To compare the quality of chest compressions performed according to the classical technique (MT) vs. a new technique (NM) (compression with 2 thumbs with closed fists) in an infant manikin.
DesignA controlled, randomized cross-over study was carried out in professionals assisting pediatric patients.
SettingA University Hospital with a Pediatric ICU in the north of Spain.
ParticipantsResidents and nurses in Pediatrics who had completed a basic and an advanced pediatric cardiopulmonary resuscitation course.
InterventionsQuantitative analysis of the variables referred to chest compression quality in a 2-min cardiopulmonary resuscitation scenario in infants. Laerdal's SimPad® with SkillReporter™ system was used.
Main variables of interestMean rate and percentage of compressions in the recommended rate range, mean depth and percentage of compressions within the depth range of recommendations, percentage of compressions with adequate decompression, and percentage of compressions performed with the fingers in the center of the chest.
ResultsGlobal quality of the compressions (NM: 84.2±23.7% vs. MT: 80.1±25.4% [P=.25; P=ns]), percentage of compressions with correct depth (NM: 59.9±35.8% vs. MT: 59.5±35.7% [P=.76; P=ns]), mean depth reached (NM: 37.3±3.8mm vs. MT: 36±5.3mm [P=.06; P=ns]), percentage of complete re-expansion of the chest (NM: 94.4±9.3% vs. MT: 92.4±18.3% [P=.58; P=ns]), and percentage of compressions with the recommended rate (NM: 62.2±34.6% vs. MT: 51±37.2% [P=.13; P=ns]) proved similar with both methods.
ConclusionsThe quality of chest compressions with the new method (thumbs with closed fists) is similar to that afforded by the traditional method.
Comparar en un maniquí de lactante la calidad de las compresiones torácicas según el método tradicional (MT) o según la nueva técnica de 2 pulgares con puños cerrados (NM).
DiseñoEstudio controlado, aleatorizado y cruzado en profesionales.
ÁmbitoHospital Universitario con UCI Pediátrica del norte de España.
ParticipantesResidentes y enfermeros de Pediatría, habiendo superado un curso de RCP básica y avanzada pediátrica.
IntervencionesAnálisis cuantitativo de calidad de compresiones torácicas en escenario de RCP en lactante durante 2min, mediante el sistema SimPad® con SkillReporter™ de Laerdal.
Variables de interés principalesFrecuencia media y porcentaje de compresiones en rango recomendada, profundidad media y porcentaje de compresiones en rango recomendado, porcentaje de compresiones con descompresión adecuada y porcentaje de compresiones realizadas con los dedos en el centro del tórax.
ResultadosLa calidad global de las compresiones (NM: 84,2±23,7% vs. MT: 80,1±25,4% [p=0,25; no sig.]), el porcentaje de compresiones con profundidad correcta (NM: 59,9±35,8% vs. MT: 59,5±35,7% [p=0,76; no sig.]), la profundidad media alcanzada (NM: 37,3±3,8mm vs. MT: 36±5,3mm [p=0,06; no sig.]), el porcentaje de reexpansión completa de la caja torácica (NM: 94,4±9,3% vs. MT: 92,4±18,3% [p=0,58; no sig.]) y el porcentaje de compresiones con la frecuencia recomendada (NM: 62,2±34,6% vs. MT: 51±37,2% [p=0,13; no sig.]) fueron similares con los 2 métodos.
ConclusionesLa calidad de compresiones torácicas con el nuevo método (pulgares con los puños cerrados) es similar a la obtenida con el método tradicional.
Pediatric cardiorespiratory arrest (CRA) is a rare event that requires immediate quality action for short-term recovery and survival free from unwanted neurological side effects in the victim.1–6
However, we have seen that in practice, the quality of ventilations and chest compressions is usually poor even when cardiopulmonary resuscitation (CPR) maneuvers are performed by healthcare providers highly experienced in pediatric care.7
There are several reasons behind this, among these the scare frequency of CRA in children, the lack of training and re-training by healthcare providers, the lack of quality surveillance systems to monitor the CPR maneuvers or even the use of the most appropriate CPR maneuvers.8–11 Basically, and same as it happens with adults, there is no doubt that quality chest compressions impact the results which is why choosing a technique that provides the best organic perfusion possible during the CPR should be the primary goal here.
