To construct a model of factors predicting mortality in severe community-acquired pneumonia (SCAP) with data on the first 24h after admission to the intensive care unit (ICU).
DesignA prospective, observational study was carried out.
SettingThe ICU of a university hospital.
PatientsICU-admitted patients with SCAP were studied prospectively.
InterventionsAdmission pneumonia scores were calculated, and clinical variables were registered during the first 24h. Relationships between predictors of mortality at 28 days were assessed by means of a multivariate logistic regression model.
ResultsA total number of 242 SCAP patients were evaluated. The SAPS II severity score was 37.2±15.5 points. Bivariate analysis showed high mortality to be more frequent in elderly patients, as well as in patients with high SAPS II scores, neoplastic disease or chronic renal failure. The other prognostic factors related to increased mortality included mechanical ventilation, acute respiratory distress syndrome (ARDS), acute renal failure, bacteremia, and septic shock. Mortality at 28 days was 23.1% (56 patients). Multivariate analysis of the risk factors generated a new predictive model of mortality applicable within the first 24h after ICU admission and comprising 5 main factors: age, CURB severity score 3–4, septic shock, ARDS, and acute renal failure.
ConclusionsAge in years, CURB score 3–4, septic shock, ARDS, and acute renal failure during the first 24h of ICU admission were found to be independent predictors of mortality in SCAP patients.
Construir un modelo de factores predictivos de mortalidad en la neumonía adquirida en la comunidad grave (NACG) utilizando los datos de las primeras 24h de ingreso en la unidad de cuidados intensivos (UCI).
DiseñoEstudio prospectivo y observacional.
ÁmbitoUCI de un hospital universitario.
PacientesSe estudiaron de forma prospectiva los pacientes ingresados en la UCI con el diagnóstico de NACG.
IntervencionesSe calcularon las escalas de neumonía y se registraron las variables clínicas en las primeras 24h del ingreso en la UCI. Para evaluar los factores predictores de mortalidad a los 28días, se construyó un modelo multivariado de regresión logística.
ResultadosUn total de 242pacientes con NACG fueron analizados. La puntuación de gravedad por el SAPSII fue de 37,2±15,5 puntos. El análisis bivariado mostró una mayor mortalidad en pacientes de edad avanzada, con una puntuación de SAPSII alta, enfermedad neoplásica o insuficiencia renal crónica. Otros factores pronóstico relacionados con el aumento de la mortalidad fueron la ventilación mecánica, el síndrome de distrés respiratorio agudo (SDRA), la insuficiencia renal aguda, y el shock séptico o la bacteriemia. La mortalidad a los 28días fue del 23,1% (56pacientes). El análisis multivariado de los factores de riesgo permitió construir un nuevo modelo predictivo de mortalidad aplicable en las primeras 24h de ingreso en la UCI, que consistió en 5factores: edad, CURB score 3-4, shock séptico, SDRA e insuficiencia renal aguda.
ConclusionesLa edad en años, el CURB score 3-4, el shock séptico, el SDRA y la insuficiencia renal aguda evaluados en las primeras 24h de ingreso en la UCI fueron factores de riesgo independientes de mortalidad en pacientes con NACG.
Severe community-acquired pneumonia (SCAP) remains a serious illness with important clinical impact. In the USA, community-acquired pneumonia is the 7th leading cause of death1 and 0.5–1 million patients per year are hospitalised for treatment. Out of these, 10% require intensive care unit (ICU) admission.2 Despite advances in therapy and ICU measures, mortality rates due to SCAP remain high, between 20% and 50%, depending on studies.3,4 Since potential poor prognosis is known to contribute to increased ICU patient admissions, anticipating complications through the use of supporting measurements becomes essential. Scores of severity such as the pneumonia severity index (PSI), CURB and CURB 655–7 are of limited use in clinical practice to determine hospital admission. Recently, IDSA/ATS guidelines have redefined SCAP and indications for ICU admission, according to major and minor clinical criteria.1,8. Although publications proposing new criteria and scales to define which SCAP patients require ICU admission, patient evolution and prognosis after ICU admission are still broadly distributed, with mortality up to 20–30%.9 Besides, models of mortality should evaluate the behaviour of critical variables during the first 24h of ICU admission of SCAP patients, being aimed at detecting predictive factors and anticipating more intensive treatment, particularly in patients with initial bad prognosis.
