In this study, we aimed to evaluate the death risk factors of patients included in the sepsis protocol bundle, using clinical data from qSOFA, SIRS, and comorbidities, as well as development of a mortality risk score.
DesignThis retrospective cohort study was conducted between 2016 and 2021.
SettingTwo university hospitals in Brazil.
ParticipantsPatients with sepsis.
InterventionsSeveral clinical and laboratory data were collected focused on SIRS, qSOFA, and comorbidities.
Main variable of interestIn-hospital mortality was the primary outcome variable. A mortality risk score was developed after logistic regression analysis.
ResultsA total of 1,808 patients were included with a death rate of 36%. Ten variables remained independent factors related to death in multivariate analysis: temperature ≥38 °C (odds ratio [OR] = 0.65), previous sepsis (OR = 1.42), qSOFA ≥ 2 (OR = 1.43), leukocytes >12,000 or <4,000 cells/mm3 (OR = 1.61), encephalic vascular accident (OR = 1.88), age >60 years (OR = 1.93), cancer (OR = 2.2), length of hospital stay before sepsis >7 days (OR = 2.22,), dialysis (OR = 2.51), and cirrhosis (OR = 3.97). Considering the equation of the binary regression logistic analysis, the score presented an area under curve of 0.668, is not a potential model for death prediction.
ConclusionsSeveral risk factors are independently associated with mortality, allowing the development of a prediction score based on qSOFA, SIRS, and comorbidities data, however, the performance of this score is low.
En este estudio, nuestro objetivo fue evaluar los factores de riesgo de muerte de los pacientes incluidos en el protocolo de sepsis, utilizando datos clínicos de qSOFA, SIRS y comorbilidades, así como el desarrollo de un puntaje de riesgo de mortalidad.
DiseñoEste estudio de cohorte retrospectivo se llevó a cabo entre 2016 y 2021.
ÁmbitoDos hospitales universitarios en Brasil.
ParticipantesPacientes con sepsis.
IntervencionesSe recopilaron varios datos clínicos y de laboratorio centrados en SIRS, qSOFA y comorbilidades.
Variable de interésprincipalesLa mortalidad intrahospitalaria fue la variable de resultado primaria. Se desarrolló un puntaje de riesgo de mortalidad después del análisis de regresión logística.
ResultadosSe incluyeron un total de 1,808 pacientes con una tasa de mortalidad del 36%. Diez variables permanecieron como factores independientes relacionados con la muerte en el análisis multivariado: temperatura ≥38 °C (odds ratio [OR] = 0.65), sepsis previa (OR = 1.42), qSOFA≥2 (OR = 1.43), leucocitos >12,000 o <4,000 células/mm3 (OR = 1.61), accidente cerebrovascular encefálico (OR = 1.88), edad >60 años (OR = 1.93), cáncer (OR = 2.2), duración de la estancia hospitalaria antes de la sepsis >7 días (OR = 2.22), diálisis (OR = 2.51) y cirrosis (OR = 3.97). Considerando la ecuación del análisis de regresión logística binaria, el puntaje presentó un área bajo la curva de 0.668, un modelo débil para la predicción de la muerte.
ConclusionesVarios factores de riesgo se asocian de forma independiente con la mortalidad, lo que permite el desarrollo de una puntuación de predicción basada en datos de qSOFA, SIRS y comorbilidades; sin embargo, el rendimiento de esta puntuación es bajo.
