To evaluate the quality of cardiopulmonary resuscitation (CPR) by lay people when guided by a mobile phone application with real-time feedback, with the comparison of three different mobile phone applications (APPs).
DesignA cross-sectional quasi-experimental study was carried out.
ParticipantsA sample of 113 nursing students participated in the study.
InterventionsThree hands-only CPR tests with continuous compressions were performed: (i) without external help; (ii) with the mobile phone turned off; and (iii) guided by APP. Three different APPs were randomly assigned (Pocket CPR®, CPR Pro® and Massage cardiaque et DSA®). The mannequin Laerdal Resusci Anne QCPR (Stavanger, Norway) 2.0.0.14 software was used.
Variables of primary interestAPPs used. Demographic variables characterizing the study sample. Independent variables: mean depth, mean rate, percentage of correct hand positioning, percentage of compressions with correct re-expansion, percentage of compressions with correct depth, percentage of compressions at the correct rate, and overall quality of CPR.
ResultsOverall CPR quality was 33.3±32.7% using Pocket CPR, 10.9±22.72% using CPR Pro and 7.8±9.2% using Massage cardiaque et DSA. None of the APPs produced a statistically significant improvement. The percentage of time that the resuscitator managed to maintain a correct compression rate improved when using all three APPs.
ConclusionsCardiopulmonary resuscitation guided by phone APPs did not improve the overall quality of compressions during resuscitation, though it improved the percentage of compressions performed at the correct rate.
Evaluar la calidad de la reanimación cardiopulmonar (RCP) de personas no expertas guiada por una aplicación móvil con retroalimentación en tiempo real.
DiseñoEstudio cuasi-experimental de corte transversal.
ParticipantesUna muestra de 113 estudiantes de enfermería sin experiencia ni formación en RCP participaron en el estudio.
IntervencionesSe realizaron tres test de RCP solo manos con compresiones continuas: 1) RCP sin dispositivo; 2) RCP con el teléfono apagado, y 3) RCP guiada por APP. Se aleatorizaron tres aplicaciones diferentes (Pocket CPR®, CPR Pro® y Massage cardiaque et DSA®). Los tres test se realizaron de forma consecutiva, aleatorizados y separados 30min entre cada uno. Se utilizó el maniquí Laerdal Resusci Anne QCPR (Stavanger, Noruega) software 2.0.0.14.
Variables de interés principalesAplicaciones utilizadas. Variables demográficas para caracterizar a la muestra. Variables independientes: media de profundidad, ritmo medio, porcentaje de posición correcta de mano, porcentaje de compresiones con reexpansión correcta, porcentaje de compresiones con profundidad correcta, porcentaje de compresiones al ritmo correcto, calidad global de la RCP.
ResultadosLa calidad global de la RCP fue del 33,3%±32,7 para Pocket CPR, del 10,9%±22,72 para CPR Pro y del 7,8%±9,2 para Massage cardiaque et DSA. Con ninguna de las APP se consiguen mejorías estadísticamente significativas. El porcentaje de tiempo que el reanimador consiguió mantener el ritmo correcto mejoró con el uso de las tres APP.
ConclusionesLa RCP guiada por APP no mejoró la calidad global de las compresiones durante la reanimación, si bien mejoró el porcentaje de compresiones realizadas a un ritmo correcto.
Every year there is some 50000 out-of-hospital cardiorespiratory arrests (OHCA) in Spain that amount to up to 10% of the total number of dead patients.1,2 One of today's challenges is to increase the rate of witnesses involved in OHCAs3–5 and improve the quality of cardiopulmonary resuscitation (CPR) since it often does not follow the actual recommendations.6,7
As part of this effort to transform society and make it more CPR proactive and aware, mobile technology, the social media, and digital platforms are contributing to learning and training in resuscitation protocols for especially young populations.8
Smartphone mobile applications (app) are the leading platforms9 for learning purposes and to find witnesses close to where the incident occurs.10 Also, they can simulate the devices that provide feedback when performing chest compressions and ventilations11,12 and they have been confirmed to improve the quality of the CPR.13
Most of these apps use the information provided by the 3-axis accelerometer mounted on smartphones to translate these data into values of depth, rhythm, and number of compressions. This means that the device needs to be hand-held while the CPR maneuvers are being performed. However, we do not know much about the interferences that can occur holding a smartphone while performing chest compressions. We do not know much either about the app capacity to do the information follow-up or if it can impact the quality of the CPR.