In this work, a cohort of ICU-admitted SCAP patients was studied. The main aim was constructing a model of predictive factors of mortality from variables evaluated during the first 24h of ICU admission. Another aim was studying general severity scores for pneumonia, so as to determine patient evolution according to severity of community-acquired pneumonia.
Materials and methodsPatient study subjectsAll SCAP patients hospitalized in our 16-bed ICU were prospectively studied from January 2005 to January 2009 in a 420-bed university and teaching hospital that serves a population of 725,000 inhabitants. According to the SCAP definition by the Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS), the presence of symptoms of lower respiratory tract infection was required, along with a new infiltrate on chest radiography and no other alternative diagnosis during follow-up, in non-hospitalized patients for at least the previous 72h. The patients were included by a study protocol and the final decision on ICU patient admission was made according to clinical judgement by the physician in charge. The institutional review board and the local ethical committee for clinical research approved the study protocol. The written consent of the patient or the patient's legally authorized representative was obtained before inclusion in the study.
Data collectionThe data collected for each patient were divided into three groups: (1) demographic and clinical data prior to admission; (2) clinical data at the time of admission; and (3) clinical data obtained during the clinical process. The following data were recorded upon admission: age, gender, smoking and alcohol habits, co-morbid illness, antimicrobial treatment prior to hospital admission, clinical symptoms and clinical presentation (body temperature, confusion, respiratory rate, heart rate, arterial systolic pressure, saturation O2, pleural effusion), analytical data (haemoglobin, BUN, glucose, sodium, leukocytes, arterial pH and PaO2/FiO2). During the clinical process the following variables were collected: results of microbial investigations, presence of septic shock, need for mechanical ventilation and non-invasive ventilation, days of mechanical ventilation, renal failure development, radiographic progression – increased involvement in the chest radiography with an additional lung lobe respect to emergency department admission – emphysema, bacteraemia, shock, acute respiratory distress syndrome (ARDS), empiric antibiotic treatment and length of ICU stay. Mortality was evaluated at 28 days.
Co-morbidities were defined as follows: cardiac illness: congestive heart failure with ventricular dysfunction documented by clinical, radiology and echocardiography or presence of valve heart disease or previous coronary artery disease; pulmonary: treatment for asthma or chronic obstructive pulmonary disease (COPD); central nervous system disorders: acute or chronic vascular or nonvascular encephalopathy; diabetes mellitus: diagnosis of intolerance to glucose and treatment with oral antidiabetics or insulin; hepatic: pre-existing viral or toxic hepatopathy or liver cirrhosis; renal: pre-existing renal disease with documented abnormal serum creatinine level outside the period of the pneumonia episode; neoplasic illness: any solid tumour; immunosupression: for severe immunosupression such as manifested by neutropenia (<1.0×109cells/l), or from human immunodeficiency virus (HIV) infection with counting of CD4<350cell/mm3, solid-organ or bone-marrow transplantation, or steroid treatment within the previous 30 days. Alcohol abuse was defined as the ingestion of ≥40g in males and >24g in females per day for at least one year before presentation. Smokers were defined as current smokers of ≥10 cigarettes/day during at least the preceding year.
Score calculationsAdmission pneumonia scores were calculated with data of 24h of ICU admission (PSI-Pneumonia Severity Index-, CURB and CURB-65), according to the original publications,5–7 but not used to admit or not the patient in ICU. High-risk patients were defined as those with PSI risk class IV–V, a CURB risk class 3–4 or CURB-65 risk class 3–5 upon admission.
All patients were classified into IDSA/ATS criteria, according to the 2007 IDSA/ATS guidelines,1 and SCAP was defined as the presence of two major criteria (receipt of invasive mechanical ventilation and septic shock with the need for vasopressors), or presence of three minor criteria (respiratory rate≥30breaths/min, PaO2/FiO2≤250mmHg, multilobar infiltrates, confusion and/or disorientation), uraemia (BUN level≥20mg/dl), leukopenia (WBC count<4×109cells/l), thrombocytopenia (platelet count<100×109platelets/l), hypothermia (core temperature≤36°C), hypotension (SBP≤90mmHg; requiring aggressive fluid resuscitation).