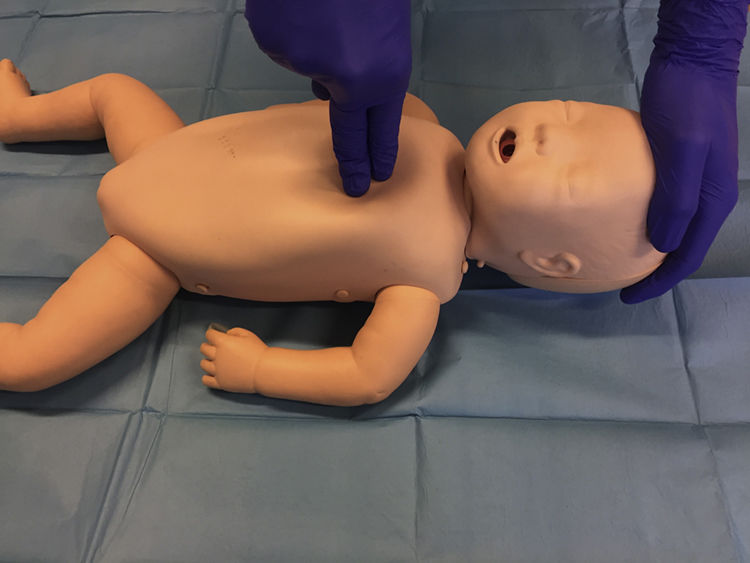
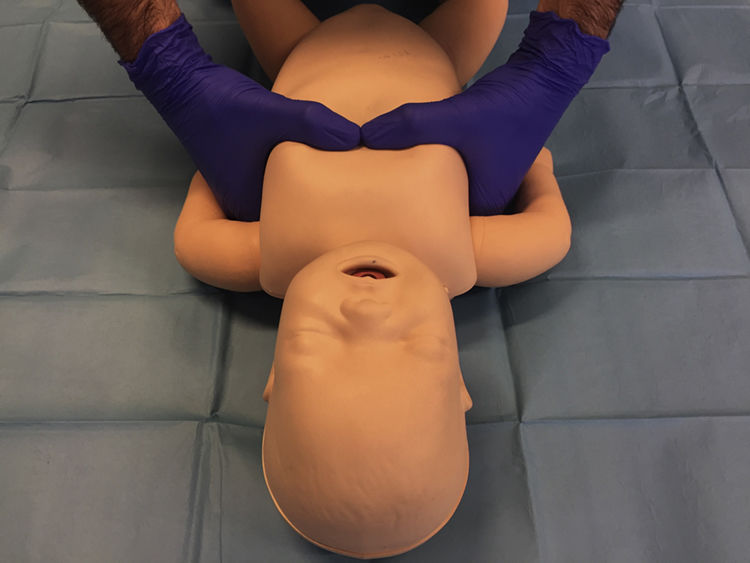
It is odd to see that, even though pediatric CPR has been updated based on the available actual evidence over the last 20 years, chest compression techniques in infants have not changed that much, whether because new evidence has come to light or because it was never been seen as a priority research in the first place.12–14 Thus, the actual international clinical practice guidelines recommend to use the so-called ‘two-finger technique’ in both new-born babies and infants (Fig. 1) if only one resuscitator is present, and the ‘hugging’ technique with both hands (Fig. 2) when two resuscitators are present.15 Over the last few years, several studies have shown that the ‘hugging’ technique may be more effective than the ‘two-finger technique’.16–19
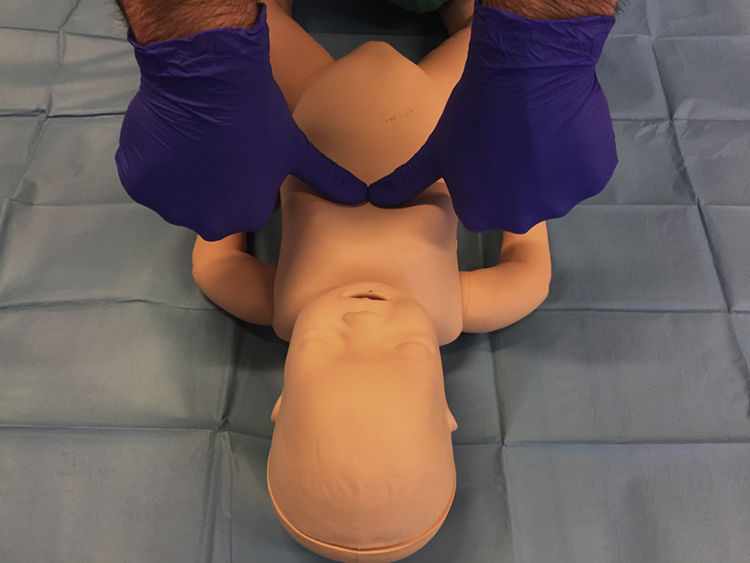
Recently, Smereka et al.20 described a new technique for cardiac massage in infants that consists of using both thumbs in a 90° angle with respect to the infant's chest while closing the remaining fingers of both hands making a fist (Fig. 3). Such a technique allows exerting more force with less finger wear and tear, which in turn helps maintaining the quality of chest compressions in time.
