The introduction of clinical information systems (CIS) in Intensive Care Units (ICUs) offers the possibility of storing a huge amount of machine-ready clinical data that can be used to improve patient outcomes and the allocation of resources, as well as suggest topics for randomized clinical trials. Clinicians, however, usually lack the necessary training for the analysis of large databases. In addition, there are issues referred to patient privacy and consent, and data quality. Multidisciplinary collaboration among clinicians, data engineers, machine-learning experts, statisticians, epidemiologists and other information scientists may overcome these problems.
A multidisciplinary event (Critical Care Datathon) was held in Madrid (Spain) from 1 to 3 December 2017. Under the auspices of the Spanish Critical Care Society (SEMICYUC), the event was organized by the Massachusetts Institute of Technology (MIT) Critical Data Group (Cambridge, MA, USA), the Innovation Unit and Critical Care Department of San Carlos Clinic Hospital, and the Life Supporting Technologies group of Madrid Polytechnic University. After presentations referred to big data in the critical care environment, clinicians, data scientists and other health data science enthusiasts and lawyers worked in collaboration using an anonymized database (MIMIC III). Eight groups were formed to answer different clinical research questions elaborated prior to the meeting.
The event produced analyses for the questions posed and outlined several future clinical research opportunities. Foundations were laid to enable future use of ICU databases in Spain, and a timeline was established for future meetings, as an example of how big data analysis tools have tremendous potential in our field.
La aparición de los sistemas de información clínica (SIC) en el entorno de los cuidados intensivos brinda la posibilidad de almacenar una ingente cantidad de datos clínicos en formato electrónico durante el ingreso de los pacientes. Estos datos pueden ser empleados posteriormente para obtener respuestas a preguntas clínicas, para su uso en la gestión de recursos o para sugerir líneas de investigación que luego pueden ser explotadas mediante ensayos clínicos aleatorizados. Sin embargo, los médicos clínicos carecen de la formación necesaria para la explotación de grandes bases de datos, lo que supone un obstáculo para aprovechar esta oportunidad. Además, existen cuestiones de índole legal (seguridad, privacidad, consentimiento de los pacientes) que deben ser abordadas para poder utilizar esta potente herramienta.
El trabajo multidisciplinar con otros profesionales (analistas de datos, estadísticos, epidemiólogos, especialistas en derecho aplicado a grandes bases de datos), puede resolver estas cuestiones y permitir utilizar esta herramienta para investigación clínica o análisis de resultados (benchmarking).
Se describe la reunión multidisciplinar (Critical Care Datathon) realizada en Madrid los días 1, 2 y 3 de diciembre de 2017. Esta reunión, celebrada bajo los auspicios de la Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC) entre otros, fue organizada por el Massachusetts Institute of Technology (MIT), la Unidad de Innovación y el Servicio de Medicina Intensiva del Hospital Clínico San Carlos, así como el grupo de investigación «Life Supporting Technologies» de la Universidad Politécnica de Madrid. Tras unas ponencias de formación sobre big data, seguridad y calidad de los datos, y su aplicación al entorno de la medicina intensiva, un grupo de clínicos, analistas de datos, estadísticos, expertos en seguridad informática de datos realizaron sesiones de trabajo colaborativo en grupos utilizando una base de datos reales anonimizada (MIMIC III), para analizar varias preguntas clínicas establecidas previamente a la reunión.
El trabajo colaborativo permitió establecer resultados relevantes con respecto a las preguntas planteadas y esbozar varias líneas de investigación clínica a desarrollar en el futuro. Además, se sentaron las bases para poder utilizar las bases de datos de las UCI con las que contamos en España, y se estableció un calendario de trabajo para planificar futuras reuniones contando con los datos de nuestras unidades.
El empleo de herramientas de big data y el trabajo colaborativo con otros profesionales puede permitir ampliar los horizontes en aspectos como el control de calidad de nuestra labor cotidiana, la comparación de resultados entre unidades o la elaboración de nuevas líneas de investigación clínica.
One of the fundamental challenges intensivists face in the care of the critically ill is the management of a huge amount of information gathered from patients. In intensive care units equipped with electronic information systems, hundreds of individual elements of structured information are collected every day in an electronic chart, including vital signs, basic and advanced monitoring records, laboratory data, drug prescriptions and their administration, as well as nursing records, among others. A lot of textual information, like nurse's and physician's comments and progress notes, is also generated, as well as images of different formats and heterogeneous structure.1
It is impossible for the human brain to fully assimilate this abundance of data, so one of the fundamental qualities of the good intensivist is knowing how to prioritize and filter the most relevant information for a given patient. The exponential growth in computerized information storage and processing systems, however, enables a different approach in which all the available information is taken into account and processed.