Septic shock was defined as sepsis induced hypotension persisting despite adequate fluid replacement. Sepsis induced tissue hypoperfusion is defined as septic shock, an elevated lactate or oliguria.10,11
ARDS was defined as acute onset of bilateral radiographic infiltrates, PaO2/FiO2≤250mmHg, pulmonary artery wedge pressure<18mmHg if this information is available or lack of clinical evidence of left ventricular failure.12
Acute renal failure (ARF) was defined using de RIFLE criteria as tripling of basal creatinine or creatinine≥4mg/dl with an increase of 0.5mg/dl, 75% reduction in glomerular filtration rate, urine output≤0.3ml/kg/h for 24h, or anuria for 12h.13
As a comparative baseline of severity, SAPS II (Simplified Acute Physiology Score) was also calculated.14
Microbiological evaluationIn non-intubated patients, the routine sampling for microbiological examination consisted of a sputum, two blood cultures, and a sample of urine for culture and for the determination of Legionella sp. and Streptococcus pneumoniae urinary antigen assays, and pleural fluid culture in case of large pleural effusions. All intubated patients with mechanically ventilation, underwent at least one tracheobronchial aspirate (TBA) or protected bronchoalveolar mini-lavage (mini-BAL).15 Patients with any level of immunosupression or/and bilateral pulmonary infiltrates underwent bronchoscopic sampling techniques (protected specimen brush [PSB] or bronchoalveolar lavage [BAL]). During the period of study, urine, TBA, and blood were processed for polymerase chain reaction (PCR) analysis of Legionella pneumophila.
Sputum was stained for Gram and only cultured with the presence of more than 25 granulocytes and less than 10 epithelial cells. PSB and BAL fluid samples were cultured for aerobic and anaerobic bacteria pathogens, mycobacteria and fungi. Negative bacterial cultures were discarded after 7 days. Micro-organism identification was completed according to standard microbiological methods. Results of quantitative cultures were expressed as colony-forming units per millilitre (cfu/ml), according to published standards.16
Pneumonia aetiology was considered definite whenever one of the following criteria was met: (1) blood cultures yielding a bacterial pathogen; (2) pleural fluid cultures yielding a bacterial pathogen; (3) a positive urinary antigen for Legionella or S. pneumoniae; (4) bacterial growth in cultures of TBA≥105cfu/ml, in PSB≥103cfu/ml, and in mini-BAL and BAL≥104cfu/ml; or (5) specific PCR amplification of L. pneumophila.
Statistical analysisDescriptive statistics of demographic and clinical variables included means and standard deviations for quantitative variables, and percentages for qualitative variables. For unadjusted comparisons between or among groups, continuous variables were compared by using Student's t test, if data are normally distributed, or Mann–Whitney U test for non-normally distributed data. Categorical variables were compared by using the chi-square test or Fisher's exact test where appropriate. Analysis of risk factors for mortality at 28 days was performed initially by using a bivariate analysis, whereas a multivariate analysis was performed by logistic regression. A multiple logistic regression model was used to assess the relationships between predictors of mortality and death at 28 day by all causes. Our primary predictors of interest are the general severity score (SAPS II), scores of pneumonia (PSI, CURB and CURB 65) upon admission, and other predictors such as septic shock, ARDS, and acute renal failure within the first 24h of ICU admission.
The list of other candidate predictors was narrowed to include those with a bivariate significance at p<0.2 level, as well as clinically significant variables. A forward selection model, using an entry criterion of p≤0.05, was carried out to limit co-linearity problems. Because the number of deaths was limited (N=56), the model was constrained to a total number of 5–6 degrees of freedom. No confounding was found, so this term was not included in the final model. Model discrimination and predictive power were assessed by the area under the receiver operator characteristic curve (AUC-ROC). Possible over-fitting was evaluated with the Hosmer–Lemeshow goodness-of-fit test. Data are presented as odds ratios (OR) with 95% confidence intervals (CI). p value<0.05 was considered statistically significant for all comparisons. Statistical analyses were performed using SPSS (version 12; SPSS®, Inc., Chicago, IL).