The goal of this study was to assess the quality of app-guided CPR techniques performed by nonexperts with real time feedback.
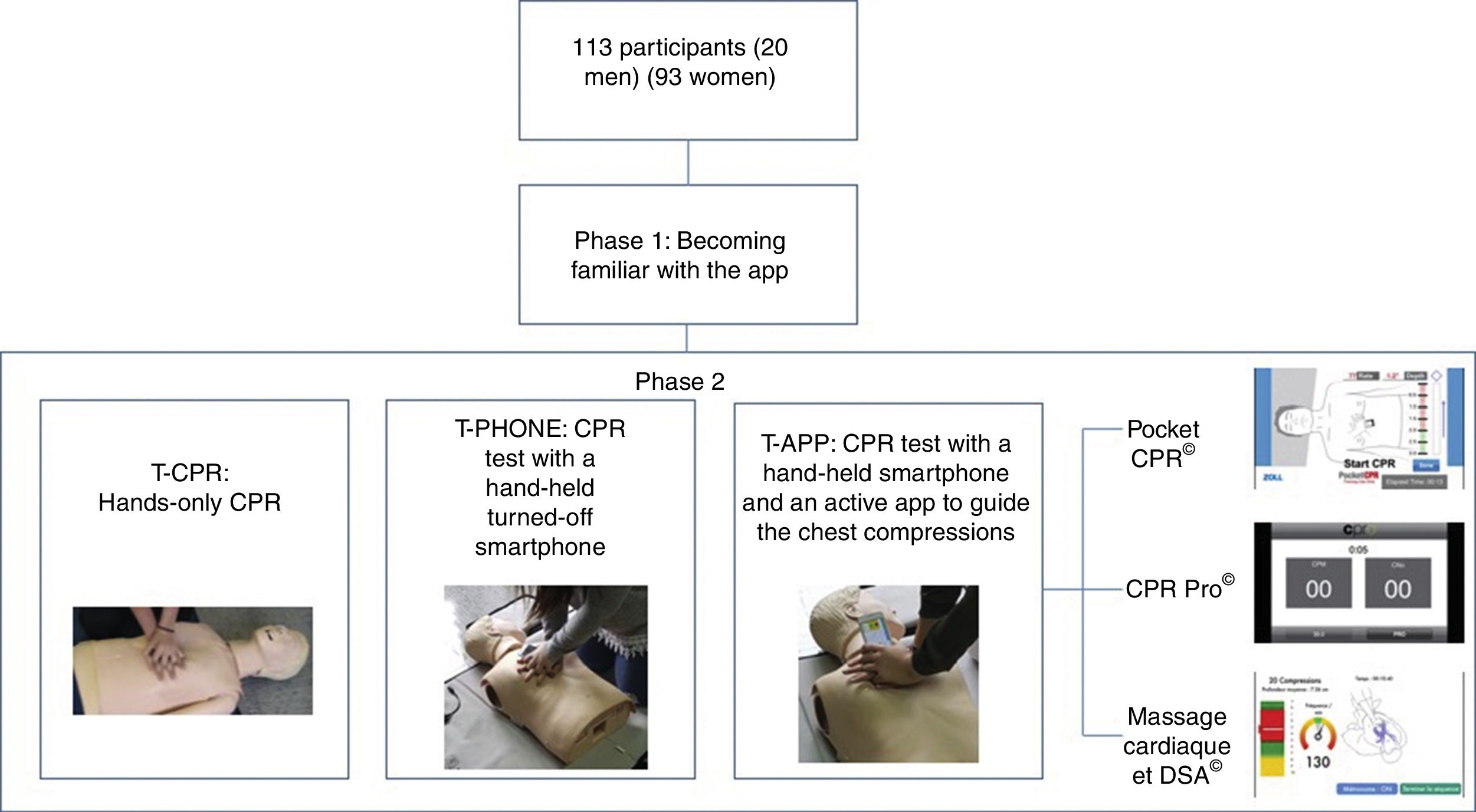
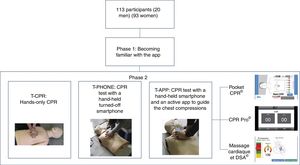
Material and methodA quasi-experimental cross-sectional study was conducted. Randomization was performed intergroup (the app that would be used was assigned) and intragroup (the order in which the tests would be run was assigned too). The quality of the CPR was compared in 3 situations: (1) CPR test without device [T-CPR]; (2) CPR with a turned-off smartphone [T-PHONE], and (3) app-guided CPR randomizing 3 different apps [T-APP].
