Augmented renal clearance (ARC) is a phenomenon that can lead to therapeutic failure in critically ill patients. In the case of sepsis, the inadequate dose of an antibiotic (AB) worsens prognosis and increases the generation of resistances.1
Definition and epidemiologyAlthough this phenomenon was already described back in the 1970s,2 the ARC is defined today as creatinine clearance (CrCl) levels >130mL/min/1.73mm2.3 The ARC is relevant in patients treated with renal clearance drugs as long as it is significant, that is, as long as the CrCl levels are more than150mL/min/1.73m2 in women and >160mL/min/1.73m2 in men for, at least, four days.3 The prevalence varies between 14% and 80% depending on the type of ICU the study was conducted at.3
Physiopathology and risk factorsThe phenomenon of ARC is due to an acute insult, it can appear at admission in a significant number of patients, and it can remain during the entire first week after its debut at the ICU. Since it is a dynamic phenomenon, follow-up during the entire hospital admission is mandatory in order to avoid overdose or therapeutic failures.4
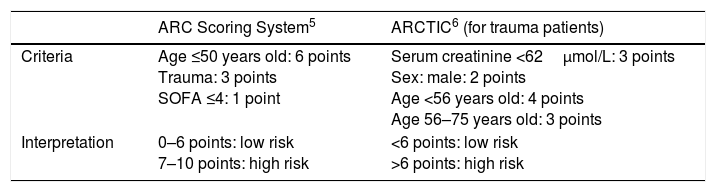
Some contributing factors are high temperature, brain injury, and the systemic inflammatory response syndrome (SIRS). This systemic inflammatory response can be found in trauma patients, pancreatitis, TBI, autoimmune alterations, ischemia, major surgery and sepsis.4 The profile of a hyperfiltrating patient is that of a young (<55 years old) male trauma patient or with an SIRS and lower scores in the severity scales (lower SOFA, SAPS II or APACHE II). Urine creatinine levels >45mg/mL are also considered a risk factor. Several ARC risk scoring systems have been developed so far5,6 (Table 1).
ARC risk scoring systems.
| ARC Scoring System5 | ARCTIC6 (for trauma patients) | |
|---|---|---|
| Criteria | Age ≤50 years old: 6 points Trauma: 3 points SOFA ≤4: 1 point | Serum creatinine <62μmol/L: 3 points Sex: male: 2 points Age <56 years old: 4 points Age 56–75 years old: 3 points |
| Interpretation | 0–6 points: low risk 7–10 points: high risk | <6 points: low risk >6 points: high risk |
ARC, augmented renal clearance; ARTIC, augmented renal clearance in trauma intensive care.
In the routine clinical practice, in order to estimate the glomerular filtration rate (GFR) we use the concentration of serum creatinine or equations based on the level of creatinine, sex, race, ethnic group, etc. However, this is not adequate in cases of ARC, and to be completely sure about diagnosis it needs to be achieved using the GFR. The GFR is the correlation between the urine creatinine level of a volume of urine per unit of time (between 2 and 24h) and the plasma creatinine level.7,8
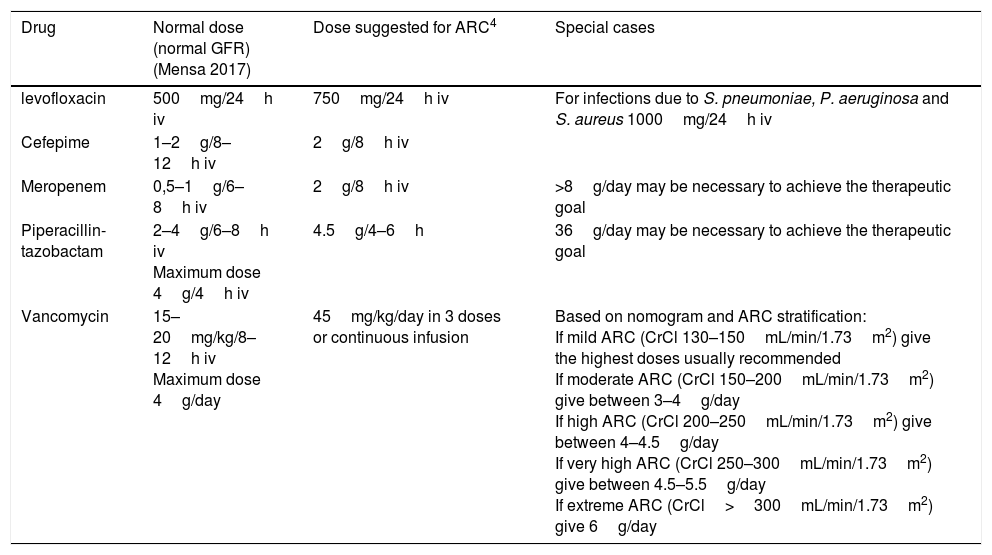
Drug clearance in augmented renal clearanceThe antibiotics that most commonly are involved and relevant in the hyperfiltrating patient are beta-lactam antibiotics (BLAs) (penicillins, cephalosporins, piperacillin-tazobactam, carbapenems and monobactams), aminoglycosides, vancomycin and quinolones such as levofloxacin (Table 2). As a matter of fact, any drugs that are cleared through urine can be affected in cases of ARC. The ARC of these drugs reduces the half-life of the drugs (t½). This is particularly important in time-dependent antibiotics.
