According to epidemiological data, critical care is needed by 5% of COVID-19 patients.1 Patients requiring ICU admission exceeded the total capacity of many hospitals, posing national healthcare systems at risk. An impressive effort from ICU teams managed to multiply their capacity by two or three-fold, trying to cover the continuous need for ICU beds.2,3
We report adult ICU admissions related to COVID-19 at a polyvalent ICU of a second-level hospital, with eight beds available in summer, and 10 in winter (0.47–0.59 ICU beds/10,000 inhabitants). Our goals included to analyse patients’ characteristics, identify factors associated with mortality, and share our experience regarding the organisational changes that were made in an environment of care-providing under pressure.
We performed a retrospective study with nasal/throat swabs or bronchial aspirate positive for SARS-CoV-2 by polymerase chain reaction (PCR) hospitalised between March 5th and May 7th, 2020. Patients transferred to other centres, and those still in ICU were excluded. Treatment adhered to current national protocols. The local IRB approved the study. We analysed clinical characteristics and performed a logistic regression multivariate analysis, including all variables to check the causes and associated factors of ICU mortality. We report numbers (percentages) for binary/categorical variables and medians (interquartile ranges) for continuous variables. Statistical analyses were performed using SPSS 20.0.
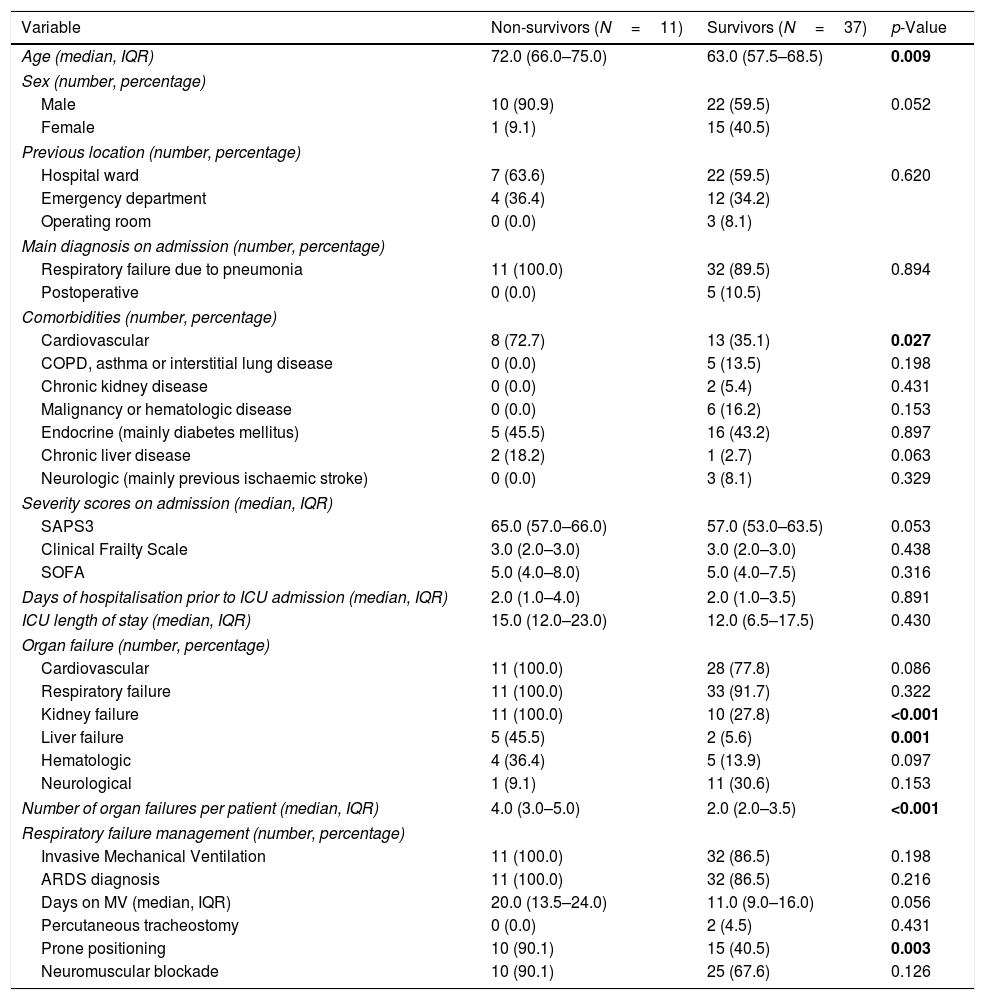
During the aforementioned period, 54 patients presented a positive PCR. Forty-eight patients were finally included (excluding six patients remaining in ICU). The median age was 65 years (IQR 59–72). 65.3% were men. 73.5% of the patients had associated comorbidity. The main diagnosis on admission was respiratory failure due to pneumonia (87.8%). Table 1 depicts the characteristics of the included patients. 77.1% of the patients survived upon ICU discharge. Non-survivors were older, presented a significantly higher rate of cardiovascular comorbidities, a higher number of organ failures (especially relevant regarding liver and kidney failure), and an increased need in prone positioning during ICU stay.