SampleA convenience sample of 113 first year nursing students was invited to participate in the study. Inclusion criteria were that they knew how to use a smartphone and had no prior CPR training and/or know-how. Exclusion criteria were that they had prior CPR training or experience or physical disabilities limiting them from conducting this experiment.
All individuals were previously informed of the goals of the study and gave their written informed consent for their participation. They were told that they would not be rewarded or penalized for their participation. Results were anonymous through random coding. This study observed all ethical principles established by the Declaration of Helsinki.
Since this was a sham study with manikins, approval from the hospital ethics committee was not deemed necessary.
App and smartphoneThe following apps are free of charge for IOS with feedback during the CPR and were used while conducting our research (Fig. 1):
- a)
Pocket CPR® (Zoll Medical Corporation, Chelmsford, MA, United States).
It provides sound feedback with voice messages and visual information on the rhythm of compressions per minute and depth of the compressions performed, metronome, and measures for how long the CPR has been going.
- b)
CPR Pro® (Ivor Medical, Leeds, United Kingdom). It provides feedback on the rhythm of compressions per minute, metronome and counts the number of compressions performed.
- c)
Massage cardiaque et DSA® (MC et DSA) (Imaios, Montpellier, France). It provides feedback on the depth and rhythm of compressions per minute, counts the number of compressions performed, metronome, and measures for how long the CPR has been going.
All apps were installed on an Iphone5S® smartphone (Apple Inc., Cupertino, CA, United States).
Becoming familiar with the techniqueTo avoid use bias and test the app more reliably, participants were allowed to become familiar with the indications of the app with which they would be running the tests. Also, to spend time learning how they would hold the phone while performing the compressions. Right when the test was about to start, an instructor accredited by the CPR National Plan instructed the participants to “steadily compress the center of the chest”. No participant performed any compressions on the manikin before running the tests.
CPR test and manikinEach participant ran 3 hands-only CPR tests of 2-min duration each (Fig. 2):
- 1)
CPR test without device [T-CPR].
- 2)
CPR test with a hand-held turned-off smartphone [T-PHONE].
- 3)
CPR test with a hand-held smartphone plus an active app to guide the chest compressions [T-APP].
To avoid learning effect the order in which the tests would be run was randomized. To minimize the effect of fatigue each CPR technique was performed with a 30-min timeframe separation.
The Laerdal Resusci Anne QCPR adult training manikin (Stavanger, Norway) was used to perform the CPR measurements.
VariablesDemographic data were gathered to characterize the sample. Independent variables were average depth (AD) in mm; average rhythm (AR) of compressions per minute; percentage of compressions with proper hand placement (PHP); percentage of compressions with correct re-expansion (CCR); percentage of correct chest compression depth (CCD); percentage of compressions at correct rhythm (CCR); and overall quality (QCPR) according to the ERC guidelines of 2015.14 These variables were registered using the Laerdal Resusci Anne Wireless SkillReporter software version 2.0.0.14 (Stavanger, Norway). The Resusci Anne Wireless SkillReporter® software provides a general parameter called quality of cardiopulmonary resuscitation (QCPR) based on the 4 variables of cardiac massage (depth, rhythm, hand placement, and re-expansion). This is a widely used variable in studies with Laerdal simulators.15–17 The result provided goes from 0% to 100%. If the performance of the CPR deviates from the standard, the score goes down. The higher the deviation the lower the score. In regard to the QCPR variable, percentages >70% were considered quality CPR.18
Statistical analysisStatistical analysis was performed using IBM SPSS statistical software package version 20 (SPSS, Inc., Chicago, IL, United States). Results are expressed as central tendency measurements (mean) and dispersion (typical deviation and confidence interval). To verify the normality assumption of the sample the Kolmogorov–Smirnov test was used. For the intragroup analysis, the repeated measures ANOVA model with Bonferroni correction was used for variables with normal distribution. The Friedman test was used for the variables that did not meet this criterion. The Wilcoxon signed rank test was used for pair comparisons of cluster data. P values <.05 were considered statistically significant.