Big data analysis (BDA) can be applied to an individual patient, but also be extended to population management of critically ill patients, or to subgroups of patients meeting certain criteria.2 The large volume of data may partially address the lack of “formal” randomization of tests and treatments by presenting instrumental variables with which patients are “pseudo-randomized” to receive or not receive a particular intervention. Analysis of observational data can also generate hypotheses and inform the study design of prospective trials to evaluate those hypotheses. BDA is already routinely employed in other fields as varied as marketing, strategic business decision-making, insurance, banking, transport and logistics services and fraud detection in electronic commerce. Additionally, BDA requires that high quality data are entered by clinicians and nurses.
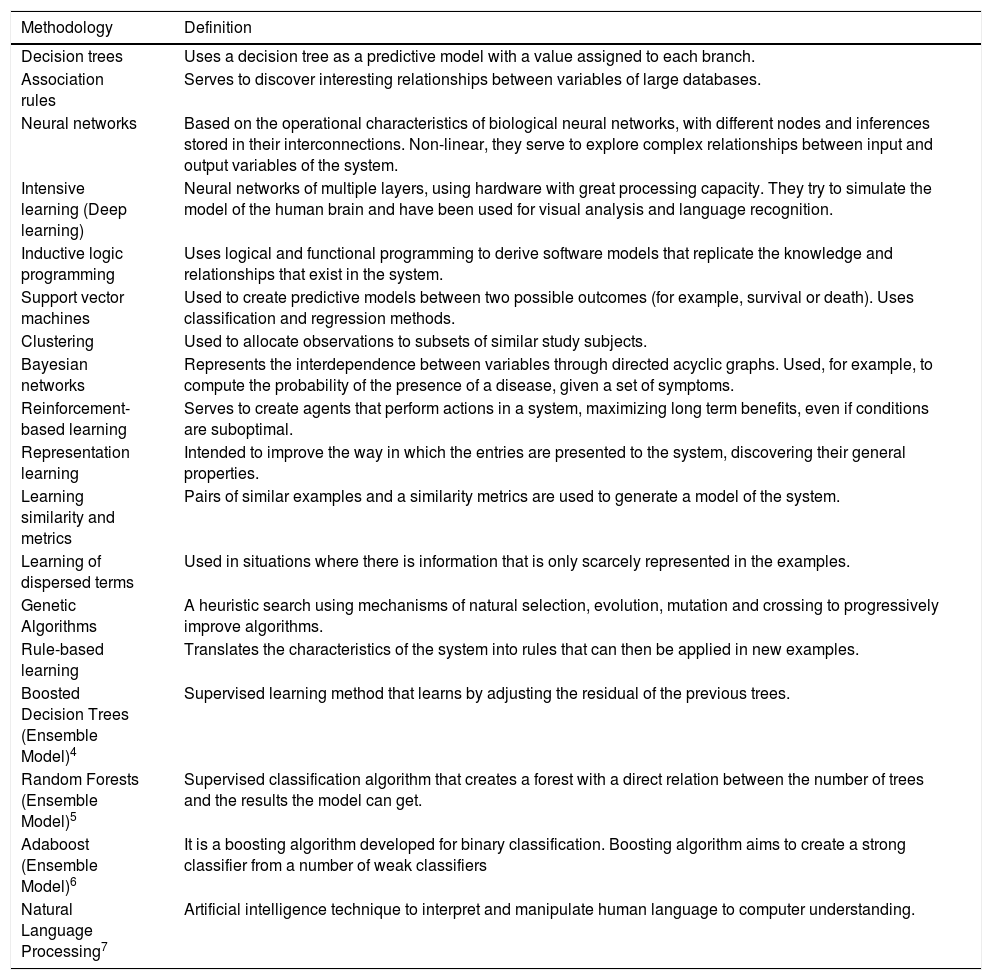
Apart from the data, the other component of BDA is what is referred to as “Machine Learning” (ML), which fuels what is collectively known as artificial intelligence (AI). This technology uses different methodologies (Table 1) to identify patterns from the data which typically involve either classification or event prediction and subsequently apply the software output to a very specific task, such as automatic interpretation of medical images.3 This technology has been used successfully in domains that, until recently, seemed unlikely use cases, such as Jeopardy and the board game Go. Traditional computer systems differ from AI in that in the former, rules are agreed upon by experts and fed into the computers as algorithms. With AI, data is fed into the computers, and the computers “discover” and then implement the rules. In addition, the computers continuously assess the rules and re-calibrate them as needed.