ResultsBaseline featuresDuring the period from 2005 to 2009, 242 SCAP patients were prospectively collected. One hundred and sixty-seven patients (69%) were male, and 75 (31%) female, while average age was 56.8±16. Considering co-morbidity, 99 patients (40.9%) had previous COPD diagnosis, 49 patients (20.2%) had congestive heart failure, and 43 patients (17.8%) had diabetes mellitus. Only 12 patients (5%) had chronic renal disease. Upon ICU admission, patient severity by SAPS II was 37.2±15.5 points.
During the first 24h, 150 patients (62%) showed some level of respiratory failure that required ventilation support, and 141 patients (58.3%) displayed involvement of multiple lobes and radiographic progression. Average ICU stay was 11.0±11.8 days, and 28-day mortality rate was 23.1%. Demographic data, risk factors, co-morbidities, clinical data and outcome are shown in Table 1.
Characteristics of the study population.a
| Characteristics | All (N=242) |
| Demographics | |
| Age, years | 56.8 (16.0) |
| SAPS II on admission, points | 37.2 (15.5) |
| Gender, male | 167 (69.0) |
| Alcohol abuse | 74 (30.6) |
| Smokers | 140 (57.9) |
| Co-morbid illnesses | |
| COPD | 99 (40.9) |
| Neoplasic disease | 15 (6.2) |
| Liver disease | 31 (12.8) |
| Congestive heart failure | 49 (20.2) |
| Cerebral stroke | 11 (4.5) |
| Chronic Renal disease | 12 (5.0) |
| Diabetes mellitus | 43 (17.8) |
| Immunosuppression | 36 (14.9) |
| HIV infection | 10 (4.1) |
| Clinical data | |
| Septic shock | 89 (36.8) |
| Acute respiratory distress syndrome | 54 (22.3) |
| Acute renal failure | 81 (33.5) |
| Acute neurological failure | 85 (35.1) |
| Bacteraemia | 48 (19.8) |
| Empyema | 23 (9.5) |
| Radiographic progression | 141 (58.3) |
| Mechanical ventilation | 150 (62.0) |
| Outcome | |
| Days of mechanical ventilation | 8 (10.3) |
| Length of ICU stay, days | 11.0 (11.8) |
| Length of hospital stay, days | 18.7 (17.1) |
| ICU mortality | 57 (23.6) |
| Mortality at 28 days | 56 (23.1) |
| Hospital mortality | 67 (27.7) |
Microbiological aetiology could be determined in 173 out of 242 (71.5%) patients. The most frequent pathogen was S. pneumoniae (33.5% of all patients). The second and third most common pathogens were L. pneumophila and Haemophilus influenzae. Pseudomonas aeruginosa was isolated in 8 patients (3.3%). No difference in microbiological aetiology was found between survivor and non-survivor patients. See Table 2.
Aetiology of severe community-acquired pneumonia in all patients.a
| Microbiological aetiology | All patients (N=242) | Non-survivors (N=56) | Survivors (N=186) | p value |
| Streptococcus pneumoniae | 81 (33.5) | 20 (35.7) | 61 (32.8) | 0.69 |
| Legionella pneumophila | 39 (16.1) | 7 (12.5) | 32 (17.2) | 0.40 |
| Haemophilus influenzae | 10 (4.1) | 1 (1.8) | 9 (4.8) | 0.69 |
| Staphylococcus aureus | 6 (2.5) | 2 (3.6) | 4 (2.2) | 0.55 |
| Pseudomonas aeruginosa | 8 (3.3) | 2 (3.6) | 6 (3.2) | 0.90 |
| Escherichia coli | 8 (3.3) | 4 (7.1) | 4 (2.2) | 0.55 |
| Klebsiella pneumoniae | 4 (1.7) | 2 (3.6) | 2 (1.1) | 0.20 |
| Other microorganisms | 18 (7.4) | 4 (7.1) | 14 (7.5) | 0.92 |
| Unknown aetiology | 69 (28.5) | 15 (26.8) | 51 (27.4) | 0.74 |
Demographics and comorbidities associated with death at 28 days are shown in Table 3. Non-survivor patients were older than survivors (64.7±13.4 vs. 54.7±16.1; p=0.0001). In addition, neoplasic disease, immunosupression, chronic renal disease, invasive mechanical ventilation, ADRS, acute renal failure, bacteraemia and septic shock were risk factors of mortality at 28 days. On the other hand, the support treatment with non-invasive ventilation was associated with better survival (Table 4).