Lastly, the effect sizes (ES) in all pair comparisons were calculated. Cohen test was used with variables with normal distribution and Rosenthal test with variables with non-normal distribution. To describe the ES, the parameters assigned by Cohen19 and expanded by Rosenthal were used20: trivial (<0.2), small (0.2–0.5), medium (0.5–0.8), large (0.8–1.3) and very large (>1.3).
ResultsThe overall sample (n=113) included 82.3% women (n=93) and 17.7% men (n=20). The mean age of female participants was 19.7±4.2 years and the mean age of men was 18.9±1.4 years.
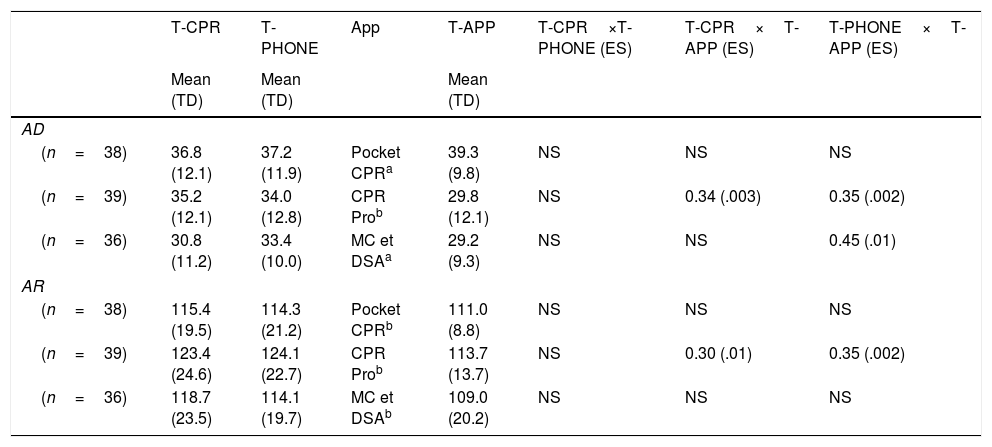
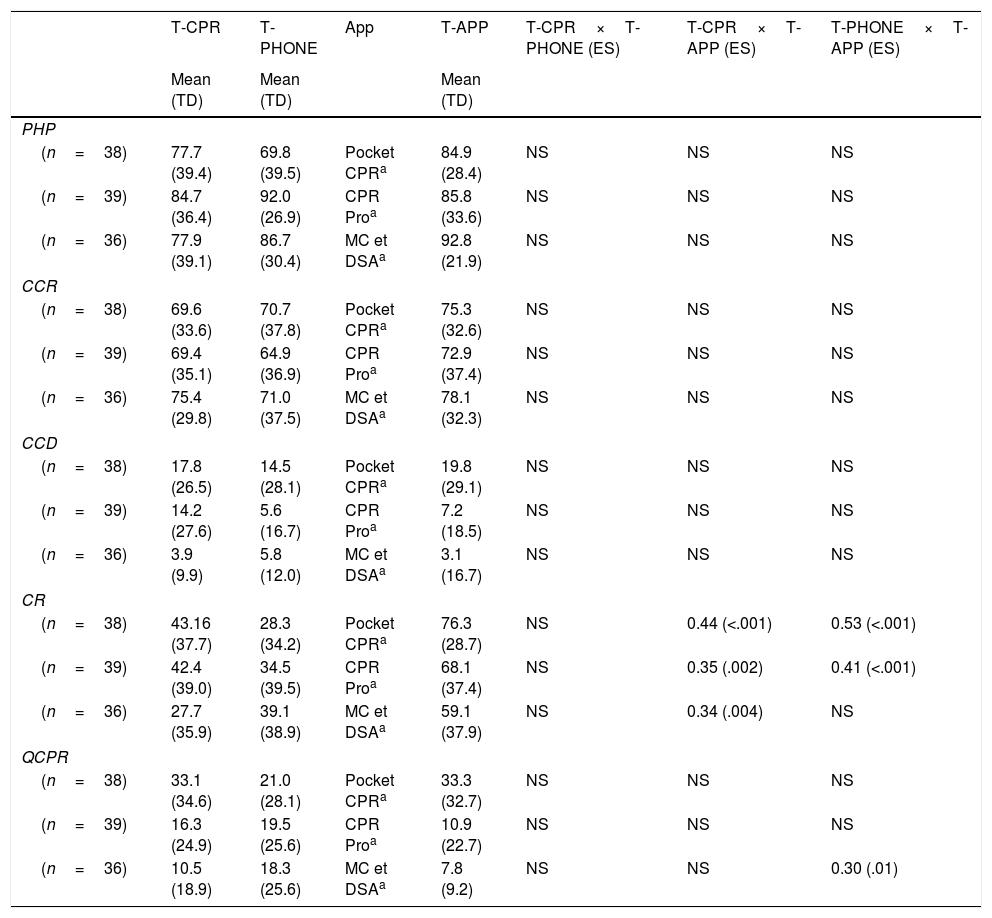
Data regarding the CPR tests run are shown in Tables 1 and 2.