Machine learning methodologies (Refs. 4–7).
| Methodology | Definition |
|---|---|
| Decision trees | Uses a decision tree as a predictive model with a value assigned to each branch. |
| Association rules | Serves to discover interesting relationships between variables of large databases. |
| Neural networks | Based on the operational characteristics of biological neural networks, with different nodes and inferences stored in their interconnections. Non-linear, they serve to explore complex relationships between input and output variables of the system. |
| Intensive learning (Deep learning) | Neural networks of multiple layers, using hardware with great processing capacity. They try to simulate the model of the human brain and have been used for visual analysis and language recognition. |
| Inductive logic programming | Uses logical and functional programming to derive software models that replicate the knowledge and relationships that exist in the system. |
| Support vector machines | Used to create predictive models between two possible outcomes (for example, survival or death). Uses classification and regression methods. |
| Clustering | Used to allocate observations to subsets of similar study subjects. |
| Bayesian networks | Represents the interdependence between variables through directed acyclic graphs. Used, for example, to compute the probability of the presence of a disease, given a set of symptoms. |
| Reinforcement-based learning | Serves to create agents that perform actions in a system, maximizing long term benefits, even if conditions are suboptimal. |
| Representation learning | Intended to improve the way in which the entries are presented to the system, discovering their general properties. |
| Learning similarity and metrics | Pairs of similar examples and a similarity metrics are used to generate a model of the system. |
| Learning of dispersed terms | Used in situations where there is information that is only scarcely represented in the examples. |
| Genetic Algorithms | A heuristic search using mechanisms of natural selection, evolution, mutation and crossing to progressively improve algorithms. |
| Rule-based learning | Translates the characteristics of the system into rules that can then be applied in new examples. |
| Boosted Decision Trees (Ensemble Model)4 | Supervised learning method that learns by adjusting the residual of the previous trees. |
| Random Forests (Ensemble Model)5 | Supervised classification algorithm that creates a forest with a direct relation between the number of trees and the results the model can get. |
| Adaboost (Ensemble Model)6 | It is a boosting algorithm developed for binary classification. Boosting algorithm aims to create a strong classifier from a number of weak classifiers |
| Natural Language Processing7 | Artificial intelligence technique to interpret and manipulate human language to computer understanding. |
Critical care is particularly well suited for machine learning technology, because technology is a large component of the care provided in the ICU with data as an exhaust of the technology.8,9 In fact, there have been ML applications in the ICU, such as in natural language processing, pharmacovigilance and decision support.10 Providers, including intensivists, however, are typically not trained to develop, implement and evaluate such technologies. The next section deals with how to solve this problem.
Collaborative workSince it is would be extremely unusual that one individual would have both the clinical training and the computer science background for BDA and ML, teams with professionals across different fields are required, composed of data scientists including statisticians and epidemiologists, clinicians and other biomedical researchers. The coordination of a group with different schedules, the establishment of clear objectives and an effective leadership to manage members with different cultures and who “speak different languages” are all individual challenges in themselves,11 although in critical care medicine teamwork is routinely applied in the day-to-day workflow.
This article describes an initiative event organized by the Massachusetts Institute of Technology (MIT) Critical Data group, the Life Supporting Technologies (LifeSTech) research group at Universidad Politécnica de Madrid (UPM) and the Innovation Unit and Critical Care Department of Hospital Clínico of San Carlos (HCSC) in Madrid.
Databases of critically ill patientsThe use of BDA and ML techniques creates a new avenue for clinical research that includes non-traditional, non-academic investigators, especially when large anonymized databases of critical patients are shared under pre-specified data user agreement. The pioneers in this field are Beth Israel Deaconess Medical Center and MIT, whose partnership created the MIMIC database (Medical Information Mart in Intensive Care, http://mimic.physionet.org) for the research community. The MIMIC-III version contains data from more than 50,000 admissions to Beth Israel ICUs from the years 2001 to 2012 and is available online under a data user agreement. It includes vital signs and other monitoring data, laboratory results, data of prescription and administration of drugs, as well as progress notes, diagnostic codes, physiologic waveforms, both in the ICU and for some variables, from throughout the entire stay in the hospital.
Similar high-resolution ICU databases exist, like the Critical Care – Health Informatics Collaborative (CC-HIC) Database,12 but MIMIC is unique because it is completely open-access. In addition, the MIT group published a textbook that is available at no cost and teaches a course to guide investigators on the analysis of the database.3,13–15 Since 2016, they have also organized several datathons16 in various regions of the world (MIT, London, Paris, Melbourne, Beijing, Sao Paulo and Singapore), to jumpstart disseminate the field of machine learning as applied to health data.