Since the early results have been obtained by paramedics and possibly they cannot be generalized to the CPR maneuvers performed by healthcare providers, we decided to conduct this study in order to draw a quality comparison of the results obtained using the new technique and the traditional method when used by pediatric healthcare providers in a sham procedure using an infant manikin. Our hypothesis was that the new method was non-inferior compared to the recommended one.
Patients and methodsTwenty-eight (28) healthcare providers from a university hospital in northern Spain were included in this study. They had done a course on pediatric CPR and had been evaluated quantitatively using Laerdal QPCR-meter. Participation was voluntary and they did not receive any monetary compensation for their collaboration in the study.
Study designThis was an observational, randomized, crossover study with infant manikins (SimBaby™, Laerdal Medical, Stavanger, Norway, that simulates a 3-month old infant) conducted between January and May 2017.
All participants knew how to perform the ‘hugging’ technique with both hands, the so-called Traditional Method (TM), as recommended by the actual clinical practice guidelines for the management of pediatric CPR.15 Before doing this test, the so-called New Method (NM)20 was briefly explained to them and they were allowed to practice it for about 5min so they could become familiar with it.
Prior to starting the test, the order in which one method or the other would be performed was randomized: 12 participants started performing the NM (43%) and the remaining 16 participants (57%) the TM.
Each participant performed two tests of pediatric CPR with a 15:2 compression/ventilation ratio for 2min with a 30min rest between one and the other. Chest compressions were performed using two different techniques in a randomized sequence:
- a)
Hugging technique with both hands (TM) (Fig. 2): in this technique both fingers are placed on the lower half of the sternum with the remaining fingers somehow hugging the rib cage while resting on the infant's back.
- b)
New technique of using both thumbs with the fists closed (NM) (Fig. 3): it consists of using both thumbs in a 90° angle with respect to the chest while the remaining fingers of both hands stay closed making two fists.
The participants did the cardiac massage only; the ventilations were performed by researchers in order to avoid any biases and using a self-inflating bag and a mask that was the size of the manikin.
Data miningData on chest compression were recorded with a SimBaby™ manikin using the SimPad® system with SkillReporter™ (Laerdal Medical, Stavanger, Norway). For every CPR sequence, the following variables were recorded: frequency of compressions, percentage of compressions with the recommended frequency, percentage of adequate depth compressions, percentage of sufficient re-expansion compressions, compressions with a right position of the fingers, and overall quality (a parameter that weighs in on every component of chest compressions). Also, the participants were asked for their opinion on which of the two methods was the easiest to use and which was the least exhausting of the two in order to evaluate the average difficulty perceived using a subjective score between 1 (lowest difficulty) and 10 (greatest difficulty).
Once the test was over, all participants filled out a questionnaire for demographic information purposes.
Statistical analysisAll statistical analyses were conducted using the Epidat v.4.2 software package (Consellería de Sanidade, Xunta de Galicia, Spain; Pan American Health Organization (PAHO-WHO); CES University, Colombia). Results are expressed as mean and standard deviation. The paired t test was used for the continuous variables in order to compare both methods. In all analyses, P values <.05 were considered significant.