Results of the variables showing means in the cardiopulmonary resuscitation (CPR) tests.
| T-CPR | T-PHONE | App | T-APP | T-CPR×T-PHONE (ES) | T-CPR×T-APP (ES) | T-PHONE×T-APP (ES) | |
|---|---|---|---|---|---|---|---|
| Mean (TD) | Mean (TD) | Mean (TD) | |||||
| AD | |||||||
| (n=38) | 36.8 (12.1) | 37.2 (11.9) | Pocket CPRa | 39.3 (9.8) | NS | NS | NS |
| (n=39) | 35.2 (12.1) | 34.0 (12.8) | CPR Prob | 29.8 (12.1) | NS | 0.34 (.003) | 0.35 (.002) |
| (n=36) | 30.8 (11.2) | 33.4 (10.0) | MC et DSAa | 29.2 (9.3) | NS | NS | 0.45 (.01) |
| AR | |||||||
| (n=38) | 115.4 (19.5) | 114.3 (21.2) | Pocket CPRb | 111.0 (8.8) | NS | NS | NS |
| (n=39) | 123.4 (24.6) | 124.1 (22.7) | CPR Prob | 113.7 (13.7) | NS | 0.30 (.01) | 0.35 (.002) |
| (n=36) | 118.7 (23.5) | 114.1 (19.7) | MC et DSAb | 109.0 (20.2) | NS | NS | NS |
AD, average depth, in millimeters; AR, average rhythm, measured in compressions per minute; NS, non-significant; TD, typical deviation; T-APP, CPR test with a hand-held smartphone plus an active app; T-CPR, CPR test without device; T-PHONE, CPR test with a hand-held turned-off smartphone.
Results of percentage variables in the cardiopulmonary resuscitation (CPR) tests.
| T-CPR | T-PHONE | App | T-APP | T-CPR×T-PHONE (ES) | T-CPR×T-APP (ES) | T-PHONE×T-APP (ES) | |
|---|---|---|---|---|---|---|---|
| Mean (TD) | Mean (TD) | Mean (TD) | |||||
| PHP | |||||||
| (n=38) | 77.7 (39.4) | 69.8 (39.5) | Pocket CPRa | 84.9 (28.4) | NS | NS | NS |
| (n=39) | 84.7 (36.4) | 92.0 (26.9) | CPR Proa | 85.8 (33.6) | NS | NS | NS |
| (n=36) | 77.9 (39.1) | 86.7 (30.4) | MC et DSAa | 92.8 (21.9) | NS | NS | NS |
| CCR | |||||||
| (n=38) | 69.6 (33.6) | 70.7 (37.8) | Pocket CPRa | 75.3 (32.6) | NS | NS | NS |
| (n=39) | 69.4 (35.1) | 64.9 (36.9) | CPR Proa | 72.9 (37.4) | NS | NS | NS |
| (n=36) | 75.4 (29.8) | 71.0 (37.5) | MC et DSAa | 78.1 (32.3) | NS | NS | NS |
| CCD | |||||||
| (n=38) | 17.8 (26.5) | 14.5 (28.1) | Pocket CPRa | 19.8 (29.1) | NS | NS | NS |