Sepsis is associated with high in-hospital mortality, hospital cost, and morbidity.1 According to the consensus published in 1991, sepsis is defined as the presence of suspected infection in addition to systemic inflammatory response syndrome (SIRS).2 The definitions of sepsis, septic shock, and organic dysfunction have remained unchanged for more than 2 decades. Thus, the last definition of sepsis was changed to life-threatening organ dysfunction caused by a dysregulated host response to infection.3
The sequential organ failure assessment (SOFA) score has high predictive validity.4 However, the SOFA score is not a practical tool in the emergency room or ward because it requires laboratory tests. Considering the high mortality associated with sepsis and that prompt intervention is necessary, a new practical measure is needed to help healthcare professionals recognize sepsis. The quick SOFA (qSOFA) comprised the following criteria: altered mental status, systolic blood pressure of 100 mmHg or less, and respiratory rate of 22/min or greater,5 and the presence of two of these criteria were correlated with mortality. Although SIRS criteria are positive in almost 90% of patients with infection and organ dysfunction, neither qSOFA nor SIRS scores have been used as unique screening options, while medical evaluation and criticism should also be considered.6,7
Both scores have been used for screening of sepsis, but the evaluation of these scores in the prediction of mortality can be useful because approach to patients with higher mortality risk can be differentiated. Even though several scores have been well established, an individualized prognostic model on the basis of the nomogram could accurately predict mortality and optimize management or tailored therapy.8 The SIRS, qSOFA, and pSOFA (pediatric) have been used in previous studies as a predictive model of mortality in pediatric population, pregnant and adult hematological patients.9–12 These predictive models can be used for alert systems, improving the approach of patient care.13
We hypothesized that these scores and comorbidities can be used to predict mortality. In this study, we aimed to develop of a mortality risk score based on qSOFA, SIRS, and comorbidities.
MethodsStudy designThis was a retrospective cohort study of patients included in the sepsis protocol in two Brazilian university hospitals. This study was approved with a waiver of informed consent by the institutional review board of the Pontifícia Universidade Católica do Paraná (CAAE number: 79976517.4.0000.0020).
SettingsThis study was conducted on adult patients with suspected sepsis. The cohort included patients admitted at two academic public hospitals between January 2016 and December 2021. The first hospital was composed of an emergency room, a 207-bed hospital ward, and a 29-bed mixed intensive care unit (ICU), but reference for trauma, neurosurgery, and general surgery. The second hospital was also composed of an emergency room, 240-bed hospital wards, and a 38-bed ICU, reference for general surgery and cardiovascular surgery.
Both hospitals present the same antimicrobial stewardship team.
Sepsis protocolThe antibiotic therapy decisions were based on local microbial resistance profiles.14 The antibiotic stewardship program (ASP) implemented a restrictive policy for dispensing carbapenems and polymyxin using a hand-filled form.15 In addition, a prospective auditing and feedback process was adopted for all antimicrobial prescriptions. Dose, length of treatment adjustment, de-escalation, route of administration, and side effects were determined under the guidance of a clinical pharmacist and infectious diseases specialist.16
Once sepsis was suspected and judged that antimicrobial therapy was needed in the first hour, the physician fulfilled the protocol. However, only those with Sepsis-3 criteria were included,3 which was defined within 24 hours by the antimicrobial stewardship. The patients were followed up until death or discharge. The hour-1 bundle includes: i) measuring lactate level and remeasuring lactate if initial lactate is elevated (> 2 mmol/L); ii) obtaining blood cultures before administering antibiotics; iii) administration of broad-spectrum antibiotics; iv) rapid administration of 30 mL/kg crystalloid for hypotension or lactate ≥ 4 mmol/L; v) application of vasopressors if the patient was hypotensive during or after fluid resuscitation to maintain a mean arterial pressure ≥65 mmHg.7 The sepsis bundle is shown in Supplementary Figure 1 (Fig. 1).
ParticipantsInclusion criteria were (i) a hospital admission, (ii) ≥18 years of age, and (iii) a starting sepsis protocol, (iv) sepsis diagnosis according to Sepsis-3 criteria.3 The only exclusion criterion was a lack of information in the patient’s sepsis protocol file to avoid selection bias. Follow-up was performed using electronic medical records. Patients with more than one episode of sepsis were included as a “new” event. The population of the study included ICU, ward, and emergency room.
VariablesThe SIRS (2 points) and qSOFA (2 points), as well as other clinical data were considered at the moment of protocol. The SIRS criteria (i.e., temperature > 38 °C, heart rate >90/min, respiratory rate >20/min, and leukocytes >12,000 or <4,000 cell/mm3)17 and qSOFA score (i.e., systolic blood pressure <100 mmHg, respiratory rate >22 rpm, and Glasgow coma scale <15) were used.18 Comorbidities were analyzed according to the Charlson comorbidity index.19 Hospital-acquired infection were defined according with the Centers for Disease Control and Prevention were included.20 Community-acquired infection was defined based on the physician’s classification, using the International Classification of Diseases, Tenth Revision (ICD-10), and diagnosis codes.21
The primary outcome was global mortality. The timing of antibiotic treatment relative to clinical diagnosis was evaluated. The cultures were evaluated, and appropriate antimicrobial therapy was provided to patients with sepsis. The length of hospital stay was also assessed. Outcomes were compared according to SIRS criteria and qSOFA scores, hospital unit (ICU, ward, or emergency room [ER]), and positive cultures.