Demographics.
| Variable | Non-survivors (N=11) | Survivors (N=37) | p-Value |
|---|---|---|---|
| Age (median, IQR) | 72.0 (66.0–75.0) | 63.0 (57.5–68.5) | 0.009 |
| Sex (number, percentage) | |||
| Male | 10 (90.9) | 22 (59.5) | 0.052 |
| Female | 1 (9.1) | 15 (40.5) | |
| Previous location (number, percentage) | |||
| Hospital ward | 7 (63.6) | 22 (59.5) | 0.620 |
| Emergency department | 4 (36.4) | 12 (34.2) | |
| Operating room | 0 (0.0) | 3 (8.1) | |
| Main diagnosis on admission (number, percentage) | |||
| Respiratory failure due to pneumonia | 11 (100.0) | 32 (89.5) | 0.894 |
| Postoperative | 0 (0.0) | 5 (10.5) | |
| Comorbidities (number, percentage) | |||
| Cardiovascular | 8 (72.7) | 13 (35.1) | 0.027 |
| COPD, asthma or interstitial lung disease | 0 (0.0) | 5 (13.5) | 0.198 |
| Chronic kidney disease | 0 (0.0) | 2 (5.4) | 0.431 |
| Malignancy or hematologic disease | 0 (0.0) | 6 (16.2) | 0.153 |
| Endocrine (mainly diabetes mellitus) | 5 (45.5) | 16 (43.2) | 0.897 |
| Chronic liver disease | 2 (18.2) | 1 (2.7) | 0.063 |
| Neurologic (mainly previous ischaemic stroke) | 0 (0.0) | 3 (8.1) | 0.329 |
| Severity scores on admission (median, IQR) | |||
| SAPS3 | 65.0 (57.0–66.0) | 57.0 (53.0–63.5) | 0.053 |
| Clinical Frailty Scale | 3.0 (2.0–3.0) | 3.0 (2.0–3.0) | 0.438 |
| SOFA | 5.0 (4.0–8.0) | 5.0 (4.0–7.5) | 0.316 |
| Days of hospitalisation prior to ICU admission (median, IQR) | 2.0 (1.0–4.0) | 2.0 (1.0–3.5) | 0.891 |
| ICU length of stay (median, IQR) | 15.0 (12.0–23.0) | 12.0 (6.5–17.5) | 0.430 |
| Organ failure (number, percentage) | |||
| Cardiovascular | 11 (100.0) | 28 (77.8) | 0.086 |
| Respiratory failure | 11 (100.0) | 33 (91.7) | 0.322 |
| Kidney failure | 11 (100.0) | 10 (27.8) | <0.001 |
| Liver failure | 5 (45.5) | 2 (5.6) | 0.001 |
| Hematologic | 4 (36.4) | 5 (13.9) | 0.097 |
| Neurological | 1 (9.1) | 11 (30.6) | 0.153 |
| Number of organ failures per patient (median, IQR) | 4.0 (3.0–5.0) | 2.0 (2.0–3.5) | <0.001 |
| Respiratory failure management (number, percentage) | |||
| Invasive Mechanical Ventilation | 11 (100.0) | 32 (86.5) | 0.198 |
| ARDS diagnosis | 11 (100.0) | 32 (86.5) | 0.216 |
| Days on MV (median, IQR) | 20.0 (13.5–24.0) | 11.0 (9.0–16.0) | 0.056 |
| Percutaneous tracheostomy | 0 (0.0) | 2 (4.5) | 0.431 |
| Prone positioning | 10 (90.1) | 15 (40.5) | 0.003 |
| Neuromuscular blockade | 10 (90.1) | 25 (67.6) | 0.126 |
ARDS: acute respiratory distress syndrome. COPD: chronic obstructive pulmonary disease. CRRT: continuous renal replacement therapy. IQR: interquartile range. MV: mechanical ventilation. SAPS: Simplified Acute Physiology Score. SOFA: Sequential Organ Failure Assessment.
We would like to highlight that patients included had a 22.4% mortality during ICU admission. In our cohort, mortality was significantly associated with cardiovascular comorbidities and a higher number of associated organ failures. It should be noted that the published mortality rate is extremely variable, ranging from was 88% for patients who received mechanical ventilation4 to a reported 26% in an Italian study.5 Regarding management of respiratory failure and compared to other published studies,6 we observed a higher percentage of invasive mechanical ventilation therapy, with a lower prone rate and a similar use of neuromuscular blockade. Though our initial database was not designed to analyse the effect of the applied treatments, we intend to carry out an analysis in the future that will include it.
These encouraging data have been possible after multiplying our capacity by four and achieving a ratio of 1.8 ICU beds/10,000 inhabitants, reaching a peak of 30 critical patients admitted at the same time, with a maximum of 27 patients under mechanical ventilation on the same day. These results are thanks to an all-around strategy, based on our stable model of “ICU without walls”,7 multidisciplinary collaboration (enabling operating rooms, Major Outpatient Surgery, Reanimation and Emergency Department), maintenance of our protective mechanical ventilation protocol (personalised adjustment of PEEP using, whenever possible, electric impedance tomography), and reinforcement of our follow-up protocol after ICU discharge.
The COVID-19 pandemic has demonstrated the need for quick and innovative response mechanisms. New protocols should cover the growing demands while trying to maintain adequate care for our patients. The challenge remains.
Ethics approval and consent to participateStudy was approved by local Research Ethics Committee. Data was anonymized at the time of inclusion in the study.
Authors’ contributionsBLV and MMGA wrote and prepared the manuscript. DVD performed statistical analysis. RBP and FG supervised and approved the final version of the manuscript.
Conflict of interestAuthors admit no competing interests regarding publication of this manuscript.