| (n=39) | 14.2 (27.6) | 5.6 (16.7) | CPR Proa | 7.2 (18.5) | NS | NS | NS |
| (n=36) | 3.9 (9.9) | 5.8 (12.0) | MC et DSAa | 3.1 (16.7) | NS | NS | NS |
| CR | |||||||
| (n=38) | 43.16 (37.7) | 28.3 (34.2) | Pocket CPRa | 76.3 (28.7) | NS | 0.44 (<.001) | 0.53 (<.001) |
| (n=39) | 42.4 (39.0) | 34.5 (39.5) | CPR Proa | 68.1 (37.4) | NS | 0.35 (.002) | 0.41 (<.001) |
| (n=36) | 27.7 (35.9) | 39.1 (38.9) | MC et DSAa | 59.1 (37.9) | NS | 0.34 (.004) | NS |
| QCPR | |||||||
| (n=38) | 33.1 (34.6) | 21.0 (28.1) | Pocket CPRa | 33.3 (32.7) | NS | NS | NS |
| (n=39) | 16.3 (24.9) | 19.5 (25.6) | CPR Proa | 10.9 (22.7) | NS | NS | NS |
| (n=36) | 10.5 (18.9) | 18.3 (25.6) | MC et DSAa | 7.8 (9.2) | NS | NS | 0.30 (.01) |
CCR, compressions with correct re-expansion, in percentage; CR, correct rhythm during the test, in percentage; NS, non-significant; PHP, compressions in proper hand placement, in percentage; QCPR, quality of the CPR, in percentage; TD, typical deviation; T-APP, CPR test with a hand-held smartphone plus an active app; T-CPR, CPR test without device; T-PHONE, CPR test with a hand-held turned-off smartphone.
Analyzing the absolute values according to the ERC recommendations14 (Table 1) for the AD variable we found significantly lower values when using the CPR Pro and MC et DSA apps compared to the T-PHONE app with a small effect size (0.35 and 0.45, respectively). The CPR Pro app also showed significantly lower values compared to the T-CPR app with a small effect size (0.34).
When the AR value was analyzed, the Pocket CPR and MC et DSA groups kept the mean AR within the ERC recommendations in the 3 tests run (no significant differences were found). However, in the CPR Pro group where the T-CPR and T-PHONE apps did not follow the ERC recommendations, significant differences were found when the T-APP was run (0.30 vs T-CPR and 0.35 vs T-PHONE) showing an average value within the recommendations (113.7 compressions per minute).