Statistical analysisThe continuous variables were expressed was mean or median according with normality test (Kolmogorov–Smirnov test). The descriptive variables were expressed as percentages. The dispersion of variables were standard deviation or 95% confidence interval.
In the bivariate analysis, P-values were calculated using the χ2 or Fisher’s exact test for categorical variables and the Student’s t-test or Mann–Whitney test for continuous variables. The covariates were compared based on the criteria for sepsis and outcomes. Covariates were compared between survivors versus non-survivors. In the forward stepwise regression, variables with P-values ≤ 0.2 were included in the model, while those with P-values ≤ 0.10 were maintained in the model. Multicollinearity was calculated with the variance inflation factor for each independent variable. Variables which included other variables (e.g., SIRS and qSOFA) were not included in the model. All tests were two-tailed. A P significance was set at P < 0.05. A receiver operating characteristic (ROC) curve was constructed based on independent variables associated with mortality and the logistic binary regression model. The score was based on coefficient (beta) of each variable in the multivariable analysis. The area under the curve (AUC) was calculated to determine the internal performance of the score based on multivariable analysis.
ResultsGeneral dataA total of 2,232 were screened and 205 were excluded due to lack of data, and 219 patients do not fulfill sepsis-3 criteria. Thus, 1,808 were included in the study. The mean age was 60 years (interquartile range [IQR]: 42–72), and 38% of the patients were men. The SIRS criteria (≥2) and qSOFA (≥2) accounted for 63% (n = 1,278) and 29% (n = 593), respectively. The main sites of infection were the lungs (42% [n = 657]) and abdomen (15% [n = 236]). The median length of hospital stay after sepsis was 10 days (IQR: 4–22), while death occurred in 36.8% of patients (n = 666). The mortality in patients admitted at ICU was 47.7%, at emergency room 26.2%, and those with diagnosis of sepsis in the ward was 26.8%. The main comorbidities were systemic arterial hypertension (SAH) (42% [n = 782]), diabetes mellitus (DM) (16% [n = 303]), previous stroke (14.7% [n = 274]), and cancer (8.3% [n = 155]). Among the patients with microbiological data, 45% (n = 626) presented with positive culture results. Blood cultures were obtained from all patients and other cultures, according to the medical decision.
Variables associated with mortalityThe data from patients who died or survived are described in the Table 1. The mortality, the outcome variable, was higher in ICU admitted patients (p < 0.001), but similar between emergency room and ward. Twenty variables were found to be related to death after univariate analysis. Major variables were age (64 vs. 52 years, P < 0.001), length of hospital stay before sepsis (10 vs. 5.4 days, P < 0.001), temperature >38 °C (26% vs. 39%, P < 0.001), leukocytes >12,000 or <4,000 cells/mm3 (49% vs. 38%, P = 0.001), qSOFA criteria >2 (35% vs. 25%, P < 0.001), altered level of consciousness (30% vs. 21%, P < 0.001), low blood pressure (i.e., systolic blood pressure [SBP] <90 mmHg) (31% vs. 21%, P < 0.001), minutes to antimicrobial infusion (45 min vs. 35 min, P < 0.001), heart failure (9.5% vs. 4.8%, P < 0.0001), previous stroke (20% vs. 11%, P < 0.0001), SAH (47% vs. 38%, P < 0.001), cancer (13% vs. 5.5%, P < 0.001), previous sepsis (35% vs. 18%, P < 0.0001), and positive culture (50% vs. 39%, P < 0.0001).