The creators of MIMIC have proposed a system of learning and continuous improvement in Intensive Care they call “closed circuit”.8 This strategy consists in using the patient database to answer questions of clinical interest and then taking it back to the bedside.
Initiatives in SpainAlthough adoption of electronic medical records and databases of critically ill patients is still in the growth phase in our country, and not all Units have implemented an integrated digital information system, there are already some initiatives under way.
The Spanish Society of Critical Care (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) has published reference standards for the implementation of Clinical Information Systems (CIS),17 and is in the process of building the national electronic record of the minimum basic data set (CMBD) registry to facilitate quality measurement, benchmarking and clinical research.
In some services and hospitals, the process of creating anonymous data bases for collaborative research has already begun. The Critical Care Department at Hospital Clínico San Carlos in Madrid, in collaboration with Philips, has already anonymized its database including its first 12,000 admissions after implementation of the IntelliSpace Critical Care and Anesthesia (ICCA™, Philips) clinical information system. Other ICUs in Spain, such as the Unit at Hospital Joan XXIII in Tarragona, are working on similar initiatives, using the data obtained automatically from their CIS.18,19
The creation and research use of these patient-level databases have some important legal implications, which need to be addressed to comply with regulatory policies, particularly those under the Spanish Data Protection Law. Projects that employ BDA and ML of these patient databases also require prior evaluation and approval by local Ethics Committees.
Critical Care Datathon MadridIn order to promote the use of BDA and ML in healthcare in our country, the seventh Critical Care Datathon, organized jointly by the MIT Critical Data Group, the HCSC in Madrid and the LifeSTech from UPM, took place on December 1, 2 and 3, 2017 at Impact-Hub co-working space in Madrid. The event brought together clinicians, computer scientists and other professionals interested in health data science. HCSC and LifeSTech-UPM group collaborated in the event diffusion informing participants about the content and meaning of the Datathon.
Prior to the event, a group of clinicians from the Critical Care Department of Hospital Clínico San Carlos prepared a list of eight research questions of clinical interest, by way of brain storming, discussion and reaching internal agreement, to be explored during the event: (1) the choice of empirical antibiotics in the ICU on hospital mortality, (2) risk factors for prolonged ICU stay and mortality after cardiac surgery, (3) prediction of poor prognosis after admission for resuscitated out-of-hospital cardiac arrest, (4) prediction of mortality in patients with non-elective ICU admission, (5) prognostic implications of hyperglycemia in critically ill patients with and without diabetes, (6) the epidemiology of massive transfusion of packed blood cells, (7) understanding the association of positive fluid balance and mortality, and (8) seasonality of subarachnoid hemorrhage.
After brief presentations of the background and the rationale behind the research questions with consideration of the non-healthcare professionals among the Datathon attendees, eight groups were formed, one for each topic, with the stipulation that all the necessary expertise (clinical, data extraction and processing, machine learning) is represented in each group.
The MIT Critical Group with the support of LifeSTech from UPM set up for the event virtual servers with the MIMIC-III database with access to platforms and software for data analysis (Python, R, Jupyter notebook). LifeSTech evaluated using natural language processing techniques to extract information from clinician's reports written in free text, with the purpose of codifying them through SNOMED-CT terminology.20 Mentors from the MIT team and LifeSTech were on hand throughout the weekend to help troubleshoot issues, both technical and those related to the MIMIC database or to data modeling. Finally, each group presented their methods and results to the rest of attendees and a panel of judges from MIT, UPM and HCSC.
As an illustration of the relevant conclusion rendered by the collaborative work of the groups during the datathon, we briefly describe the experience of the group who worked on the project looking at the prediction of mortality among patients with non-elective ICU admission.
First, the clinician in the team presented the existing critical care mortality prediction models (APACHE II, MPM, SAPS 2, SAPS 3), and interest in developing an updated score with better calibration from a larger database. A literature search was carried out to select the scores with the best performance for comparison. The OASIS21 and APACHE II22 scores were chosen as the current “gold standard”. OASIS, which was constructed using ML techniques, has the best performance among critically ill patients in the MIMIC III database (area under the receiver operating curve or AUROC, 0.82) (personal communication from MIMIC team), while the APACHE II score, the most frequently used for benchmarking and clinical research, has an AUROC of 0.75.23
Likewise, the clinician identified variables in MIMIC-III potentially related to prognosis. The data scientists were responsible for generating the table of more than 40,000 patients with all the selected variables. The entire team went over phases of the model building. In the first phase (training), Support Vector Machines (SVM) was trained using 25,000 patients and produced a model of 30 variables with an AUROC of 0.81. This performance was validated in a different subset of 15,000 patients, with a similar AUROC, confirming the robustness of the model. Presently, the group is working in refining the model and evaluate its performance in the anonymized ICCA™ (Philips) database with 12,000 patients of our Critical Care Department.