ResultsOf the 28 healthcare providers included in this study, 16 were women and 12 were men; 13 were nurses, 9 were doctors, and 6 were paramedics. Their average age was 29.5±6.5 years, their average height was 169±10.7cm, and their average weight was 69.7±12.5kg.
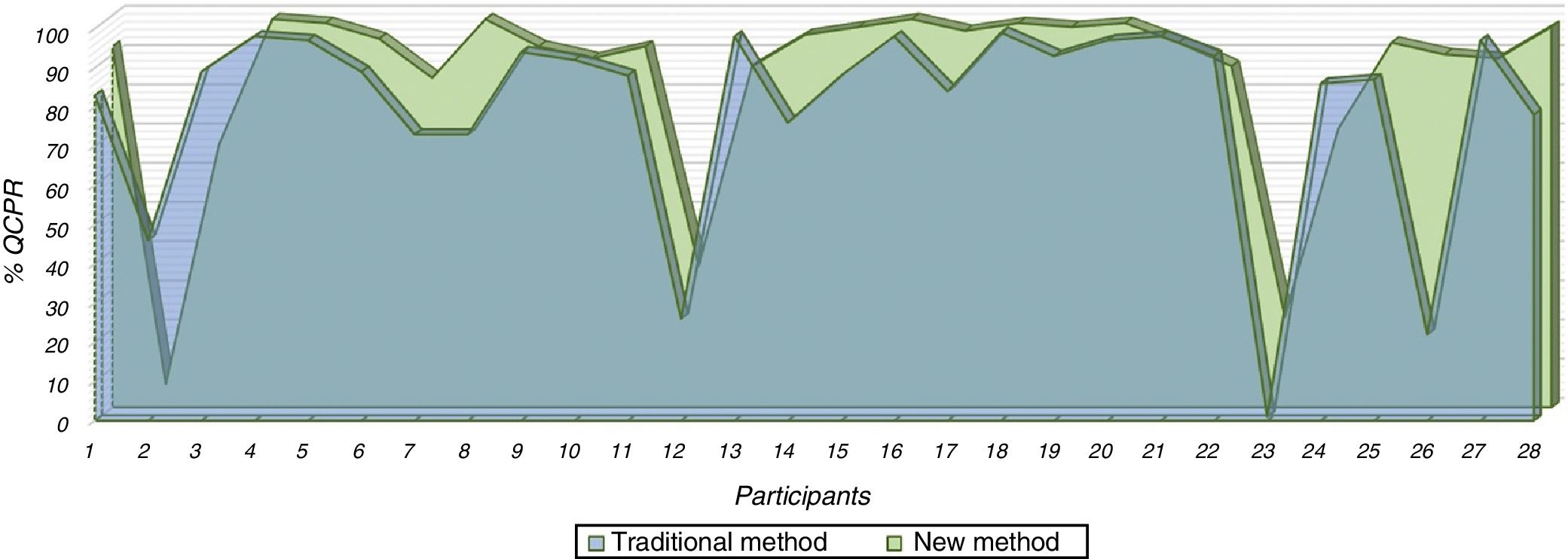
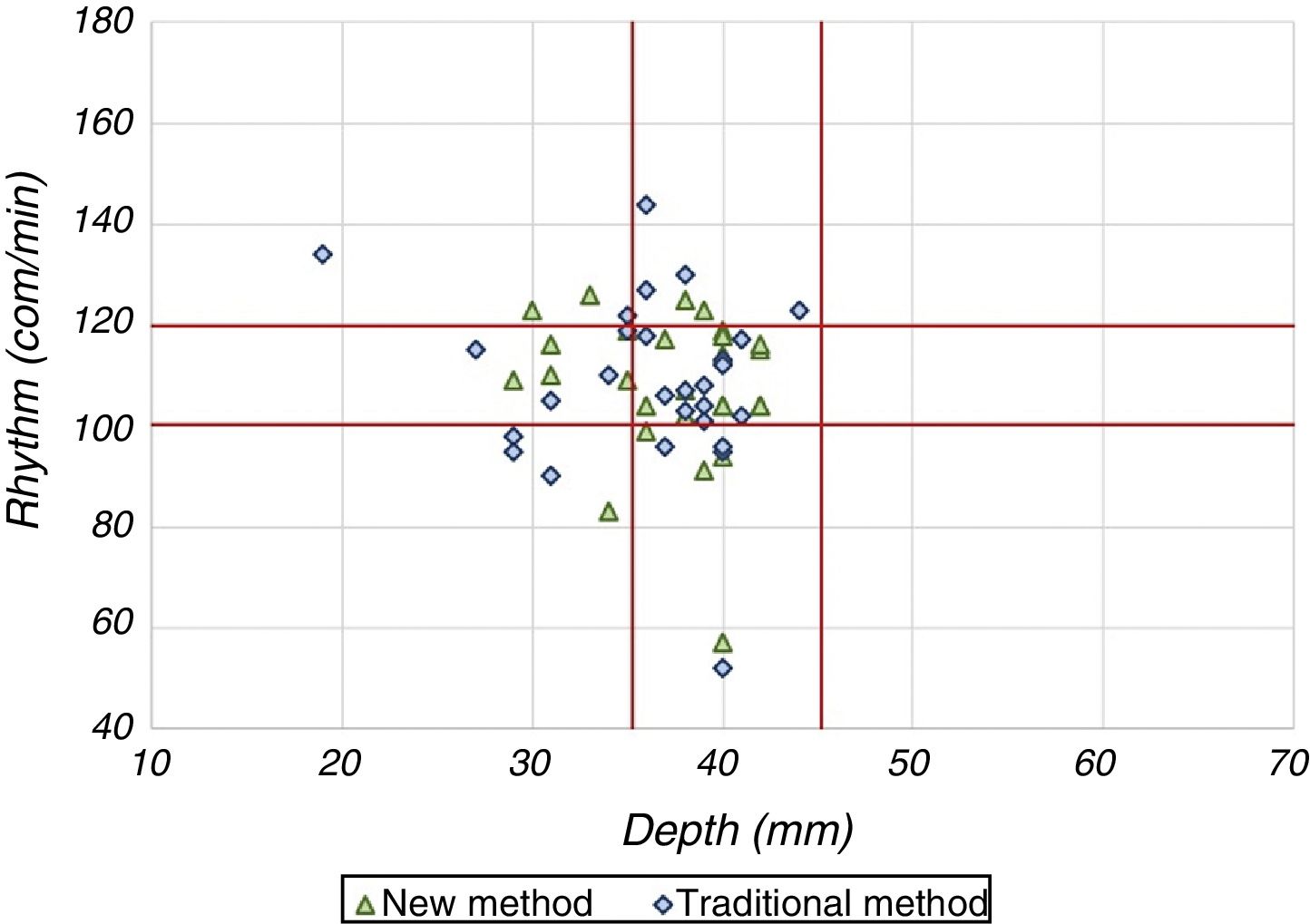
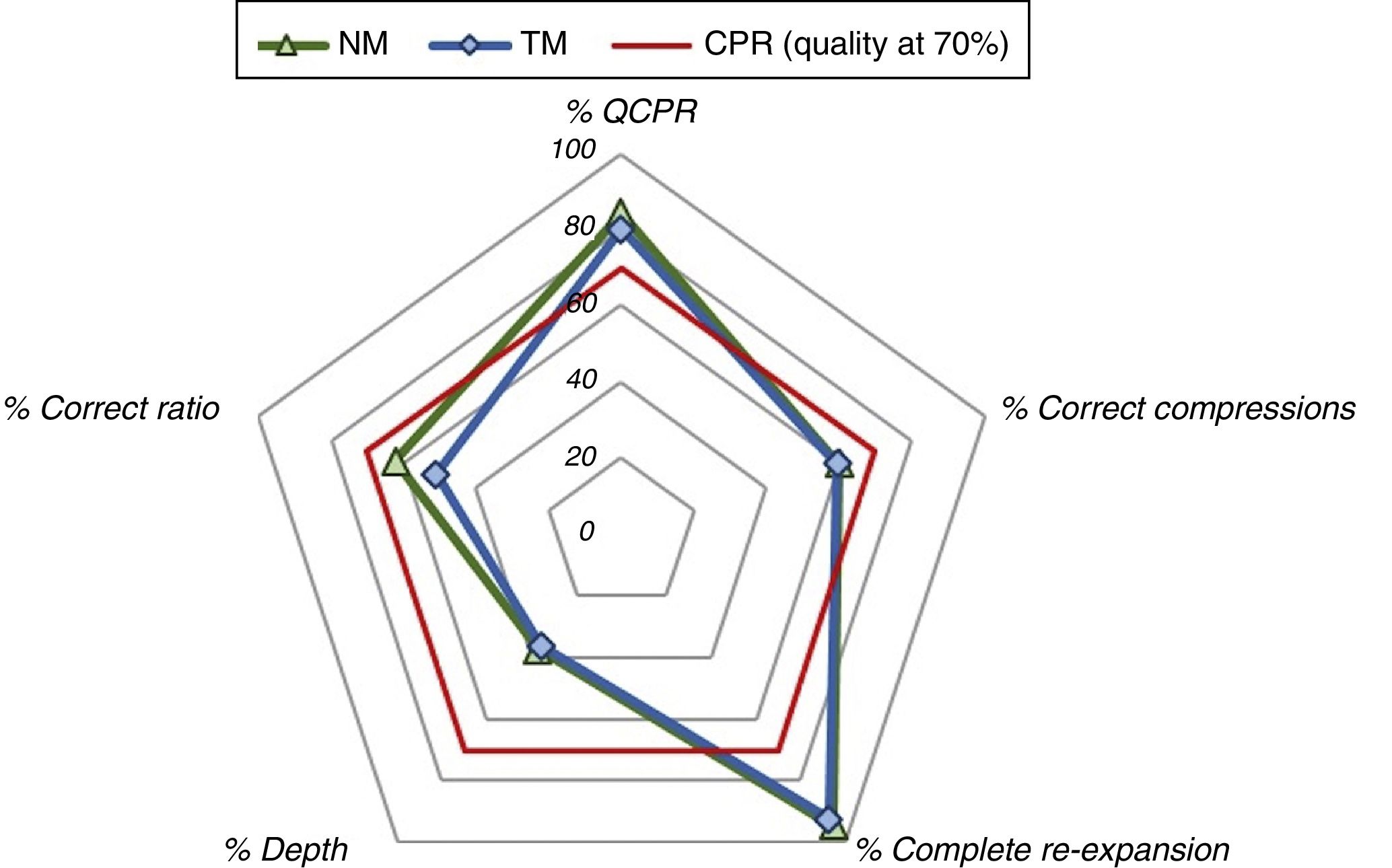