Univariate analysis of the outcome of 1,808 patients included in a sepsis protocol bundle in two Brazilian hospitals.
| Variables | Death(n = 666) | Survival(n = 1142) | P-value |
|---|---|---|---|
| Male sex, n (%) | 276 (41) | 410 (36) | 0.017 |
| Age, mean (SD) | 64 (16) | 52 (19) | <0.001 |
| Length of hospital stay before sepsis, median (IQR) | 10 (14) | 5.4 (10) | <0.001 |
| SIRS criteria ≥2, n (%) | 422 (63) | 711 (62) | 0.640 |
| Temperature >38.3 °C, n (%) | 177 (26) | 454 (39) | <0.001 |
| Cardiac frequency >90 bpm, n (%) | 352 (53) | 592 (52) | 0.685 |
| Respiratory frequency >22 rpm, (n%) | 314 (47) | 455 (40) | 0.09 |
| Leukocytes >12,000 or <4,000 cell/mm3, n (%) | 309 (49) | 442 (38) | 0.001 |
| qSOFA criteria ≥1, n (%) | 319 (47) | 461 (40) | 0.002 |
| qSOFA criteria ≥2, n (%) | 239 (35) | 286 (25) | <0.001 |
| Glasgow Coma Scale <15, n (%) | 201 (30) | 242 (21) | <0.001 |
| Low mean blood pressure (<60 mmHg), n (%) | 207 (31) | 247 (21) | <0.001 |
| Time to antimicrobial infusion, minutes, median (IQR) | 45 (20–90) | 35 (15–79) | <0.001 |
| Previous ICU admission, n (%) | 116 (17) | 138 (12) | 0.002 |
| Previous hospital admission, n (%) | 176 (26) | 267 (23) | 0.154 |
| HIV, n (%) | 13 (1.9) | 20 (1.7) | 0.764 |
| DM, n (%) | 114 (17) | 170 (15) | 0.216 |
| Dialysis, n (%) | 50 (7.6) | 50 (4.4) | 0.006 |
| Heart stroke, n (%) | 36 (5.4) | 46 (4) | 0.178 |
| Heart failure, n (%) | 62 (9.5) | 54 (4.8) | <0.0001 |
| Peripheral arterial disease, n (%) | 69 (10) | 73 (6.5) | 0.003 |
| EVA, n (%) | 137 (20) | 128 (11) | <0.0001 |
| Hemiplegia, n (%) | 17 (2.5) | 24 (2.1) | 0.540 |
| Dementia, n (%) | 20 (3) | 29 (2.5) | 0.564 |
| COPD, n (%) | 61 (9.1) | 87 (7.7) | 0.996 |
| SAH, n (%) | 314 (47) | 437 (38) | <0.001 |
| Cancer, n (%) | 85 (13) | 62 (5.5) | <0.001 |
| Cirrhosis, n (%) | 12 (1.8) | 8 (0.7) | 0.037 |
| Steroids chronic use, n (%) | 45 (6.8) | 58 (5.1) | 0.142 |
| Trauma, n (%) | 182 (27) | 313 (27) | - |
| Elective surgery, n (%) | 107 (16) | 203 (18) | 0.365 |
| Emergency surgery, n (%) | 227 (34) | 343 (30) | 0.082 |
| Previous sepsis, n (%) | 203 (35) | 210 (18) | <0.0001 |
| Palliative care patient, n (%) | 20 (3.2) | 5 (0.4) | <0.0001 |
| Positive culture, n (%) | 277 (50) | 312 (39) | <0.0001 |
| Antimicrobial adequacy | 174/278 (62) | 202/312(65) | 0.324 |
| Setting ICU | 352 (52.8) | 385 (33.7) | <0.0001 |
| Ward | 40 (6) | 109 (9.5) | * |
| Emergency room | 210 (31.5) | 591 (51.7) | * |
SD: standard deviation; IQR: interquartile range; SIRS: systemic inflammatory response syndrome; qSOFA: quick Sequential Organ Failure Assessment; ICU: intensive care unit; HIV: human immunodeficiency virus; DM: diabetes mellitus; EVA: encephalic vascular accident; COPD: chronic obstructive pulmonary disease; SAH: systemic arterial hypertension. * comparison with ICU setting.
