Point-of-care ultrasound (POCUS) has revolutionized the care of the critically ill patient, serving as a useful tool in the diagnosis and monitoring of a wide range of clinical scenarios, and providing interventional guidance as well.1 Regarding the last point, ultrasound-guided central venous cannulation (USCVC) is the main procedure performed in the intensive care unit (ICU) adult patient, although it is not used as frequently as expected, since approximately half of the central venous catheters are placed under ultrasound guidance.2 The evidence for USCVC in the critically ill adult patient is clear. Improved cannulation success and reduced complications such as arterial puncture are well demonstrated, strongly indicating that all cannulations should be performed under ultrasound guidance.3–5 For the critically ill pediatric patient, the evidence is more limited. In this regard, the study of Pietroboni et al.6 provides light in that issue and confirmed what was a priori expected: USCVC (femoral vein) is better than the landmark technique. Selection of this vein for cannulation looks wise since it avoids any possibility of needle-stick injury of the pleura or the carotid artery which could add serious morbidity to the patient when attempting veins of the upper body, and also because, in the pediatric field, the femoral catheters have similar rates of infection when compared with non-femoral catheters.7 Improved cannulation of this vein and reduced arterial puncture using ultrasound guidance when compared with the traditional technique are the key findings of this study.
In addition, several other points of this investigation are worth mentioning.
Firstly, to perform USCVC with proficiency, intensivists must be properly trained. Otherwise, cannulation success is compromised and, more importantly, patient safety is at risk. In this study, intensivists’ training for USCVC was achieved through a combination of 2-h theory and 2-h practice in vascular phantom models. Although this short 4-h training sounds enough at first glance, it is important to know how many “real” USCVC were performed by these practitioners before the study, since if experienced practitioners performed most cannulations, this could explain the favorable results observed in the USCVC group. However, a point of this training merits consideration and is worth to be reinforced: using phantoms is a “must do”. Using vascular phantoms helps trainees to learn all the practical variables of the procedure, without putting any patient at risk. Several phantom models have been created and although a “champion phantom” does not seem to exist, one model deserves attention: those created with chicken breast (simulating the background echogenicity) and modeling balloons (simulating the vessels).8,9 This phantom replicates accurately the ultrasound appearance of vessels and surrounding tissues and, what is also important, the resistance of the tissues as the needle is advanced. In addition, it is reusable, affordable, and allows practitioners to perform multiple punctures over the entire training session given that balloons (vessels) are easily filled and replaced. Also, varying degrees of complexity can be created, for example, changing vessel depth and/or using smaller or even partially filled balloons, simulating hypovolemic veins.8
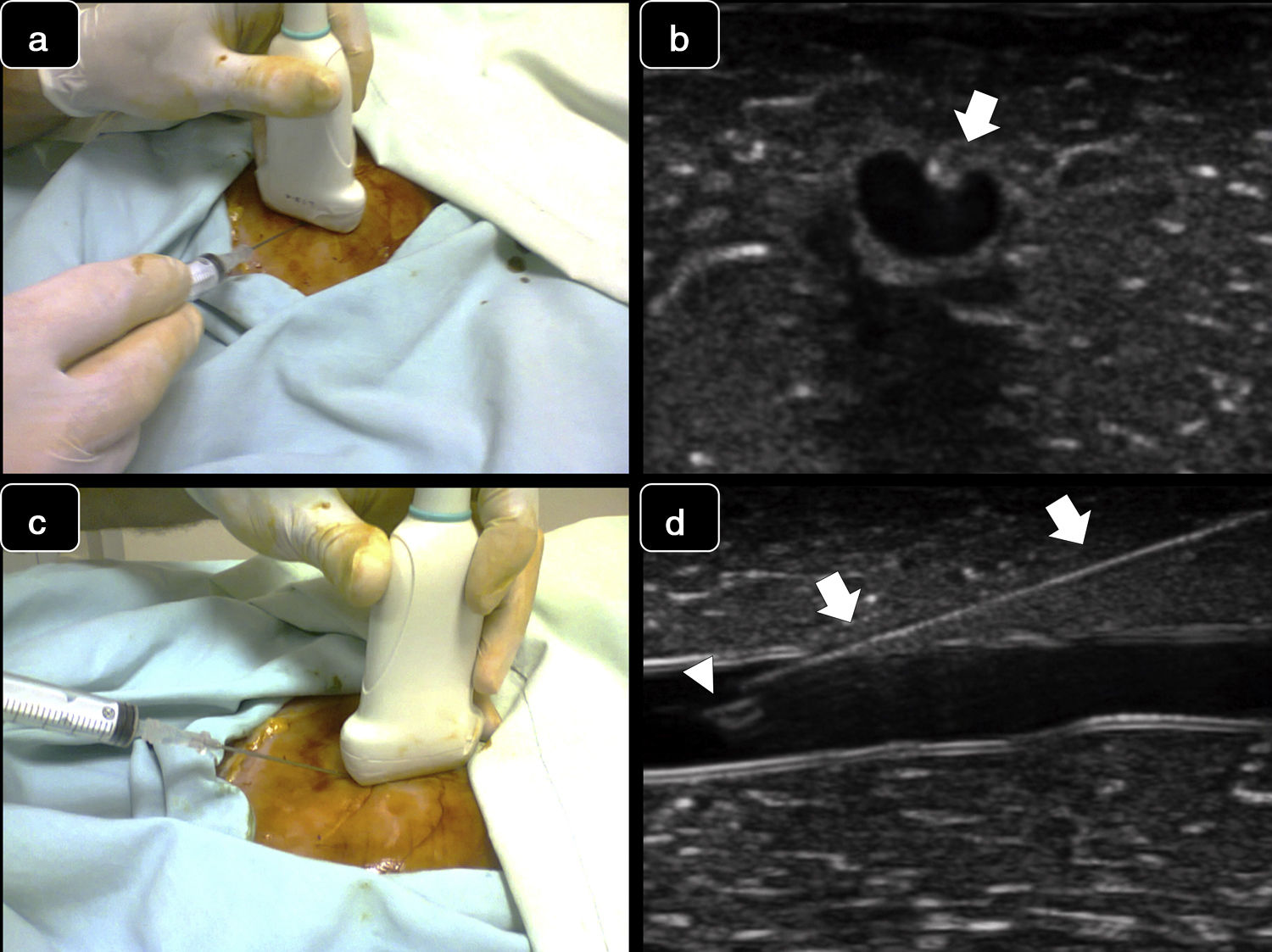
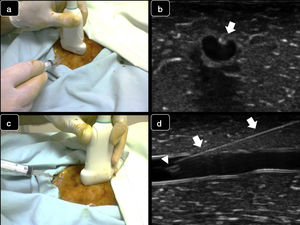
Secondly, a few comments regarding the USCVC approach and the vein size. As it is known, the out-of-plane and the in-plane technique have advantages and disadvantages, and one or the other can be chosen based not only on operator preference, but also considering other characteristics such as the size of the vein or the spatial relation between the vein and the artery. Briefly, the out-of-plane cannulation technique is performed when the vessel is in the short axis, and, after the vein is centered on the screen, the needle is inserted at the middle of the transducer and then is advanced intersecting the ultrasound beam. The needle is visualized as an echogenic spot entering from superficial tissues up to the desired vessel; movement of