Demographics and comorbidities in non-survivors vs. survivors patients.a
| Variables | Non-survivors at 28d (N=56) | Survivors at 28d (N=186) | Odds ratio or mean difference (95%CI)b | p value |
| Demographics | ||||
| Age, years | 64.7±13.4 | 54.7±16.1 | 8.9 (4.7–13.2) | 0.000 |
| Male | 42 (75.0) | 125 (67.2) | 1.5 (0.7–2.8) | 0.270 |
| Alcohol habit | 17 (30.4) | 57 (30.6) | 0.98 (0.5–1.8) | 0.967 |
| Smokers | 27 (48.2) | 113 (60.8) | 0.6 (0.3–1.1) | 0.096 |
| Comorbidities | ||||
| COPD | 26 (46.4) | 73 (39.2) | 1.3 (0.7–2.4) | 0.339 |
| Neoplasic disease | 8 (14.3) | 7 (3.8) | 4.3 (1.5–12.3) | 0.004 |
| Liver disease | 11 (19.6) | 20 (10.8) | 2.0 (0.9–4.5) | 0.082 |
| Congestive heart failure | 16 (28.6) | 33 (17.7) | 1.8 (0.9–3.7) | 0.078 |
| Cerebral stroke | 5 (8.9) | 6 (3.2) | 2.9 (0.9–10.0) | 0.073 |
| Chronic renal disease | 7 (12.5) | 5 (2.7) | 5.2 (1.6–17.0) | 0.003 |
| Diabetes mellitus | 10 (17.9) | 33 (17.7) | 1.0 (0.5–2.2) | 0.984 |
| Immunosuppression | 14 (25.0) | 22 (11.8) | 2.5 (1.2–5.3) | 0.015 |
| HIV infection | 3 (5.4) | 7 (3.8) | 1.4 (0.3–5.8) | 0.599 |
Risk factors in non-survivors vs. survivors patients.a
| Variables | Non-survivors at 28d (N=56) | Survivors at 28d (N=186) | Odds ratio | p value |
| Septic shock | 42 (75.0) | 47 (25.3) | 8.9 (4.5–17.7) | <0.001 |
| Acute renal failure | 38 (67.9) | 43 (23.1) | 7.0 (3.6–13.5) | <0.001 |
| Bacteraemia | 17 (30.4) | 28 (15.1) | 2.5 (1.2–4.9) | 0.010 |
| Empyema | 8 (14.3) | 15 (8.1) | 1.9 (0.8–4.7) | 0.165 |
| Rx progression | 35 (62.5) | 106 (57.0) | 1.3 (0.7–2.3) | 0.464 |
| Mechanical ventilation | 53 (94.6) | 100 (53.8) | 15.2 (4.6–50.4) | <0.001 |
| Non-invasive ventilation | 8 (16.0) | 50 (34.2) | 0.4 (0.2–0.8) | 0.015 |
| ARDS | 28 (50.0) | 26 (14.0) | 6.1 (3.2–12.0) | <0.001 |
After applying severity scores (SAPS II, PSI, CURB and CURB 65) to our population, both SAPS II and higher PSI were associated with significantly higher mortality. Most survivor patients were classified into CURB 1–2 and CURB 65 1–3 groups (Table 5).