Despite these 20 variables, after multivariate analysis, half of them remained independent variables related to death (Table 2). Characteristics such as (i) cirrhosis, (ii) dialysis, and (iii) cancer at least doubled the risk of death: (i) (odds ratio [OR] = 3.97, 95% confidence interval [CI] 1.41–11.16, P = 0.009), (ii) (OR = 2.51, 95% CI 1.54–4.10, P < 0.0001), and (iii) (OR = 2.2, 95% CI 1.49–3.24, P < 0.0001). Other variables were also related to poor prognosis increasing between 42–93% the odds of death: previous sepsis (OR = 1.42, 95% CI 1.08–1.87, P = 0.012), qSOFA criteria ≥2 (OR = 1.43, 95% CI 1.12–1.84, P = 0.04), leukocytes >12,000 or <4,000 cells/mm3 (OR = 1.61, 95% CI 1.27–2.03, P < 0.0001), and previous stroke (OR = 1.88, 95% CI 1.39–2.55, P < 0.0001). A temperature >38 °C was related to survival (OR = 0.65, 95% CI 0.51–0.83, P = 0.0001].
Multivariable analysis of risk factors of mortality in 1,808 patients included in a sepsis protocol bundle in two Brazilian hospitals and mortality score based on beta coefficient.
| Coefficient (beta) | Error | Wald | OR | 95% CI | P | |
|---|---|---|---|---|---|---|
| Chronic renal failure under dialysis | 2.186 | 0.24 | 10.616 | 2.51 | 1.54–4.10 | <0.0001 |
| Cerebrovascular disease | 2.51 | 0.155 | 35.245 | 1.88 | 1.39–2.55 | <0.0001 |
| Cancer | 2.629 | 0.195 | 24.546 | 2.20 | 1.49–3.24 | <0.0001 |
| Cirrhosis | 2.992 | 0.507 | 4.676 | 3.97 | 1.41–11.16 | 0.009 |
| Previous sepsis | 1.842 | 0.13 | 22.225 | 1.42 | 1.08–1.87 | 0.012 |
| Fever (temperature >38.3 °C) | 2.04 | 0.123 | 33.396 | 0.65 | 0.51–0.83 | <0.001 |
| Leukocytosis or leukopenia | 1.387 | 0.114 | 8.202 | 1.61 | 1.27–2.03 | <0.0001 |
| Constant | −1.587 | 0.14 | 128.952 |
OR: odds ratio; CI: confidence interval; qSOFA: quick Sequential Organ Failure Assessment; EVA: encephalic vascular accident. Mortality score = 2.186 × (Chronic renal failure) + 2.51 × (Cerebrovascular disease) + 2.629 × (neoplasm) + 2.992 × (cirrhosis) + 1.842 × (2nd sepsis) + 2.040 × (fever) + 1.387 × (leukocytosis).
Considering the equation of the binary regression logistic analysis, the weight of each significant variable was calculated using the following equation: mortality score = 2.186 × (chronic renal failure) + 2.51 × (cerebrovascular disease) + 2.629 × (cancer) + 2.992 × (cirrhosis) + 1.842 × (previous sepsis) + 2.040 × (fever) + 1.387 × (leukocytosis or leukopenia). The mortality risk according to the scores is presented in Table 3.
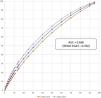
When applying the score, a ROC curve was constructed, as shown in Fig. 2, considering the sensitivity and specificity of the mortality prediction score. The AUC was 0.668 (95% CI 0.623–0.702), suggesting that the mortality score based on the multivariable analysis was weak. We also performed a ROC curve for SIRS and qSOFA, with AUC = 0.522 (95% CI 0.481–0.563) and 0.583 (95% CI 0.535–0.631), respectively (Supplementary material).