superficial tissues and flattening of the anterior vessel wall are also observed as the needle is advanced (Fig. 1a and b). Since the needle tip often exceeds the body of the transducer as is inserted, the needle shaft and needle tip cannot be clearly differentiated in this approach. The out-of-plane technique is better to control the needle at the sides of the vein, and thus preferable to be used when the vein is next to the artery. Also, when the vein is large and close to the transducer, the out-of-plane technique offers a rapid way for the needle to enter into the vein, without wasting time or adding extra complexity if an in-plane technique is attempted (see below). While distinguishing the needle tip versus the needle shaft can be challenging when using the out-of-plane approach and this is a key factor that is associated with an increased incidence of perforation of the posterior vessel wall, the walkdown or “follow the tip” maneuver aids in improving needle tip recognition and should be routinely used in out-of-plane cannulations.3 The in-plane cannulation technique is performed when the vessel is in the long or in the oblique-axis, and the needle is inserted and advanced from one corner of the transducer following the path of the ultrasound beam; the needle is clearly depicted (shaft and tip) as advanced from superficial tissues up to the desired vessel (Fig. 1c and d). To do this accurately, an excellent alignment between the ultrasound beam and the needle is required with this approach, otherwise, cannulation will not be successful and complications may arise, such as posterior vessel wall perforation or injuring a structure at the sides of the desired vessel.3 In contrast to the out-of-plane technique, the in-plane approach offers a better control of the needle tip and thus, for example, when the vein is mounted over the artery, aids in controlling the needle tip and minimizing the risk of perforating the posterior venous wall and puncturing the artery. It would be important to know which approach was preferred in this investigation, the reasons behind it and if there is a difference between the two approaches in cannulation outcomes.
Real-time techniques for ultrasound-guided vascular cannulation. Upper panel: short axis, out-of-plane technique. (a) The needle is inserted at the middle of the transducer and then is advanced; (b) Corresponding ultrasound images. The needle is observed as an echogenic spot (arrow) along with flattening of the anterior vessel wall. Lower panel: long axis, in- plane technique: (c) The needle is inserted and advanced from one corner of the transducer; (d) Corresponding ultrasound images. The needle is entirely observed (arrows), including the bevel (arrowhead) inside the vessel.
Regarding vein size, it would be interesting to detail if in this study a cut-off vein diameter was related with more feasible ultrasound-guided cannulations. For example, in adults, this is >7mm for central veins, and >4mm for peripheral veins.3,4,10 Knowing the vein size is also of value when selecting the catheter size, since intuitively smaller catheters are suitable for smaller veins, and vice versa. Among other variables, a catheter occupying a large proportion of the vein lumen predisposes to vein thrombosis and infection. While the catheter size is often selected based on clinical needs (e.g., hemodialysis catheters are necessarily bigger than a simple central catheter), as a rule of thumb, for the most common types of central venous lines, the AP diameter of the vein indicates the maximum catheter Fr that should be selected for cannulation. For example, a 5-Fr catheter is suitable for a 5-mm or bigger vein.
Finally, although more studies using ultrasound as a guidance to cannulate the femoral vein are needed, trained operators should use ultrasound guidance each time they need to cannulate this vein, since its benefits seem to overcome its drawbacks. As stated by authors, further investigations about the role of ultrasound guidance to cannulate other central veins are necessary in pediatrics, as well as to cannulate peripheral veins.
This work has not been presented at any conferences.