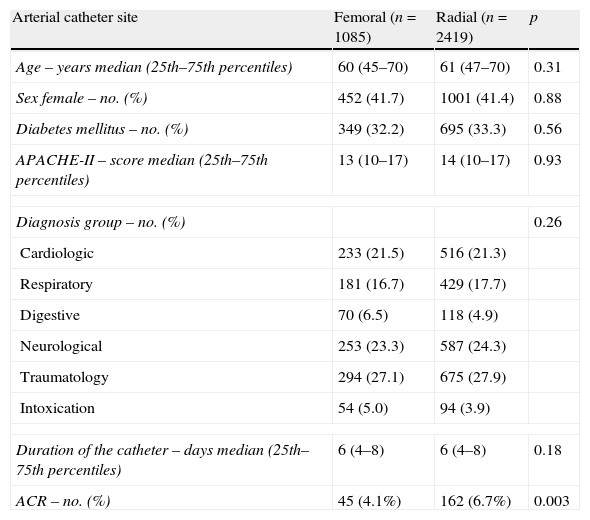
As shown in Table 1, there were no significant differences between both arterial sites in age, sex, diabetes mellitus, APACHE-II, diagnosis group and duration of the catheter. A lower ACR rate was found in femoral than in radial site (4.1% vs 6.7%; p=0.003)
Characteristics of femoral and radial arterial catheters.
| Arterial catheter site | Femoral (n=1085) | Radial (n=2419) | p |
| Age – years median (25th–75th percentiles) | 60 (45–70) | 61 (47–70) | 0.31 |
| Sex female – no. (%) | 452 (41.7) | 1001 (41.4) | 0.88 |
| Diabetes mellitus – no. (%) | 349 (32.2) | 695 (33.3) | 0.56 |
| APACHE-II – score median (25th–75th percentiles) | 13 (10–17) | 14 (10–17) | 0.93 |
| Diagnosis group – no. (%) | 0.26 | ||
| Cardiologic | 233 (21.5) | 516 (21.3) | |
| Respiratory | 181 (16.7) | 429 (17.7) | |
| Digestive | 70 (6.5) | 118 (4.9) | |
| Neurological | 253 (23.3) | 587 (24.3) | |
| Traumatology | 294 (27.1) | 675 (27.9) | |
| Intoxication | 54 (5.0) | 94 (3.9) | |
| Duration of the catheter – days median (25th–75th percentiles) | 6 (4–8) | 6 (4–8) | 0.18 |
| ACR – no. (%) | 45 (4.1%) | 162 (6.7%) | 0.003 |
Poisson regression analysis showed a lower incidence of ACR in femoral than in radial arterial site (0.69 vs 1.10 events of ACR per 100 catheter-days; OR 0.6, p=0.006, 95%CI 0.01-0.83).
DiscussionTo our knowledge, this study includes the largest series reporting data on ACR of artery catheters and it is the first comparing ACR incidence between different arterial catheter sites. The most relevant finding of our study is that femoral arterial catheter showed a lower ACR incidence than radial access.
The number of arterial catheters included in previous studies was slow, and the study of Carrion et al. reported the higher number of catheters (792 catheters).6 In our study we analyzed 3504 arterial catheters. Our ACR rate (5.91% catheters and 0.97 events of ACR/100 days of catheterization) is within the previously reported rates, which is of a range between 3.8 and 18.4% catheters and of 1.17–1.8 events of ACR per 100 days of catheterization.5–9
In most of the previous studies there was no description of the artery access;6–9 although in the study by Amo Priego 187 radial and 46 femoral artery catheters were included.5 In our study we analyzed 2419 radial and 1085 femoral artery catheters. Previously, a comparison of ACR incidence was not reported between different arterial catheter sites, and we report for the first time a lower ACR incidence in femoral than in radial arterial access. In the study by Marcos et al. 64 radial arterial catheters were analyzed and the authors found an ACR rate of 12.5% catheters and 1.8 events of ACR per 100 days of catheterization.7 García et al. published a study with 49 arterial catheters (without description of the artery access) that showed an ACR rate of 18.4% catheters and 1.69 ACR per 100 days of catheterization.8 A study by Goñi Viguria et al. with 101 arterial catheters (without description of the artery access) found an ACR rate of 9.9% of catheters and 1.47 ACR per 100 days of catheterization.9 A total of 792 arterial catheters (without description of the artery access) were analyzed in the study by Carrion et al., and the authors found an ACR incidence of 1.17 per 100 days of catheterization.6 In the study by Amo Priego et al., including 233 arterial catheters (187 radial and 46 femoral catheter), an ACR rate of 3.8% was showed (but did not report the number of events per 100 days of catheterization).5
In a previous study of our team,10 we did not find significant differences in the ACR rate between 1057 radial and 125 femoral arterial sites. Possibly, the increase of sample size to 2419 radial and 1085 femoral arterial catheters has contributed in the appearance of significant differences in our current report.
Our study has some limitations. First, the different insertion vascular sites were observationally compared without randomization. Second, we have not collected data about the sedation level, agitation, mechanical ventilation, nurse/patient relationship and work shift in each arterial catheter site. Third, femoral catheters were fixed by silk suture and radial sites by steri-strip, and this fact could have contributed in the lower incidence of ACR in femoral than in radial site. Fourth, the catheters removed due to obstruction of the catheter were not considered as ACR and this cause was included in the Quality Indicators in critically ill patients published by Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias.11,12 Five, we have not collected data about the complications associated with ACR.
Possibly, the optimal decision to use an arterial site determined should be carried out on the basis of the patient safety in a global manner, i.e. taking into account different risks of arterial catheter such as ACR, nosocomial infection and mechanical complications. With respect to ARC, we found in this study that femoral arterial site has lower risk of ACR than radial site (0.69 vs 1.10 events/100 catheter-days; OR 0.6, p=0.006, 95%CI 0.01-0.83). Regarding nosocomial infection, our team found a higher risk of catheter-related bloodstream infection in femoral arterial site than in radial site (1.92 vs 0.25/1000 catheter-days, OR 1.9 (95% CI 1.15-3.41), p=0.009).13 And with respect to mechanical complications, in one clinical review of complications of arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine, was found a higher temporary occlusion and haematoma rate in radial than in femoral site and a higher permanent ischemic damage rate in femoral than in radial arteries14; although were not reported complety data about all complications in all studies included in the review.
ConclusionWe found a lower incidence of ACR in femoral than in radial site. We think that in order to improve the safety of patients, it could be interesting to monitor exhaustively the ACR incidence, implement preventive measures and to research about ACR prevention since ACR could give rise to severe complications.
Competing interestsThe authors have no conflict of interest to declare.
FundingThis study was supported, in part, by a grant from Instituto de Salud Carlos III (I3SNS-INT-11-063) (Madrid, Spain).
This study was supported, in part, by a grant from Instituto de Salud Carlos III (I3SNS-INT-11-063) (Madrid, Spain).