DiscussionSince the introduction of the qSOFA, several publications have validated this score in different institutions and used it to assess specific infection sites. The qSOFA has been used to assess patients with pyelonephritis,22 community-acquired pneumonia,23 healthcare-associated pneumonia,24 and burn.25 Additionally, a subgroup analysis revealed that qSOFA is superior to CURB-65 in predicting the prognosis of ICU admission.23 Nevertheless, the last surviving sepsis campaign stated that qSOFA criteria should not be used alone for sepsis screening, while medical judgment must be considered.7 Indeed, according to our cohort results, the positivity of the qSOFA and SIRS criteria was lower than expected (29% and 63%, respectively). Therefore, medical judgment started our sepsis protocol in 71% and 37% of patients without the qSOFA or SIRS criteria, respectively. Despite the use of medical judgment as a possible starting point for the overdiagnosis of sepsis, the global mortality rate was 37%. This is in accordance with the World Health Organization’s global estimation of sepsis-treated death rates. For instance, 27% of in-hospital mortality is related to all treated sepsis, and 42% of in-hospital mortality is specifically related to sepsis diagnosed in the ICU.26 As expected, differences according to world regions may exist, and convergent with our results, the general treated-sepsis death rates vary from 25–36%. Even though SIRS and qSOFA are screening tool for sepsis, these scores can also be used for prediction of death in patients with diagnosis of sepsis.27
In our multivariate analysis, the SIRS criteria were not related to poor prognosis, whereas qSOFA ≥ 2 was an independent variable related to death. This reinforces the qSOFA criteria as a prognostic tool rather than a screening pathway. Therefore, the use of these criteria must be well allocated on a daily basis to decrease the causality of sepsis-related death, considering a lower diagnosis if only qSOFA is used. In six studies, the sensitivity and specificity of qSOFA for mortality varied from 68% to 90% and from 27.4% to 79.5%, respectively.28 In the same studies, the sensitivity of the SIRS criteria was higher (93.0–97.4%), but the specificity was very low (2–27.5%). Although these scores lacked sensitivity or specificity (according to the number of points), combining other markers, such as lactate29,30 and red blood cell distribution,31 can be a good strategy.23,32–39 However, a tool that fits it will probably not become real, given the difference between screening and prognosis steps.40
In our cohort, the absence of fever was an independent factor associated with poor prognosis. This can be explained by the following two points: immunosuppression at the onset of sepsis,41 and the absence of fever may falsely give a “not so bad” impression to the medical team regarding the patient’s status, leading to a softened re-evaluation pathway. Additionally, previous studies have converged with these hypotheses and found that 30-day mortality is higher in patients with afebrile bacteremia.42
Sepsis can be present without qSOFA criteria owing to the different forms of organ dysfunction and qSOFA criteria without infection, such as heart failure. Some studies have suggested that SIRS criteria should not be used.43 However, the approach to patients is not based on specific clinical or laboratory criteria. These criteria are important for didactic reasoning and diagnostic classification in clinical studies. However, some studies still confuse definitions with action strategies.40,44,45
Interestingly, SIRS and qSOFA have been studied in many publications as a score risk of mortality, but generally limited to specific populations, such as S. aureus infections, pre-hospital care, emphysematous pyelonephritis, among others.27,46–49 Liu et al. evaluated qSOFA as a risk of mortality with a AUC ROC of 0.54, similar with our results.50 Another large retrospective cohort showed that SOFA was better than qSOFA and SIRS, with AUC ROC of 0.58 and 0.60 respectively.51 These data confirm the results of our study.
Other studies evaluated in different hospitals, but not in Brazilian hospitals, and also without the description of analysis with implementation of bundles, where intervention measures tend to be standardized and lower mortality.52,53 Despite this, our score reached values very close to studies in the literature. We even performed a ROC curve analysis for qSOFA and SIRS with our patients (supplementary material), but the AUC was extremely unfavorable.
Despite the inclusion of >2,000 patients in this study, there were several limitations. First, this was a retrospective study, which could have led to misinterpretation after the extraction of data from medical records. This novel score should be validated in another cohort of patients to determine an external validation. In the model, patients from different settings were included, and if we categorize this groups, the strength of the model would decrease.
ConclusionIn conclusion, the SIRS and qSOFA scores are not independent scores for death. The the association of clinical and laboratorial data from these scores together with comorbidities resulted in a better score but not a robust predictor of death. Fever was related to a better prognosis, while cirrhosis, dialysis, prolonged length of stay, and cancer had at least double the odds of death. Therefore, medical teams must be aware of these variables as prognosis in patients with sepsis.
Author's contributionVinicius Nakad Orsatti – idealization, draft text
Victoria Stadler Tasca Ribeiro – text review
Carolina de Oliveira Montenegro – data manager
Clarice Juski Costa – data manager
Eduardo Albanske Raboni – draft text, data manager
Eduardo Ramos Sampaio – draft text, data manager
Fernando Michielin – final review
Juliano Gasparetto – idealization, statistical analysis
João Paulo Telles – statistical analysis, final text
Felipe Francisco Tuon – idealization, statistical analysis, final text
Financial disclosures: None.
Conflicts of interestNone.
None.