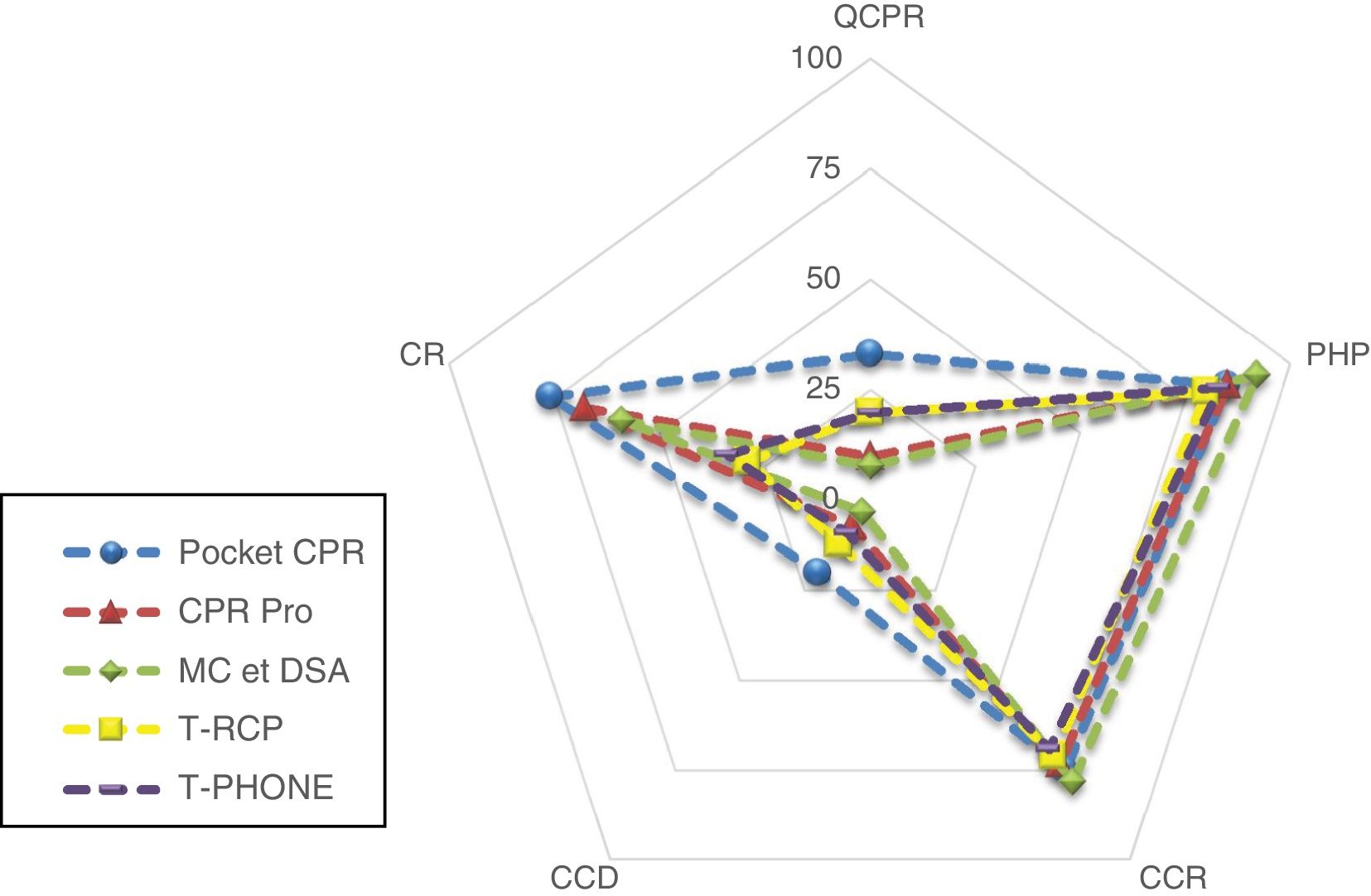
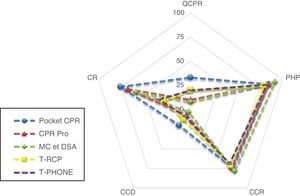
In the analysis of the CPR percent values (Table 2 and Fig. 3) we saw that in the PHP, CCR, and CCD variables none of the apps used showed significant improvements or worsening compared to the T-CPR and T-PHONE apps (P>.017).
Comparative chart of CPR percentages.
CCD, correct chest compression depth; CCR, compressions with correct re-expansion, in percentage; CR, correct rhythm during the test, in percentage; PHP, compressions with proper hand placement, in percentage; QCPR, quality CPR, in percentage; T-APP, CPR test with a hand-held smartphone plus an active APP; T-CPR, CPR test without device; T-PHONE, CPR test with a hand-held turned-off smartphone.
Regarding the CR variable that shows the percentage of compressions at rhythms of between 100 and 120 compressions per minute, significantly greater differences were seen when the T-APP was compared to the T-CPR. These were the effect sizes of using the different apps: Pocket CPR: 0.44; CPR Pro: 0.35; MC et DSA: 0.34.
Also, in the Pocket CPR and CPR Pro apps significantly higher percentages were seen when compared to the T-PHONE test being the effect size 0.53 in the first case and 0.41 in the second.
When we analyzed the overall quality of the CPR expressed in the QPCR variable, the values obtained were always <34% in all the tests. None of the apps showed statistically significant improvements and there was a significant reduction of quality when the MC et DSA app was compared to the T-PHONE test.
DiscussionOur study investigated the effectiveness of chest compressions by comparing 3 apps (T-APP): Pocket CPR®, CPR Pro®, and MC et DSA® with CPR without device (T-CPR) and CPR with turned-off smartphone (T-PHONE). The study subjects did not improve their results with the app-guided CPR. Actually, in some cases the results were worse.