Drug dose in hyperfiltrating patients (ARC).
| Drug | Normal dose (normal GFR) (Mensa 2017) | Dose suggested for ARC4 | Special cases |
|---|---|---|---|
| levofloxacin | 500mg/24h iv | 750mg/24h iv | For infections due to S. pneumoniae, P. aeruginosa and S. aureus 1000mg/24h iv |
| Cefepime | 1–2g/8–12h iv | 2g/8h iv | |
| Meropenem | 0,5–1g/6–8h iv | 2g/8h iv | >8g/day may be necessary to achieve the therapeutic goal |
| Piperacillin-tazobactam | 2–4g/6–8h iv Maximum dose 4g/4h iv | 4.5g/4–6h | 36g/day may be necessary to achieve the therapeutic goal |
| Vancomycin | 15–20mg/kg/8–12h iv Maximum dose 4g/day | 45mg/kg/day in 3 doses or continuous infusion | Based on nomogram and ARC stratification: If mild ARC (CrCl 130–150mL/min/1.73m2) give the highest doses usually recommended If moderate ARC (CrCl 150–200mL/min/1.73m2) give between 3–4g/day If high ARC (CrCl 200–250mL/min/1.73m2) give between 4–4.5g/day If very high ARC (CrCl 250–300mL/min/1.73m2) give between 4.5–5.5g/day If extreme ARC (CrCl>300mL/min/1.73m2) give 6g/day |
Source: Mahmoud and Shen's modified Table4. ARC, augmented renal clearance.
Given the characteristics of BLA whose bacterial carrying capacity is time-dependent, we should consider keeping adequate concentrations of the drug whether using the most common doses or extended or continuous infusions.
In the particular case of vancomycin there are already validated nomograms that illustrate how important it is to stratify the ARC9 and, in the case of meropenem, a tool has been developed that predicts the risk of not achieving the therapeutic goal that consists of a free easy-to-use calculator – the «MeroRisk Calculator».10
The load dose that needs to be adjusted to the volume of distribution should not be modified by the fact that a subject is a hyperfiltrating patient.
In the case of aminoglycosides, it is recommended to shorten the interval of administration to 18h instead of using daily administration.
Monitoring the plasma levels is essential if we wish to achieve our therapeutic goals, but it is not always available in the routine clinical practice for most drugs.
In this sense, it would be convenient and necessary to design guidelines on drug dose use based on hyperfiltrating patients and probably adjust the dose to the stratification of the ARC, the same thing that happens with guidelines for renal failure. Here is the stratification we could have: (1) mild ARC (CrCl 130–150mL/min/1.73m2) where the highest doses usually recommended should be used; (2) moderate ARC (CrCl 150–200mL/min/1.73m2) where there should be titration to a higher dose in a given percentage; (3) high ARC (CrCl 200–250mL/min/1.73m2) where there should be titration to a higher dose in a higher percentage than in moderate ARC; (4) very high ARC (CrCl 250–300mL/min/1.73m2) where there should be titration to a higher dose in a higher percentage than in high ARC, and (5), and extreme ARC (CrCl>300mL/min/1.73m2), where there should be titration to a higher dose in a higher percentage than in very high ARC. Thus, we need to design dosing patterns for the routine clinical practice, although today there is still no consensus on this regard.
