A new pediatric acute respiratory distress syndrome (PARDS)1 definition has been recently released by the Pediatric Acute Lung Injury Consensus Conference (PALICC). This definition (Table 1) has some characteristics which makes it different to the adult ARDS definition. There are also a number of points we are not sure about in terms of diagnosis and treatment.
PALICC definition of ARDS.
| Age | Exclude patients with peri-natal related lung disease | |||
| Timing | Within 7 days of known clinical insult | |||
| Origin of Edema | Respiratory failure not fully explained by cardiac failure or fluid overload | |||
| Chest Imaging | Chest imaging findings of new infiltrate(s) consistent with acute pulmonary parenchymal disease | |||
| Oxygenation | Non invasive mechanical ventilation | Invasive mechanical ventilation | ||
| PARDS (No severity stratification) | MIld | Moderate | severe | |
| Full face-mask bi-level ventilation or CPAP≥5cm H2Ob PF ratio≤300 SF ratio≤264a | 4≤OI<8 5≤OSI<7.5a | 8≤OI<16 7.5≤OSI<12.3a | OI>16 OSI>12.3a | |
| Special populations | ||||
| Cyanotic heart disease | Standard criteria above for age, timing, origin edema and chest imaging with an acute deterioration in oxygenation not explained by underlying cardiac disease.c | |||
| Chronic lung disease | Standard criteria above for age, timing and origin edema with chest imaging consistent with new infiltrate and acute deterioration in oxygenation from baseline which meet oxygenation criteria above.c | |||
| Left ventricular dysfuction | Standard criteria for age, timing and origin edema with chest imaging changes consistent with new infiltrate and acute deterioration in oxygenation which meet criteria above not explained by left ventricular dysfunction. | |||
OI=oxygenation index=(FiO2*mean airway pressure*100)/PaO2.
OSI=oxygen saturation index=(FiO2*mean airway pressure*100)/SatO2.
CPAP: Continuous positive airway pressure; PaO2: Arterial oxygen pressure; SpO2: Transcutaneous oxygen saturation; FiO2: Fraction of inspired oxygen; SF: spO2/FiO2; PF: PaO2/FiO2; ARDS: Acute respiratory difficulty syndrome; PARDS: Pediatric acute respiratory difficulty syndrome; OI: oxygenation index; OSI: oxygen saturation index.
Use PaO2 based metric available. If PaO2 not available, wean FiO2 to maintain SpO2≤97% to calculate OSI or SF ratio.
For non-intubated patients treated with supplemental oxygen or nasal modes of non-invasive ventilation see Table 2 for At Risk Criteria.
In 1967, Ashbaugh et al. 2 discovered a never-before described pathology. “The clinical pattern […] includes severe dyspnea, tachypnoea, cyanosis that is refractory to oxygen therapy, loss of lung compliance, and a diffuse alveolar infiltrate seen on chest X-ray”. Chest X-ray appearances consisted of “patchy, bilateral alveolar infiltrates”. “At necropsy […], gross inspection showed heavy and deep reddish-purple lungs… (whose) appearance resembled liver tissue”. Microscopic appearances were consistent with current descriptions. The histopathological hallmark of the ARDS was established by Katzenstein et al. in 1976, and named Diffuse Alveolar Damage (DAD).3
ARDS was first defined in Barcelona in 1994 by the American European Consensus Conference (AECC).4 In 2012, in Berlin, a new ARDS definition was proposed, for adult patients, which also has been validated in children,5 as an improvement to the Barcelona definition, focusing on feasibility, reliability, validity, and objective evaluation of its performance.
Using the Barcelona AECC definition, and comparing with autopsy findings of DAD, we have been able to accurately confirm the diagnosis of ARDS in both adults6 (likelihood ratio (LR) for a positive in adults=4.7) and children7 (LR for a positive in children=5.65). With the new Berlin definition, we have gained in sensitivity (98%; 95%CI=94–99) to detect DAD8: LR for a negative 0.1 (95%CI=0.0–0.2). This is practically a SnOUT: if a patient does not completely fulfill each criteria as defined by the Berlin definition of ARDS (i.e. if you have a unilateral infiltrate in the X-ray) then DAD is not clearly established.
Forty years after the first description of ARDS, the best knowledge is: a NON-ARDS patient with a hypoxemic respiratory failure is accurately and confidently defined (the way to rule out this clinical condition is well known). However the new proposed PARDS definition,1 removed the requirement of bilateral infiltrates in the chest imaging, which in our opinion means the best tool to diagnose PARDS has been lost. In order to maintain the sensitivity obtained with the previous definition, we think it is important to reconsider preserving in the PARDS definition bilateral opacities as a condition, as seen in the adult definition. Moreover, it should be necessary to focus the attention on improving the new definition's specificity. For example, measuring the intracardiac shunt through the patent foramen ovale in those patients worsening with greater PEEP values, or assessing the role of pulmonary hypoxemic vasoconstriction in hypoxemia pathophysiology.