This study is the result of numerous investigations conducted by inexperienced people and expert professionals healthcare providers on CPR techniques with feedback and improvement of resuscitation quality.12,21–24 Several studies confirm that there are different devices available capable of providing feedback and improving the quality of chest compressions, especially rhythm and depth when used by people trained in CPR techniques.25,26 The students who participated in this research had no previous training and their first contact with CPR was to become familiar with the app before running the tests. Inexperience with these platforms can be an important limiting factor as it happens in studies with lifeguards who ventilate better using mouth-to-mouth techniques than the resuscitative endovascular balloon27 or studies on intubations that show better results in the absence of intubations.28 Without proper knowledge, training or experience the mechanisms designed to improve the CPR may just not work.
CPR feedback devices should be used only if there is statistical proof of their validity and reliability as a measuring tool.29 In this sense, following the recommendations established by the US Food and Drug Administration30 medical apps need to be regulated to guarantee their validity and reliability. The apps used in our study did not improve the depth of compressions because resuscitators were inexperienced, the app was not accurate enough or because performing CPR maneuvers while holding a smartphone is uncomfortable. However, there are other hands-free devices available today that can be an alternative.31
Although there are several apps to practice resuscitation maneuvers, not all stick to the recommendations established by scientific societies or have tested their precision and usability.32 For this reason, the quality of resuscitation can vary depending on the feedback device used.33 In this sense, the study conducted by Park et al.34 assessed the use of the Pocket CPR app by placing the smartphone in 3 different positions (hand-held, with a hand-band, and with an armband). In any of the 3 cases, the measurements of chest compression depth recorded were not valid for any of the 3 body locations and the error was attributed to the system providing the information: the accelerometer.
In our study, the apps managed to keep the frequency of compressions in significantly higher values compared to other tests. We confirmed that the feedback device-guided CPR improved the rhythm of compressions.35,36 However, simple elements like LED devices or metronomes can improve this variable35 without having to keep the hands busy holding a mobile device. Compression depth was insufficient in all the tests run even with the use of the apps. Not reaching the necessary depth is a concurrent factor in numerous studies conducted with inexperienced people.37 Several causes can be the reason for this: training, experience or inaccurate feedback.
Mobile apps have revolutionized many aspects of CPR learning8 or the activation of witnesses close to the incident prompting more CPR maneuvers being performed by the witnesses.10 However, the use of apps as a support tool while performing quality CPR maneuvers still needs to be studied and complemented with more evidence.
Study limitationsThis sample included nursing students who, although had no specific training, may have had motivations that are different from other populations on the use of CPR. This study used manikins and the results cannot be generalized to the routine clinical practice. The results of the use of an app on a real victim or an actual scenario can generate different data. All participants used the same smartphone, which can also be a limiting factor, since not all phones have the same size or the same performance; therefore, the findings should be interpreted with caution. The lack of technical training on how to hold the smartphone or the inexperience of the subjects can be another limiting factor.
ConclusionIn light of the results of this sham study on the sample studied, smartphone-mounted app-guided CPR techniques did not improve the results of compressions during resuscitation. The only variable that improved using the apps was the percentage of compressions performed at a correct rhythm. The average compression depth seems the most limiting factor to be able to make quality compressions regardless of the type of test or app used. More studies are needed to learn more on the use of mobile apps as feedback providing tools when performing CPR maneuvers.
FundingThe authors declared that they did not receive any funding to conduct this study.
Author contributionFelipe Fernández-Méndez: study design and idea, data mining, analysis and interpretation of data; paper draft, and critical review.
Roberto Barcala-Furelos: study design and idea, analysis and interpretation of data, and critical review.
Martín Otero-Agra: study design and idea, data mining, analysis and interpretation of data, and critical review.
María Fernández-Méndez: study design and idea, data mining, analysis and interpretation of data, and critical review.
Myriam Santos-Folgar: study design and idea, data mining, analysis and interpretation of data, and critical review.
Antonio Rodríguez-Núñez: study design and idea, analysis and interpretation of data, and critical review.
All the authors approved the final version of this manuscript.
Conflicts of interestDr. Roberto Barcala-Furelos has participated in the development of an educational CPR app (CPR coach®) that was not tested or mentioned in this study. The authors declared no conflicts of interest whatsoever.
Please cite this article as: Fernández-Méndez F, Barcala-Furelos R, Otero-Agra M, Fernández-Méndez M, Santos-Folgar M, Rodríguez-Núñez A. Evaluación sobre la técnica de compresiones torácicas usando APP. ¿Ayudan o entorpecen la reanimación cardiopulmonar? Med Intensiva. 2020;44:72–79.