SAPS II and pneumonia severity scores on hospital admission.a
| Characteristics | Non-survivors at 28d (N=56) | Survivors at 28d (N=186) | Odds ratio or mean difference (95%CI)b | p value |
| SAPS II | ||||
| SAPS II, points | 50.3±15.7 | 33.2±13.0 | 17.0 (12.9–21.2) | <0.001 |
| PSI | ||||
| PSI, total points | 153.7±38.7 | 113.8±38.8 | 39.9 (28.2–51.5) | <0.001 |
| PSI risk classes I, II and III | 6 (10.7) | 51 (27.4) | ||
| PSI risk classes IV and V | 50 (89.3) | 135 (72.6) | 3.1 (1.3–7.8) | 0.01 |
| CURB | ||||
| CURB scores 1 and 2 | 24 (42.9) | 144 (77.4) | ||
| CURB scores 3 and 4 | 32 (57.1) | 42 (22.6) | 4.6 (2.4–8.6) | <0.001 |
| CURB 65 | ||||
| CURB 65 scores 1 and 2 | 18 (32.1) | 123 (66.1) | ||
| CURB 65 scores 3, 4 and 5 | 38 (67.9) | 63 (33.9) | 4.1 (2.1–7.8) | <0.001 |
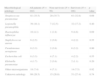
A predictive model of mortality applicable during the first 24h of ICU admission was built. This model shows that age in years (OR: 1.04; 95%CI: 1.02–1.06), CURB score 2 and 3 (OR: 3.36; 95%CI: 1.58–7.15), septic shock (OR: 4.03; 95%CI: 1.74–9.74), ARDS (OR: 2.89; 95%CI: 1.25–6.69), and acute renal failure (OR: 2.41; 95%CI: 1.07–5.38) were independent predictive factors of mortality at 28 days in SCAP patients (Table 6).
Model of logistic regression analysis of risk factors for mortality at 28 days.
| Variables | Odds ratio | 95%CI | p value |
| Age, years | 1.039 | 1.012–1.068 | 0.005 |
| CURB score 3–4 | 3.358 | 1.578–7.147 | 0.002 |
| Septic shock | 4.036 | 1.744–9.341 | 0.001 |
| Acute respiratory distress syndrome | 2.892 | 1.250–6.691 | 0.013 |
| Acute renal failure | 2.409 | 1.078–5.380 | 0.032 |
| Hosmer–Lemesow test | 0.380 | ||
| AUC-ROC | 0.863 | 0.808–0.917 | 0.001 |
Community-acquired pneumonia is still one of the most prevalent illnesses, its mortality having changed in the last 30 years.1 To decrease mortality, early and adequate antibiotic treatments were recommended,17 patients were treated according to international guidelines,18 and scores of severity were used to classify poorly prognoses and ICU-demanding patients.19 In spite of these tools, delays in ICU admission and initial inappropriate treatment contributing to disastrous consequences for patients still persist.
In this study, early prognostic factors of mortality were detected in SCAP patients, concluding, by means of a robust regression logistic model that age in years, CURB 2–3, septic shock, ARDS, and acute renal failure are independent prognostic factors. Although, most patients who are admitted to ICU are correctly diagnosed and treated with the initial basic measures (oxygen therapy and antibiotic treatment), ICU mortality holds 20–30%.9 Therefore, as intensive care professionals, we must think carefully what factors can be changed to reduce mortality in our patients.
In our work, mortality risk factors were studied during the first 24h of ICU admission for early detection and identification of these factors. In bivariate analysis, elderly patients with a high SAPS II score, or neoplasic illness, or chronic renal insufficiency, or presence of immunosupression in the acute phase of SCAP showed the highest mortality risk. These results agree with those reported elsewhere.20,21 Other factors such as the presence of septic shock, bacteraemia, acute renal failure, ARDS, and requirement for mechanical ventilation are factors associated with greatest mortality in our cohort analysis.