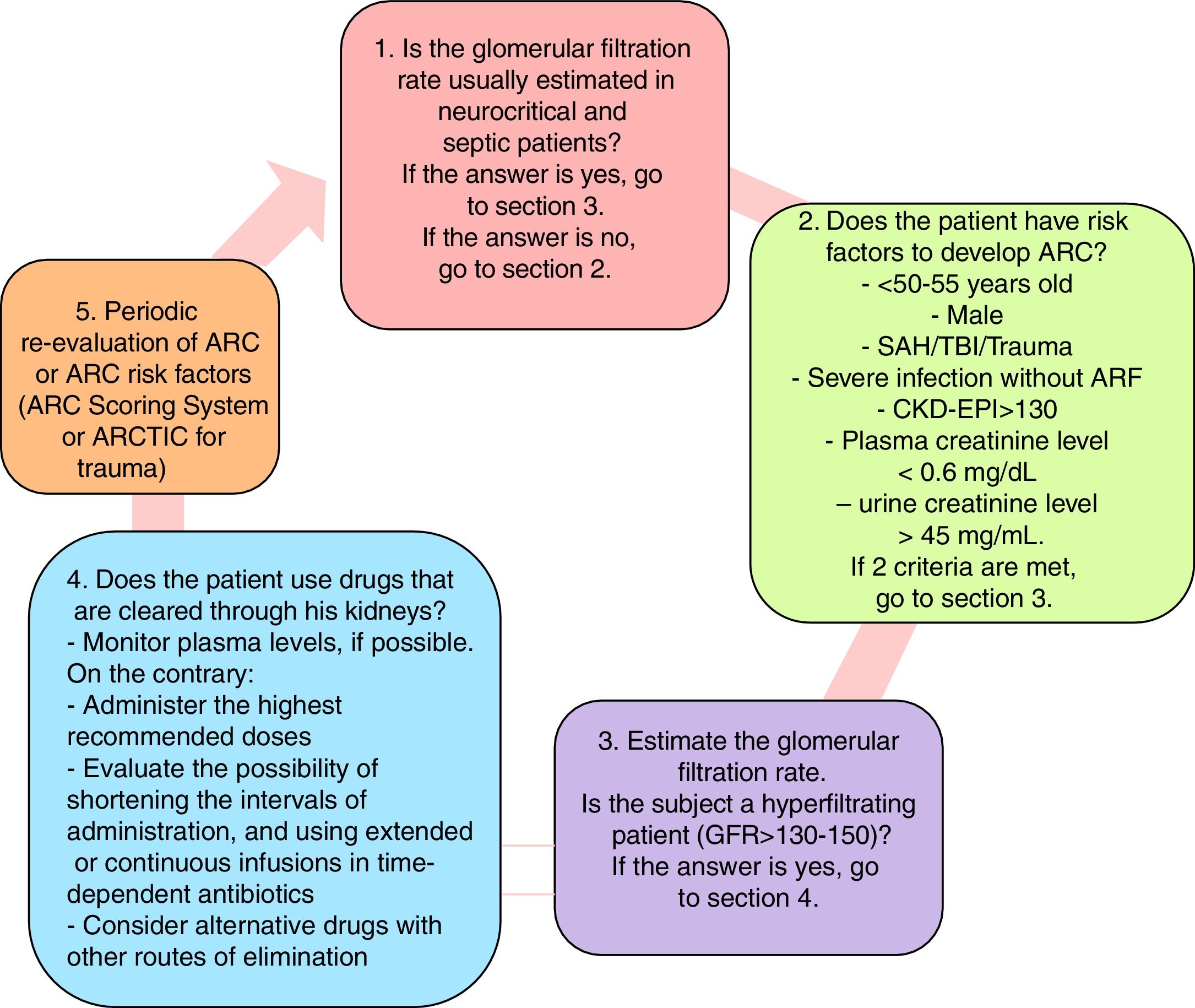
Diagnosis and management algorithm when suspected augmented renal clearanceThe diagnosis and management algorithm when suspected ARC is shown on Fig. 1 where the risk factors for ARC are shown and where it is advisable to determine the glomerular filtration rate. Similarly, a few recommendations are given, and the periodic re-evaluation of ARC is suggested.
Diagnosis and management algorithm when suspected ARC. ARC, augmented renal clearance; ARTIC, augmented renal clearance in trauma intensive care. Source: Mahmoud and Shen's modified algorithm4.
In sum, the critically ill patient can be hyperfiltrating and his diagnosis depends on the degree of clinical suspicion. Since the plasma creatinine level does not stand out, a normal renal function is presumed, and the doses of renal-clearance drugs are titrated consequently. The possible implications that the ARC has are therapeutic failure and the generation of resistances when using antibiotics. Younger age, less severity, inflammatory or neurocritical state are risk factors here. In order to confirm ARC, the glomerular filtration rate should be estimated from the urine collected over a 24-h period of time (between 2 and 24h), follow-up being necessary given the dynamic situation of the critically ill patient.
Conflicts of interestThe author declares no conflicts of interest whatsoever.
Please cite this article as: Tomasa Irriguible TM. Aumento del aclaramiento de creatinina: ¿Cuánto más, mejor? Med Intens. 2018;42:500–503.