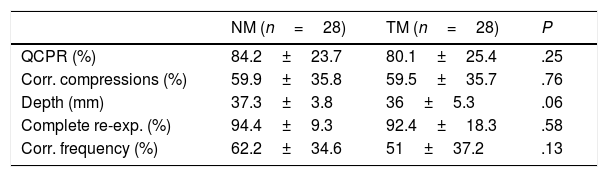
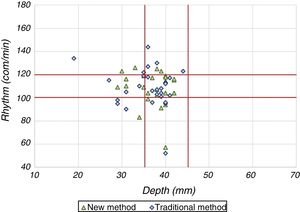
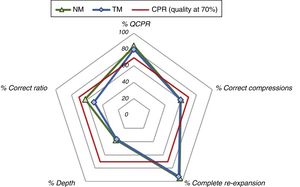
The overall quality of the compressions was similar between the two methods used and there were no significant differences between the two (NM: 84.2±23.7% vs. TM: 80.1±25.4% [P=.25]) (Fig. 4). There were no significant differences either in the percentage of compressions performed at the right depth (NM: 59.9±35.8% vs. TM: 59.5±35.7% [P=.76]), the average depth reached (NM: 37.3±3.8mm vs. TM: 36±5.3mm [P=.06]) (Fig. 5), the percentage of complete rib cage re-expansion (NM: 94.4±9.3% vs. TM: 92.4±18.3% [P=.58]) and the percentage of compressions with the recommended frequency (NM: 62.2±34.6% vs. TM: 51±37.2% [P=.13]) (Fig. 6 and Table 1).