Furthermore, in our study the use of the non-invasive ventilation (NIV) resulted in lower mortality, although in daily clinical practice this technique is indicated for specific patients.22–25 In this work we did not study this topic but, probably the successful use of NIV enables keeping patients under-sedated, thus avoiding the critically ill myopathia and the development of ventilator-associated pneumonia, both of which contribute to increased mortality. Nevertheless, delay in intubation may worsen prognosis and increase mortality.26
A strength of the study is the high percentage of microbiological confirmation in community acquired pneumonia. The SCAP aetiology was elucidated in a higher percentage of our patients, possibly due to the use of PCR for the detection of L. pneumophila. Another factor that may contribute to this high percentage of agent identification could be that microbiological samples were taken for all patients early on admission to the ICU. We followed a strict protocol for collecting respiratory specimens as described in ‘Materials and methods’ section. However, the main etiologic micro-organism was S. pneumoniae, similarly to other previous studies.27 Concerning aetiology, no differences were observed in micro-organisms between survivors and non-survivors patients.
As most clinicians use prognostic mortality scores to stratify severity and ICU requirement, there is a growing number of scores intended to reduce delay in ICU admission and patient mortality such as for example, the new criteria of ATS/IDSA, PIRO, SMART-TOP or SCAP score.8,28–31 In all these studies, mechanical ventilation and shock (major criteria of ATS/IDSA) are indicators of immediate ICU admission. However, doubts appear in the presence of minor, less specific criteria that entail delayed admission or confusion. Since evolution of pneumonia is a dynamic process, recent studies indicate the need of repeating scores 48h after clinical treatment onset, as this allows higher sensitivity and specificity.31 Similar clinical management is proposed in our local protocol in ICU-admitted SCAP patients. However, we believe like Karmakar et al.32 that the decision making in respect of severe CAP is the same whether or not a pneumonia severity score is applied. Probably, routine use of the score will identify patients with mild CAP thus potentially reducing unnecessary hospital admission.
Through multivariate study, the variables that prognoses mortality best within 24h after ICU admission were determined. Age in years, CURB score, septic shock, ARDS, and acute renal failure were independent mortality factors. In the same way, Rodriguez et al.33 showed that bacterial community-acquired pneumonia with shock, acute renal failure, and over-24-point APACHE II score were independently associated with mortality. A recent study by Sabatier et al.34 observed that invasive mechanical ventilation, ADRS, acute renal failure, and sepsis or septic shock are associated with higher mortality in bivariate analysis, but only invasive mechanical ventilation, acute renal failure, non-identifiable aetiology, and non-S. pneumoniae aetiology were independent risk factors of mortality in SCAP. In our study, CURB may clearly interact in the statistical model with septic shock, ADRS, and acute renal failure, but would be used quickly in first instance in the emergency department as a parameter to identify patients needing intensive care admission. However, if CURB score is used further during the first 24h of ICU admission together with an evaluation of haemodynamic, respiratory and renal functions, it enables predicting mortality in these patients. This early assessment allows the intensivist to start appropriate antibiotic treatment and use fast support techniques,33 like, for example, early renal replacement therapy,13 or protective ventilation.12 SCAP clearly seems to involve all those risk factors that contribute to complications of pulmonary infection and systemic sepsis effects, as well as to determine both clinical outcome and mortality, as reported by Gilavert Cuevas and Bodí Saera in an excellent review.35
Our conclusions are hereby presented, yet they have some limitations: (1) this is a large observational study on an SCAP patients cohort treated in one only centre. Therefore, a second study is needed to validate our multivariate model within the first 24h of ICU admission; (2) the causes behind delayed transfer to ICU – which might have led to misinterpretation of the first 24-h evaluation – were not assessed; (3) it is unknown if there was delay in the introduction of antibiotic therapy and if this therapy was started empirically in emergency department prior to ICU admission. Because it has been shown in other studies36 that the time of ICU admission have a significant influence on mortality; (4) although a strict protocol and robust statistical analysis were followed in the present study, results come from our hospital and, therefore, our model may need external validation; and (5) these concerns are valid risk factors for SCAP caused by bacteria, but not for SCAP caused by the virus such as influenza A/H1N1 that has a different clinical profile.37
ConclusionsIn this prospective study, age in years, CURB 3–4 score, septic shock, acute respiratory distress syndrome, and acute renal failure during the first 24h of ICU admission, were independent predictive factors of mortality in SCAP patients. No factors described are probably amenable to medical intervention, but may help to identify, upon admission, subjects at higher risk.
Conflict of interestWe declare that we have no conflict of interest to disclose.