Therefore one of the most contentious points in the new classification of PARDS is the need for unilateral or bilateral infiltrates. The authors themselves consider that this consensus is only a proposal that must be validated.9 Therefore until the definition is not validated, it is important to remember that all the scientific information available (based on therapeutic strategies and prognosis) has been generated assuming the disease is bilateral. Future studies should demonstrate whether ARDS should include unilateral conditions.
Another aspect that deserves consideration and discussion relates to the use of oxygenation index (OI) in the estimation of the severity of the patients.
To understand our argument we must consider some epistemological considerations.
Post hoc ergo propter hoc (Latin: “after this, therefore because of this”) is a logical fallacy (of the questionable cause variety) that states “Since event Y followed event X, event Y must have been caused by event X”. It is often shortened to simply post hoc fallacy. The following is a simple example: The rooster crows immediately before sunrise, therefore the rooster causes the sun to rise. Post hoc is a particularly tempting error because temporal sequence appears to be integral to causality. The fallacy lies in coming to a conclusion based exclusively on the order of events, rather than taking into account other factors that might rule out the connection. Let us give you another example: “A high Oxygenation Index (OI) is associated with high mortality in pediatric acute respiratory distress syndrome (PARDS), therefore high OI causes death in PARDS”.
Deciding that “OI, in preference to PaO2/FiO2 (P/F) ratio, should be the primary metric of lung disease severity to define PARDS for all patients treated with invasive mechanical ventilation” could be a post hoc fallacy, because a crucial factor such as the ventilatory strategy used in the treatment of the patient has not been taken into account.10 This statement (“OI in preference to P/F ratio”) is true if and only if open lung approach (OLA) is employed, but not otherwise. It can be seen clearly with two illustrative cases with four PARDS patients in their second day of Pressure Control Ventilation mode (Table 2).
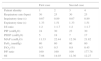
Illustrative cases of children with ARDS showing different clinical situations (see text).
| First case | Second case | |||
|---|---|---|---|---|
| Patient identity | 1 | 2 | 3 | 4 |
| Respiratory rate (bpm) | 30 | 25 | 30 | 25 |
| Inspiratory time (s) | 0.67 | 0.89 | 0.67 | 0.89 |
| Expiratory time (s) | 1.33 | 1.51 | 1.33 | 1.51 |
| I:E ratio | 1:2 | 1:1.7 | 1:2 | 1:1.7 |
| PIP (cmH2O) | 24 | 30 | 23 | 30 |
| PEEP (cmH2O) | 5 | 18 | 7 | 17 |
| MAP (cmH2O) | 11.33 | 22.44 | 12.36 | 21.82 |
| PaO2 (mmHg) | 80 | 80 | 80 | 80 |
| FiO2 (%) | 0.5 | 0.5 | 0.8 | 0.45 |
| P/F ratio | 160 | 160 | 100 | 177.78 |
| OI | 7.08 | 14.03 | 12.36 | 12.27 |
Bpm: breath per minute, s: second(s); I:E ratio: inspiratory/expiratory ratio; PIP: peak inspiratory pressure; PEEP: positive end expiratory pressure; PaO2: arterial oxygen pressure; FiO2: fraction of inspired oxygen; PF: PaO2/FiO2; MAP: mean airway pressure; OI: oxygenation index.
In the first case, patients 1 and 2 have the same P/F ratio: 160. In children,11 this P/F ratio corresponds to 11–26% mortality. They show different OI values, probably because their different inferior inflexion point in their compliance curves had lead their attending physicians (who are performing OLA guided by the P/F ratio) to use different continuous distending pressures. Same prognosis but different OIs.
On the contrary, in the second case patients 3 and 4 show the same OI. But patient 3 (whose doctors are not using OLA) has a P/F ratio: 100, which means an 18–59% mortality. Patient 4, however, is being ventilated following OLA, and the P/F ratio is 177, which relates to an expected mortality of only 11–26%. Same OI but with completely different prognosis.
It is also important to note that OI is a mathematical transformation of the P/F ratio. They are not independent variables. Therefore, entering both simultaneously in a logistic regression model would violate the independence assumption that gives internal validity to a General Linear Model. It is possible due to this statistical flaw that the sole opportunity we have to analyze which of both variables has the real weight of information, is to modelize PARDS mortality, treating OI as an interaction term, suggesting a multiplicative relationship between MAP and the inverse of P/F ratio. Only if OI reaches statistical significance, must it stay in the model but always accompanied by the other two components of the product. Otherwise, you can choose the parsimonious model (explanation or prediction with as few predictor variables as possible) with P/F ratio alone. You can never be without P/F ratio!
Agreeing with Occam's razor, and in order not to commit post hoc fallacy, we propose to maintain P/F ratio to define PARDS, a physiopathological measurement of the intrapulmonary shunt,1 totally independent to the respiratory treatment the patient (appropriately or not) is receiving. From our point of view it is very dangerous that someone could think that it is not appropriate to increase the PEEP level in order to recruit the lung only because with this maneuver the OI will increase. The OI could have an important role in the control of the evolution of the patient if and only if the patient is being treated with the open lung approach.
In summary: don’t remove that brick from the wall (bilateral infiltrates) and keep it smart and simple (P/F ratio).
Conflict of interestThe authors declare no conflict of interest.