Comparison of quality parameters of chest compressions based on the new method (NM) or the traditional method (TM).
| NM (n=28) | TM (n=28) | P | |
|---|---|---|---|
| QCPR (%) | 84.2±23.7 | 80.1±25.4 | .25 |
| Corr. compressions (%) | 59.9±35.8 | 59.5±35.7 | .76 |
| Depth (mm) | 37.3±3.8 | 36±5.3 | .06 |
| Complete re-exp. (%) | 94.4±9.3 | 92.4±18.3 | .58 |
| Corr. frequency (%) | 62.2±34.6 | 51±37.2 | .13 |
NM: new method; TM: traditional method; QCPR: CPR overall quality; Corr. compressions: compressions with a correct positioning of the fingers; Complete re-exp.: percentage of compressions with sufficient re-expansion; Corr. frequency: percentage of compressions with the recommended frequency.
The difficulty perceived by the participants with every method was 4.5±2.5 over 10 for the NM compared to 4.8±2.1 over 10 for the TM (P=.20).
DiscussionAlthough quality chest compressions are essential if we want to recover spontaneous circulation when managing CRAs, it has been observed that even healthcare providers perform this maneuver sub-optimally, which is why it has been recommended to reinforce the training of this personnel and use (both through courses and in routine clinical practice) real-time monitoring and feedback devices.
In the case of infants, added to the inadequate expertise of healthcare providers, the compression technique per se may not be the most effective of all. That is why the aforementioned new technique has been proposed here in an attempt to improve the outcomes of traditional techniques, especially when it comes to compression depth and in order to maintain quality through time since the wear and tear on the healthcare provider is lower.
Our results are consistent with those from the authors who described this technique20 in the sense that the NM proved to be non-inferior to the TM when used by healthcare providers who had already been trained and had already shown their abilities with the TM but practically knew nothing about the NM (they received a 5min practical class only). These results make us think that if these participants had been properly trained on the NT, their results would have probably been superior to the results obtained with the TM.20 Following our results, it may be interesting to compare both methods used by healthcare professionals well-trained in the management of the NM.
The position of the hands in the NM allows the resuscitator to exert pressure with the entire arm and body weight, which means that chest compressions are also deeper, and the resuscitator's wear and tear is lower compared to the TM where force is exerted by the thumbs only. Also, as Smereka et al.20 showed, when it comes to using the NM, success is not directly influenced by the size of the resuscitator's hands or by the patient's chest diameter as it is the case with the TM, which actually is an advantage when dealing with CRA in big infants and resuscitators with relatively small hands (in many cases, women). However, we did not see this possible advantage in our case since the subjective perception of difficulty when healthcare providers performed the chest compressions was similar with both methods.
Our study has some limitations that should be taken into consideration here. On the one hand, we are talking about a sham setting with manikins, so the results cannot be directly extrapolated to the healthcare provided to real infants. In any case, our data justify conducting studies to evaluate the potential impact of the NM in the management of actual CRAs. The number of individuals included in this study was scarce, although it was large enough to assess the hypothesis of non-inferiority of the NM which actually was our main goal. It is possible that, in order to prove the superiority of the NM, we will need to recruit a larger number of patients, which is something we intend to do in future studies.
In sum, the quality of chest compressions with the new method (compressions using both thumbs and closed fists) is similar to the one obtained with the traditional method. New studies should be conducted on this regard though, both with manikins and actual patients in order to know what the real potential of this new CPR technique is when used in infants.
Author contributionsERR: He participated in the study design, reviewed all data and wrote the final version of this manuscript.
VGM: He collaborated in the review of data, the statistical analysis and was one of the writers of this manuscript.
CAG: He participated in the study design, conducted the statistical analysis, and worked on the figures.
CGG and FSV: They both carried out field work and monitored the quality of data used.
RBF: He participated in the study design and launch and reviewed both the results and this manuscript.
ARN: He participated in the study design, supervised field work, worked on the results, and reviewed the final version of this manuscript.
Conflicts of interestThe authors declared no conflicts of interest whatsoever.
We wish to thank all those who participated in this study.
Please cite this article as: Rodriguez-Ruiz E, Guerra Martín V, Abelairas-Gómez C, Sampedro Vidal F, Gómez González C, Barcala-Furelos R, et al. Nueva técnica de masaje cardíaco en lactantes. Med Intensiva. 2019;43:346–351.