The same collaborative work between clinicians and data scientists performed in previous similar events and that we witnessed in the Madrid Datathon, has led to numerous publications,24–28 and we have the same expectation from the Madrid event.
The meeting, which was organized under the auspices of SEMICYUC, also served to connect Spanish ICUs working in the field of BDA and fortified partnerships among them to move this initiative forward.
What the future holds and conclusionsWe are conceivably at the dawn of a new era in intensive care, in which clinical decision making will increasingly be assisted by computers that perform data integration and analysis. The clinician will therefore have to navigate a specialty of critical care, that harnesses the power of data to individualize care in order to improve population health, where collaborative work with other non-healthcare specialists in the area of data science is essential to leverage all the information that is routinely collected in the process of care, but without compromising patient rights to privacy.
We encourage all those interested in participating in this project to contact the authors, in order to establish a national collaborative network in the field of BDA and ML as applied to healthcare data collected in the ICU, under the auspices of SEMICYUC.
Author's contributionsMIMIC III experts: Celi, Armengol, Deliberato, Paik, Pollard, Raffa, Torres.
Technical logistics (servers and database access): Celi, Armengol, Deliberato, Paik, Pollard, Raffa, Torres, Mayol, Chafer, Rey, Gonzalez, Fico, Lombroni, Hernandez, Lopez, Merino, Cabrera, Arredondo.
Preparation and presentation of research questions: Blesa, Martín, Nieto, Martínez, Álvarez, Sánchez, del Pino, Gil, Núñez.
Clinical support for the research questions: Sanchez, Núñez, Álvarez, Martínez, del Pino, Gil, Bodí, Rodríguez, Gómez, Prada.
Concept and Design of the Datathon: Celi, Armengol, Deliberato, Paik, Pollard, Raffa, Torres, Mayol, Chafer, Rey, Gonzalez, Fico, Lombroni, Hernandez, Lopez, Merino, Cabrera, Arredondo.
Drafting of the manuscript: Núñez, Sánchez, Celi, Bodí, Fico, López.
Venue of the event: Gonzalez, Mayol, Chafer, Rey.
Diffusion: Chafer, Rey, González, Sánchez.
Conflict of interestsThe authors declare no conflict of interests.
List of authors who have participated in the Organizing Committee of Critical Care Datathon Madrid 2017.
Critical Care Department, Hospital Clínico San Carlos, Madrid
Antonio Núñez Reiz MD* (anunezreiz@gmail.com), Miguel Sánchez García MD PhD*, Fernando Martínez Sagasti MD PhD, Manuel Álvarez González MD PhD, Antonio Blesa Malpica MD PhD, Juan Carlos Martín Benítez MD PhD, Mercedes Nieto Cabrera MD PhD, Ángela del Pino Ramírez MD, José Miguel Gil Perdomo MD, Jesús Prada Alonso
*Corresponding authors.
MIT Critical Data group, Massachusetts Institute of Technology, Boston
Leo Anthony Celi MD MS MPH, Miguel Ángel Armengol de la Hoz MBE, Rodrigo Deliberato MD PhD, Kenneth Paik MD MS MBA, Tom Pollard PhD, Jesse Raffa PhD, Felipe Torres
Unidad de Innovación, Instituto de Investigación Sanitaria San Carlos
Julio Mayol MD PhD, Joan Chafer MD, Arturo González Ferrer PhD, Angel Rey, Henar Gonzalez Luengo
Life Supporting Technologies, Universidad Politécnica Madrid
Giuseppe Fico PhD, Ivana Lombroni MsC, Liss Hernandez MsC, Laura Lopez MsC, Beatriz Merino MsC, Maria Fernanda Cabrera PhD, Maria Teresa Arredondo PhD.
Intensive Care Unit, Hospital Universitario Joan XXIII, Instituto de Investigación Sanitaria Pere Virgili, Rovira i Virgili University, Tarragona, Spain
María Bodí MD PhD, Josep Gómez PhD, Alejandro Rodríguez MD PhD